Clinical Case Study
Endoscopic Management of Dysfunctioning Gastric Band after Sleeve Gastrectomy with the Luso-Cor® Esophageal Stent
Resolução endoscópica de estenose pós gastrectomia vertical com anel de silicone - utilização de prótese esofágica Luso-Cor®
Filipe de Sousa Damião1
Patrícia Santos1
João Lopes1
João Raposo2
Carlos Noronha Ferreira1
3
Rui Marinho1
3
1Serviço de Gastrenterologia e Hepatologia, Centro Hospitalar Universitário Lisboa Norte, Lisboa, Portugal;
2Serviço de Cirurgia, Centro Hospitalar Universitário Lisboa Norte, Lisboa, Portugal;
3Clínica Universitária de Gastrenterologia, Faculdade de Medicina de Lisboa, Universidade de Lisboa, Lisboa, Portugal
Abstract
Sleeve gastrectomy (SG) can be aided by the addition of a calibration silicone ring, banded SG (BSG). It provides better weight loss than non-banded SG but with higher rate of adverse events. The aim of this case report is to further contribute to the knowledge of how to endoscopically manage these patients by placing a new esophageal stent (Luso-Cor®). A 58-year-old female with grade III obesity (weight 110 kg, BMI: 45.2 kg/m2) underwent SG in 2013. Due to the limited weight loss, a surgical calibration silicon ring was placed in 2017. In the following months, she developed recurrent and abundant postprandial regurgitation, achieving a minimum weight of 66 kg (BMI: 27.1 kg/m2). Gastroesophageal transit showed a stricture at the junction of the gastric corpus and antrum, causing gastric outlet obstruction. Endoscopy identified a regular luminal stenosis with normal mucosa, which allowed easy passage of the endoscope with slight pressure. Two sessions of endoscopic dilatation were performed, first with an 18-mm through-the-scope balloon and later with a 30-mm pneumatic balloon without symptomatic relief. A two-step endoscopic therapeutic approach was proposed to first promote intragastric ring erosion by placing a new partially covered metallic stent, Luso-Cor® esophageal stent 30/20/30 × 240 mm, and subsequently retrieve the stent, followed by cutting and retrieval of the ring. The proximal flare with a 30 mm diameter was placed in the distal esophagus and the distal edge in the prepyloric antrum. However, 2 weeks later , she complained of vomiting and abdominal fullness. Complete migration of the proximal flare of the stent into the remnant gastric fundus was seen on the contrast study. Endoscopy was performed, and the stent was easily removed. A blue calibration ring, partially eroded into the gastric lumen, was observed at the site of gastric tube stenosis. After stent removal, the patient was asymptomatic, and so conservative follow-up was decided. A follow-up endoscopy, performed 5 months later, showed complete reepithelization of the eroded ring. The patient remains asymptomatic after 3 years of follow-up and has regained weight up to 76 kg (BMI: 31.2 kg/m2). The efficacy of endoscopy on the management of ring-related adverse events has been previously reported. Small-case series describe the use of multiple pneumatic dilations or the deployment of plastic or covered metallic stents to cause erosion of the overlying mucosa, followed by cutting and retrieval of the ring. In conclusion, we believe that the mural pressure exerted by the Luso-Cor® esophageal stent, in the limited period it remained in situ, was sufficient to relieve the luminal pressure of the silicon ring, realigning the ring with the remnant gastric tube. This rare clinical entity highlights the potential role of specific metallic stents in the management of these patients.
