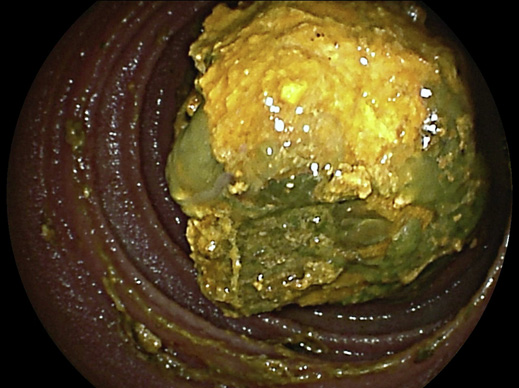
We present the case of a 67-year-old man with a medical history significant for orthotopic liver transplant 20 years earlier due to alcohol-related liver cirrhosis. The posttransplant period was complicated with posttransplant lymphoprolifer-ative disease, treated with adjustment of immunosuppressive therapy and systemic chemotherapy, and is currently on remission. This patient developed a biliary stenosis at the level of the biliary anastomosis (choledococholedocostomy), leading to secondary graft cirrhosis. Cross-sectional magnetic resonance cholangiopancreatography demonstrated the anastomotic stricture with a concomitant dilation of the distal common bile duct (native bile duct segment), with recurrent identification of large biliary stones in this dilated section. During the post-transplant follow-up period, he had multiple hospital admissions due to acute cholangitis (last episode in 2018), requiring multiple endoscopic retrograde cholangiopancreatographies for stone extraction. The patient presented to the emergency department with right upper quadrant pain, jaundice, and fever. Laboratory workup revealed elevated total bilirubin (10 mg/dL) and C-reactive protein (77 mg/L). An abdominal ultrasound was performed and revealed a discrete dilation of intrahepatic bile ducts. The patient was hospitalized under antibiotic therapy for acute cholangitis. Given the prior episodes of acute cholangitis and lithiasis and the current clinical presentation, the patient underwent an endoscopic retrograde cholangiopancreatography which showed no evidence of dilated intrahepatic bile ducts or biliary calculi but reported abundant gastric and duodenal stasis content. Over the following days, the patient developed recurrent biliary vomiting and abdominal distension, complicating with prerenal acute kidney injury and portosystemic hepatic encephalopathy. A contrast-enhanced abdominal computed tomography revealed dilation of the jejunal loops, with a maximum diameter of 40 mm, and the presence of obstructing endoluminal content (Fig. 1). Distal to this point, no dilation was evident. Due to his poor physical condition and underlying comorbidities, surgery was considered to carry an unacceptably high risk. A double-balloon enteroscopy (DBE) was performed revealing an impacted biliary stone with approximately 25 mm in the distal jejunum (Fig. 2). The stone was mobilized to the stomach using a polypectomy snare and ultimately removed using a retrieving basket (RothNet®,STERIS,Dublin,Ireland) (Fig.3).Thepatient had resolution of obstructive symptoms and resumed oral feeding with tolerance.

Fig. 1 Axial abdominal CT scan image showing endoluminal content within a jejunal loop (arrow) with upstream small bowel dilation. CT, computed tomography.
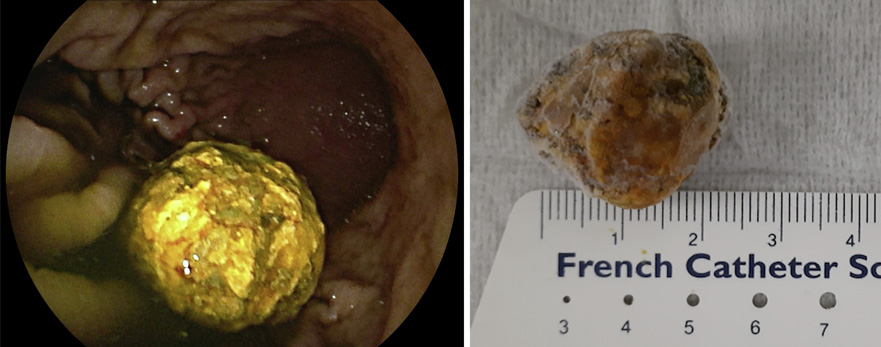
Fig. 3 a Gallstone from the stomach before being removed with a retrieving basket. b Subsequent measurement of the gallstone confirmed its estimated size of 25 mm (photo taken after the specimen had been several hours in a refrigerator for preservation).
Bowel obstruction is a rare late complication after liver transplantation, occurring in approximately in 1-2% of cases [1]. The most common etiologies include intra-abdominal adhesions and internal hernias [2]. Gallstone ileus is an uncommon etiology of mechanical small bowel obstruction, accounting for up to 4% of all cases, being more frequent in women [3]. Contrast-enhanced computed tomography is the gold standard for the diagnosis of this entity and can be of value for decision-making regarding the therapeutic strategy. To date, cases of gallstone ileus have scarcely been described in orthotopic liver transplant patients. Recently, 2 cases of gallstone ileus have been reported after liver transplantation [4, 5]. In both cases, the patients had been submitted to liver transplantation due to biliary atresia and had a bilioenteric anastomosis, favoring stone migration, and an altered gastrointestinal anatomy (Y-en-Roux jejunojejunostomy). Both cases were managed with enterotomy for stone extraction. Opposite to these reports, in this case, the patient did not have a bilioenteric anastomosis and was managed using an endoscopic technique. Indeed, the location of stone impaction combined with the accessibility to DBE allowed a safe and efficient stone extraction in a patient with a poor surgical condition.
The resolution of gallstone ileus most often requires aggressive fluid and electrolyte followed by early intervention to relieve bowel obstruction [3]. Surgical enterotomy remains the standard of care for stone extraction and resolution of bowel obstruction. Moreover, when the presence of a bilioenteric fistula is responsible for the passage of a large stone to the small bowel, surgery allows the closure of the defect [3]. The use of DBE for resolution of bowel obstruction has scarcely been reported. Nevertheless, DBE can be a valid alternative to the standard surgical approach in patients with a poor preoperative condition. Endoscopic treatment options include electrohydraulic and mechanical lithotripsy, as well as retrieving baskets [6, 7].