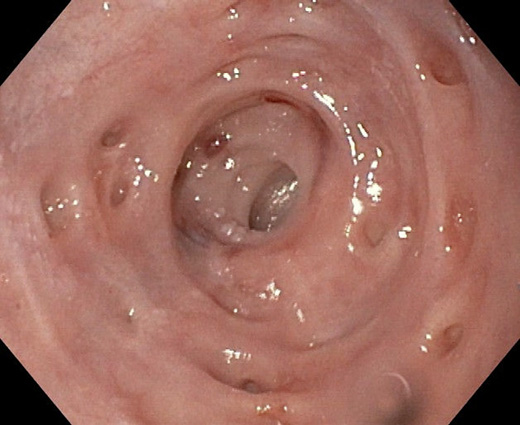
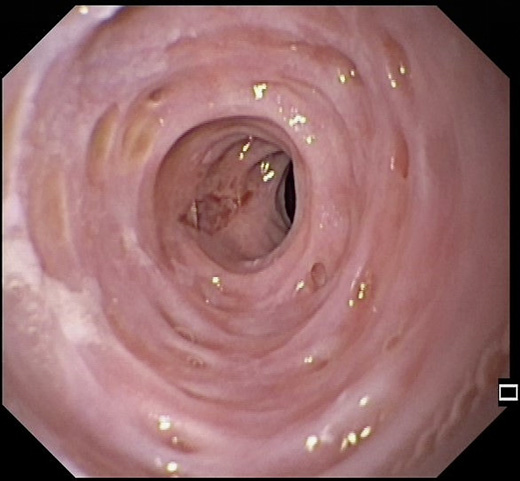
A 54-year-old male was referred to a gastroenter-ology appointment with a 15-year history of dysphagia. He had a medical history of metastatic lung adenocarcinoma and is currently under pembrolizumab treatment. He was an active smoker (63 pack-years) and drank 10 alcohol units a day. He presented with progressive dysphagia to solids and, in the last 4 years, intermittent for liquids, with progressive weight loss (10% of body weight loss in the past 6 months) with a body mass index of 16.8 kg/m2.Hewas previously assessed in different hospitals and performed numerous exams, including upper endoscopy showing a sloughing esophageal mucosa with signs of candida infection and narrowing of the distal esophagus. Histopathology was compatible with esophageal candidiasis with unspecificchronicinflammation. He underwent several endoscopic dilations, the last one roughly 12 years before, with later symptom recurrence and was lost to follow-up. An upper endoscopy performed in our center displayed esophageal pseudodiverticulosis (EP) with distal strictures with underlying regular mucosa that were not transposable by the endoscope (Fig. 1). Esophageal biopsies excluded eosinophilic esophagitis. The patient was advised for lifestyle changes, including smoking cessation and alcohol abstinence. He underwent endoscopic dilation of two distal esophageal strictures using a through-the-scope balloon, with prior intralesional steroid injection (2 mg of dexamethasone into each quadrant), up to 15 mm diameter (shown in Fig. 2), with initial dysphagia improvement and weight gain. Afterward, a proton pump inhibitor was initiated in order to reduce stricture recurrence. At 3-month follow-up, the patient had symptom relapse, namely, dysphagia for solids, and was proposed to an additional endoscopic dilation.
EP is a rare condition characterized by multiple out-pouching lesions of the esophageal wall, representing dilated ducts of submucosal glands [1]. Inflammation and increased intramural pressure are thought to be the main mechanisms behind these false diverticula [2]. Dis-tribution can be segmental or diffuse [2]. Etiology is still unclear, but tobacco smoking and alcohol consumption appear to be risk factors [1, 3]. Other associations include candida infection, caustic ingestion, gastroesophageal reflux disease, or diabetes mellitus [1, 2]. The most typical symptom is chronic dysphagia, which can be constant, intermittent, or progressive, classically for solids, and can persist for years [2, 3]. This symptom is usually associated with other conditions, such as esophageal stricture or candidiasis, rather than attributable to the EP [1, 2]. In the present case, a distal stenosis causing an increased intraluminal pressure is a possible mechanism for this endoscopic finding, as the outpouchings were not previously described and appeared over the course of a long-standing stricture. Endoscopy is significant for excluding coexisting disorders, especially in a patient presenting with dysphagia; however, barium studies are more sensible in diagnosing EP [2, 4]. Treatment is mainly supportive and should be directed at the underlying condition, with elimination of risk factors and control of associated comorbidities [1, 2]. In the presence of an esophageal stricture, dilation has been reported to be an effective and safe procedure, providing symptomatic improvement, with up to 57% requiring multiple procedures [2, 4].