Keywords: Banded sleeve gastrectomy; Gastric band migration; Bariatric surgery endoscopy; Gastric outlet obstruction; Endoscopic stenting
Resumo
A cirurgia bariátrica de gastrectomia vertical (sleeve gástrico) pode ser complementada pela adição de um anel restritivo de silicone - sleeve gástrico com anel de silastic. O acréscimo deste anel promove uma maior perda de peso, no entanto está associado a maior risco de eventos adversos. O objetivo da apresentação deste caso é contribuir para as diferentes técnicas úteis no tratamento das complicações relacionadas com o anel, através da utilização de uma prótese esofágica (Luso-Cor®). Uma doente de 58 anos, com obesidade grau III (peso 110 kg, IMC 45,2 kg/m2), foi submetida a um sleeve gástrico em 2013. Não apresentou perda de peso favorável e, em 2017, foi colocado um anel de silicone rodeando o tubo gástrico. Nos meses seguintes desenvolveu regurgitação pós-prandial recorrente e abundante, alcançando um peso mínimo de 66 kg (IMC 27,1 kg/m2). Realizou um trânsito gastroesofágico que revelou uma estenose na junção do corpo com o antro gástrico, com evidência de obstrução do esvaziamento gástrico. A endoscopia digestiva alta identificou uma estenose regular recoberta por mucosa sem lesões, com passagem do aparelho após pressão ligeira. Foram realizadas duas sessões de dilatação, inicialmente com balão trough-the-scope de 18 mm e posteriormente com balão pneumático de 30 mm. Os sintomas persistiram e, por esse motivo, foi decidido uma abordagem em dois tempos: primeiro promover a erosão intragástrica da banda para depois a seccionar e remover intraluminalmente. Nesse sentido, foi colocada uma prótese metálica esofágica parcialmente coberta, Luso-Cor® 30/20/30 × 240 mm. O segmento proximal da prótese com 30 mm de diâmetro foi colocado no esófago e o bordo distal da prótese ficou no antro pré-pilórico. No entanto, duas semanas depois, a doente queixou-se de vómitos e enfartamento precoce. O estudo radiográfico com contraste revelou migração distal da prótese, com deslocamento do segmento proximal para o corpo gástrico remanescente. A prótese foi removida endoscopicamente sem dificuldade e, na região da estenose, foi observado o anel de silicone parcialmente erosionado para o lúmen gástrico. Após remoção da prótese a doente evoluiu favoravelmente, sem novos sintomas, e, por esse motivo, foi decido seguimento sem novas intervenções. A endoscopia de seguimento, realizada cinco meses após, demonstrou reepitelização completa do anel parcial-mente erosionado. A doente permanece assintomática após três anos de seguimento e voltou a ganhar peso (peso atual 76 kg, IMC 31,2 kg/m2). A eficácia da resolução endoscópica de estenoses relacionadas com anel de silicone no sleeve gástrico já foi relatada. Pequenas séries de casos utilizaram múltiplas sessões de dilatação com balão pneumático ou colocação de próteses plásticas ou metálicas cobertas para promover erosão intragástrica do anel e sua remoção. Acreditamos que a pressão mural exercida pela prótese Luso-Cor®, no curto tempo em que permaneceu in situ, foi suficiente para aliviar a obstrução, realinhando o seu diâmetro com o restante tubo gástrico. Através do relato desta entidade clínica rara, esperamos contribuir para o conhecimento das próteses metálicas específicas para o manejo destes doentes.
Palavras Chave: Sleeve gástrico com anel de silastic; Migração de banda gástrica; Endoscopia na cirurgia bariátrica; Obstrução do esvaziamento gástrico; Próteses endoscópicas
Introduction
Band-assisted procedures have become one of the most common bariatric surgeries performed worldwide [1]. In sleeve gastrectomy (SG), if weight loss does not achieve the necessary metabolic goal, the surgical addition of a silicon ring to the gastric sleeve (banded SG [BSG]) further increases weight loss [2, 3]. However, it is essential to be aware of the specific band-related adverse events in this subgroup of patients, such as ring slippage and gastric outlet stenosis. Different methods for diagnosis and treatment have been reported [4-9]. The aim of the present case report is to further contribute to the knowledge of how to endoscopically manage these patients by the placement of a new esophageal stent (Luso-Cor®).
