A 70-year-old male patient underwent his first upper endoscopy for anemia work-up. Beyond a 3-cm hiatal hernia, an endoscopic diagnosis of Barrett’s esophagus (Prague classification C3M4) was entertained, as illustrated by a tongue at 3 o’clock on blue laser imaging (Fig. 1a). However, at the gastroesophageal junction an estimated 20-mm nodular, superficially ulcerated lesion emerged (Fig. 1b), likewise visualized on linked color imaging (LCI) after intra-hernial retroflexion (Fig. 1c). Giv en this presumed malignant complication, full-scale assessment of the Barrett’s esophagus was warranted, including acetic acid spraying. In combination with LCI, another 8-mm utterly flat lesion emerged at 6 o’clock with an irregular vessel and surface pattern, highly suggestive of early cancer as a second lesion (Fig. 1d). Pathology of endoscopic biopsies confirmed specialized intestinal metaplasia and, more intriguingly, indicated a well-differentiated adenocarcinoma (AC) for the flat lesion (Fig. 2a) and a poorly differentiated squamous cell carcinoma (SCC) for the nodular lesion (Fig. 2b). Cross-sectional and EUS staging indicated T1/2N+ stage. Notwith-standing, due to advanced chronic obstructive pulmonary disease (GOLD IIIB with long-term oxygen therapy), the patient underwent upfront esophagectomy without significant complications after pulmonary prehabilitation. Final surgical pathology indicated pT1a, pN0(0/27), G1 for the AC and pT1b, pN1(2/27), G3 for the SCC (furthermore: L0, V0, Pn0, R0 each).
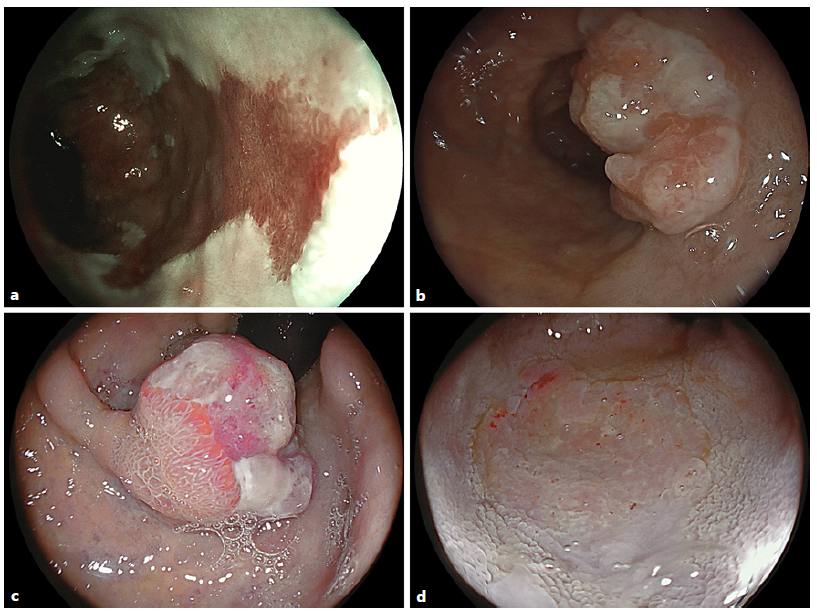
Fig. 1 a Blue laser imaging of a Prague C3M4 Barrett’s esophagus with a tongue highlighted at 3 o’clock. b An estimated 20-mm nodular ulcerated lesion emerged at the gastroesophageal junction (c) as replicated on retroflexed LCI visualization. d LCI after acetic acid spraying in the distal esophagus highlighted another 8-mm flat lesion with an irregular vessel and surface pattern consistent with early cancer.
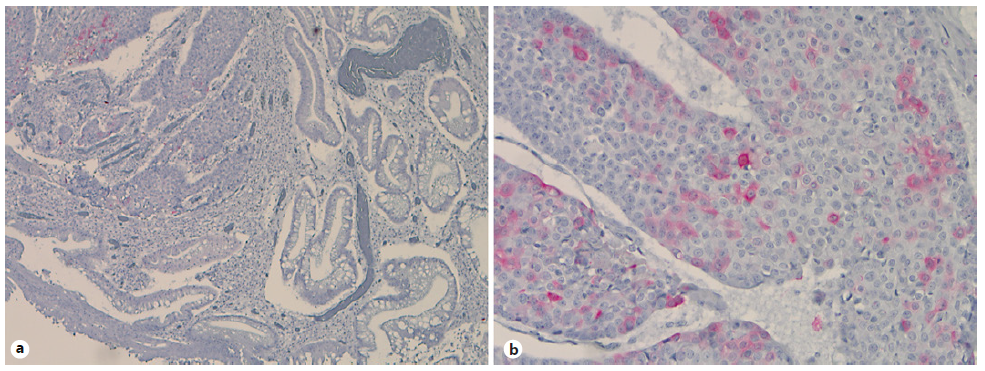
Fig. 2 Immunohistochemistries for cytokeratin (CK) 5/6 with negative staining of the AC (a) and positive results in the SCC (b).
Barrett´s esophagus is a well-acknowledged risk factor for esophageal AC formation; however, singular cases of SCC arising in Barrett’s esophagus and/or collision tumor comprising SCC and AC elements have been documented in the literature, pointing to ambivalent carcinogenic field effects [1-3]. Concurrent SCC and Barrett’s carcinoma has occasionally been reported in Barrett’s esophagus before, however, to the best of our knowledge, not with the Barrett’s segment itself [4-6]. Of interest, the patient had a mixed risk profile, including obesity and metabolic syndrome (Barrett’s) and heavy smoking (SCC). The distinct molecular mechanisms for a presumed field cancerization within a Barrett’s esophagus, which has been discussed in the literature, however, remain elusive.














