A 22-year-old female, who had underwent Fontan procedure in childhood, presented with mild elevation of liver enzymes (AST 35 U/L, ALT 50 U/L, ALP 62 U/L, GGT 61 U/L). She had no liver dysfunction (total bilirubin 1.3 mg/dL, INR 1.1, albumin 3.7 g/dL), signs of cirrhosis or portal hypertension (platelets 177 × 109), encephalopathy or ascites.
Viral, autoimmune, metabolic, and toxic etiologies were excluded. Abdominal ultrasound showed a diffusely heterogeneous and micronodular liver parenchyma, compatible with Fontan-associated liver disease (FALD) in this context. Moreover, multiple de novo hyperechogenic nodules were found, imposing investigation.
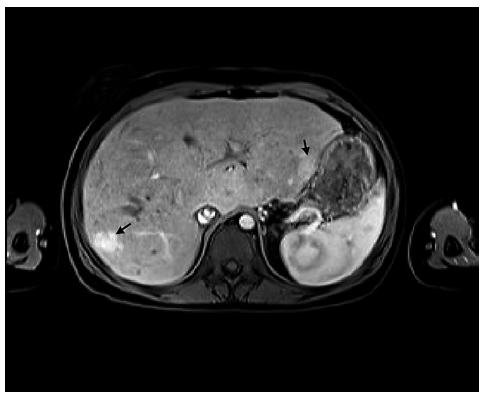
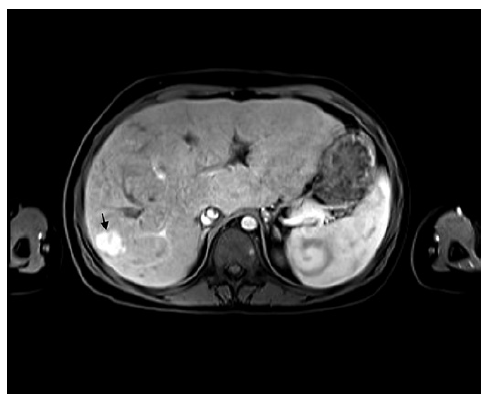
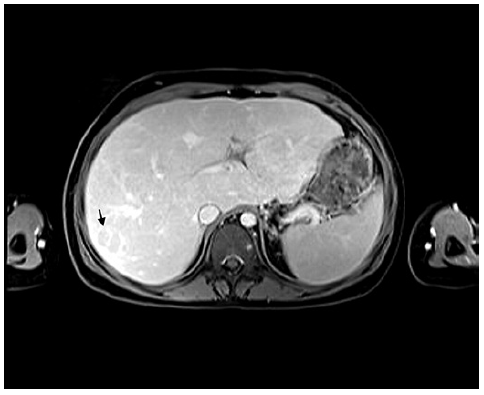
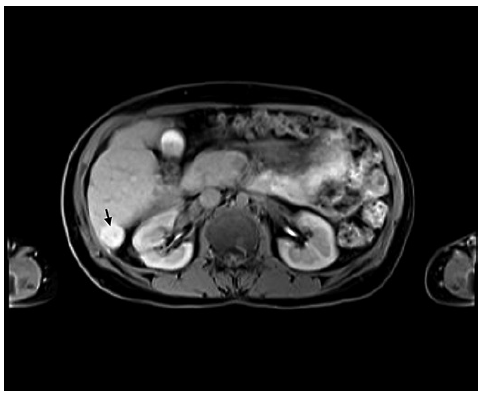
MRI reported >12 nodules, maximum diameter of 27 mm, isointense in T1-weighted sequences, hypointense in T2, with no restricted diffusion (shown in Fig. 1). Some were halosurrounded, while others displayed a central scar. Most displayed hyperenhancement in the hepatic arterial phase (shown in Fig. 2), becoming isointense in the portal phase and hypointense in the delayed one, a worrisome feature known as washout (shown in Fig. 3). Using hepatobiliary contrast, all nodules showed hyper-intensity (shown in Fig. 4). Bloodwork revealed normal alphafetoprotein (AFP). Therefore, the final diagnosis of multiple focal nodular hyperplasia (FNH)-like in a FALD background was made, and the patient kept under sur-veillance.
The Fontan procedure is a palliative surgery for patients with an anatomic or functional single-ventricular congenital heart disease, consisting of a total extra-cardiac cavopulmonary connection created by anastomosing the superior vena cava to the right pulmonary artery (PA) and insertion of an extracardiac conduit between the inferior vena cava and the PA [1, 2]. The consequent chronic liver congestion and ischemia result in FALD, leading to cirrhosis in 1-5% of patients per year and hepatocellular carcinoma (HCC) in 1.3% [1-3]. Indeed, annual and early liver surveillance is mandatory [1].
Multiple FNH is a rare entity which has been associated with some vascular diseases and treatments [4, 5]. This clinical case highlights an association between multiple FNH and FALD. Given the inherent risk of HCC in FALD and similar MRI findings between FNH and HCC in this background, their differential diagnosis becomes challenging [1, 2]. In this context, AFP and MRI hepatobiliary contrast are key [2, 3]. Nonetheless, biopsy should be considered in dubious and atypical nodules [1].