Case Report
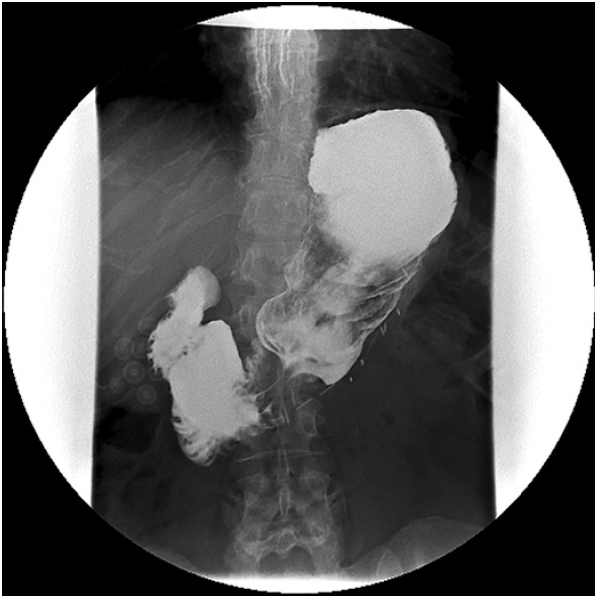
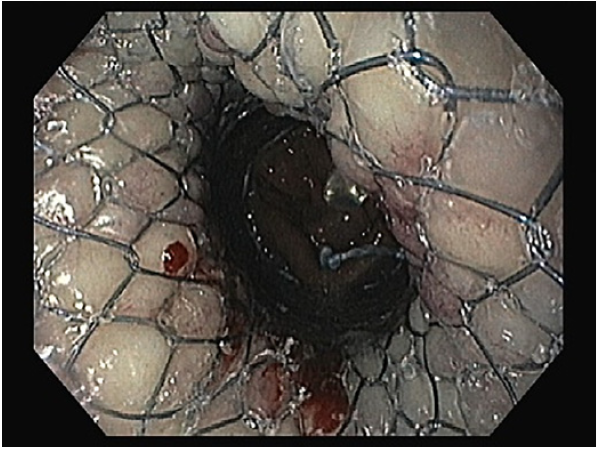
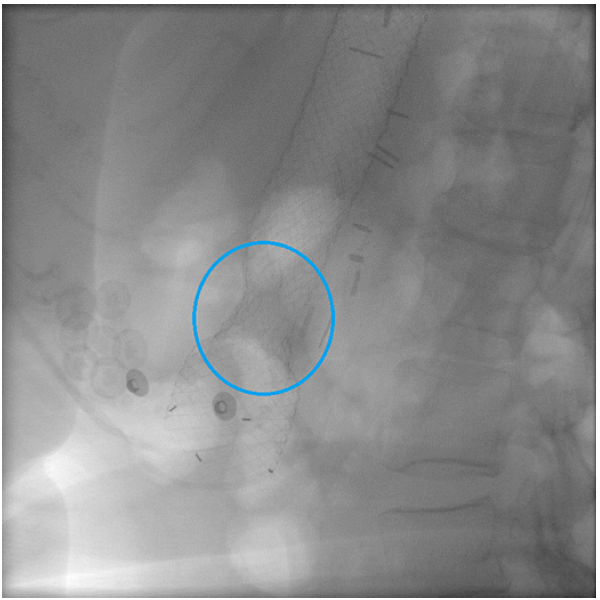
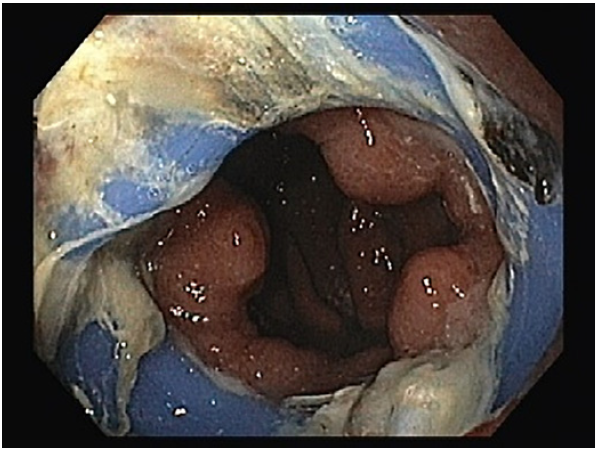
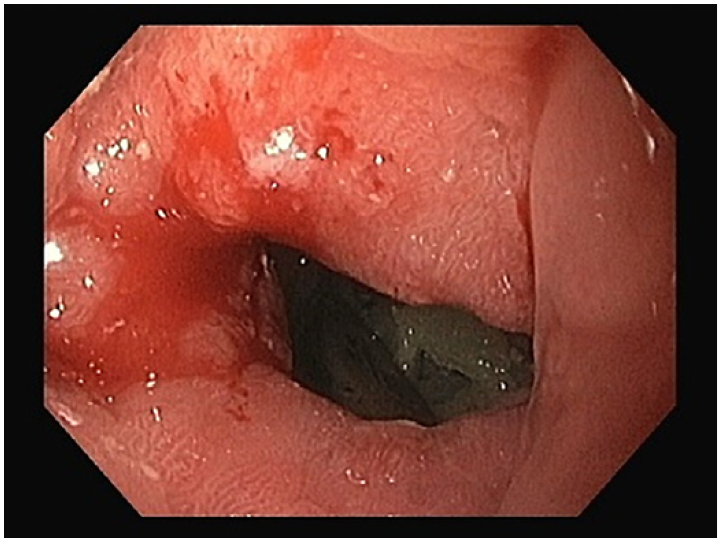
A 58-year-old female with grade III obesity (weight 110 kg, body mass index [BMI] 45.2 kg/m2) underwent SG in 2013. Due to the limited weight loss, a surgical calibration ring was placed in 2017. In the following months, she developed recurrent and abundant post-prandial regurgitation, achieving a minimum weight of 66 kg (BMI: 27.1 kg/m2). Gastroesophageal transit showed a stricture at the junction of the gastric corpus and antrum, causing gastric outlet obstruction (Fig. 1). An upper gastrointestinal endoscopy (UGIE) was performed and identified a regular luminal stenosis with normal mucosa, which allowed easy passage of the scope with slight pressure (Fig. 2). Two sessions of endoscopic dilatations were performed, first with an 18-mm through-the-scope balloon and later with a 30-mm pneumatic balloon, without symptomatic relief. A two-step approach was proposed: first to promote intragastric ring erosion by placing a specific partially covered metallic stent, the Luso-Cor esophageal 30/ 20/30 × 240 mm, and subsequently to cut and endoscopically retrieve thering. Theproximalflare of the stent measuring 30 mm in diameter, which includes a 5-mm uncovered portion, was placed in the distal esophagus and the distal edge in the prepyloric antrum (Fig. 3, 4). However, 2 weeks later, she complained of vomiting and abdominal fullness. Complete migration of the proximal flare into the remnant gastric fundus was seen in