A 59-year-old woman who underwent radical mastectomy due to multifocal mixed invasive ductal and micropapillary breast carcinoma presented with a 3-month history of progressive dysphagia for solids. After surgery, she underwent adjuvant chemoradiotherapy and hormone therapy, without clinical or radiological signs of recurrence during an 18-year follow-up period.
Gastroscopy and computed tomography were unre-markable. The contrast esophagogram revealed a slight narrowing of the proximal esophagus (besides the physiological aortic arch compression), persistent throughout the examination, but with normal contrast progression. Due to the progressive dysphagia worsening, she was referred to gastroenterology.
Gastroscopy with peri-procedural fluoroscopy was repeated and showed a protruded yellowish area, between 25 and 27 cm from the incisors, suggestive of a sub-epithelial lesion or extrinsic compression (Fig. 1a, b). Fluoroscopic findings were similar to the previous evaluation (Fig. 1c). Endoscopic ultrasound (EUS) re-vealed a hypoechogenic lesion with well-defined contours and limits, measuring 15.8 × 7.8 mm, originating in the muscle layer and with intimal contact with the aortic arch, without local invasion (Fig. 1d, e). Despite resis-tance, the scope was able to traverse de stenosis. Then, an EUS-guided 19-gauge fine-needle biopsy (FNB) was performed.
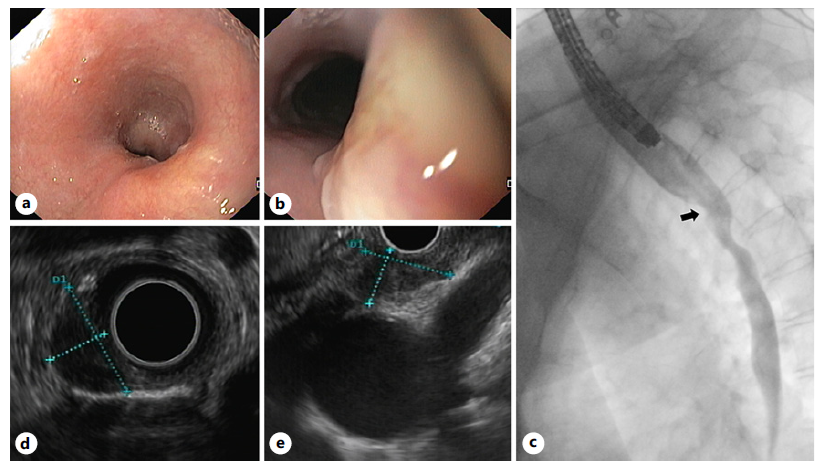
Fig. 1 a, b Endoscopic view of an elevated yellowish area covered with normal-appearing mucosa. c Normal contrast progression, despite the presence of a 15 mm narrowing of the proximal esophageal lumen (arrow). EUS revealed a hypoechogenic mass with well-defined contours and limits, centered in the muscle layer and with intimal contact with the aortic arch, maintaining the cleavage plane (d:radialprobe, e:linear probe).
Histopathological examination revealed nuclear overlapping and hyperchromatic aggregates of epithelial cells infiltrating the striated muscle. Strong nuclear staining of estrogen receptors was present in 100% of the neoplastic cells (Fig. 2 a, b). These findings were compatible with esophageal metastasis from breast cancer. Palliative treatment with letrozole and ribociclib was initiated, and the patient reported symptomatic improvement.
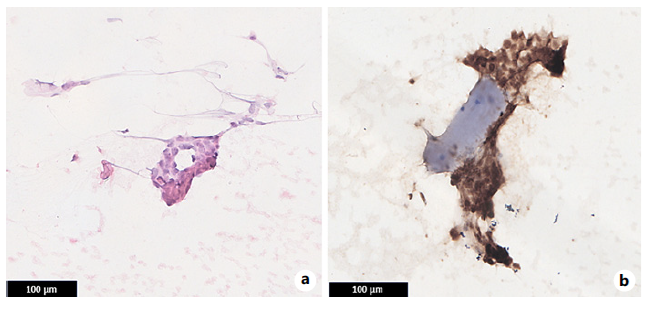
Fig. 2 a Nuclear overlapping and hyper-chromatic aggregates of epithelial cells. b Neoplastic cells showed strong nuclear staining of estrogen receptors and infiltrate the striated muscle.
Esophageal metastasis from breast cancer is rare, with a prevalence of 4.2-5.9% in autopsy studies, despite only 0.59% of patients having dysphagia [1]. A large case series (n = 2,246) reported a 0.4% prevalence of breast cancer esophageal metastases over an 18-year period [2]. The middle third of the esophagus is the most frequently affected site, probably due to the involvement of tracheobronchial lymph nodes and lymphatic drainage into the mediastinum [3]. The average time between the onset of dysphagia and diagnosisis 8 months.Diagnosis maybedifficult since esophageal metastatic lesions are almost always located below the mucosal plane, originating from the outside layers to inwards [4]. Thus, standard mucosal biopsy specimens are often not diagnostic. In turn, EUS-FNB can improve diagnostic accuracy [5]. When EUS-FNB is not feasible, mucosal-incision-assisted biopsy or single-incision needle-knife biopsy are valid alternatives. Diagnosis of esophageal metastasis from breast cancer is challenging and should be considered in every patient with a clinical history of this neoplasia, regardless of the follow-up period.





![Retraction Statement - Paper by Chee Yik Chang and Bryan Tan entitled “Splenic Abscess Caused by Clostridium difficile” [GE Port J Gastroenterol 2023; https://doi.org/10.1159/000533163]](/img/pt/next.gif)