the oral contrast study. A new UGIE was performed and the stent was easily removed with a rat tooth forceps. The blue calibration silastic ring, partially eroded into the gastric lumen, was observed at the site of stenosis in the gastric tube (Fig. 5). The patient was discharged and she remained asymptomatic, so we therefore opted for conservative management. The first follow-up UGIE, performed 5 months after the metallic stent removal, showed complete reepithelization of the eroded ring (Fig. 6).
The last UGIE was performed after one and a half years of follow-up and showed gastric stenosis at the site of the ring, without scope passage obstruction. The patient remained asymptomatic after 3 years of follow-up and has regained weight up to 76 kg (BMI: 31.2 kg/m2).
Discussion
The main bariatric surgical procedures that utilize a silastic ring are banded Roux-en-Y, gastric lap-band, and BSG. Despite well-known metabolic results, several adverse events related to the ring or the band have been
described [4-10]. BSG is associated with a 4% incidence of ring-related adverse events, with stenosis of the gastric tube being the most common [3]. Unlike lap-band, in BSG, the ring is placed loosely around the gastric sleeve to prevent dilation; therefore, it does not permanently compress the gastric wall [3].
There are mainly four types of band dysfunction. Type Iisdefined by the slipping of the band, seen in the early stages after surgery. This type of malfunction is not an indication for endoscopic management. Type II ring dysfunction is represented by outlet stoma stenosis of the pouch, and this was what our patient developed. Band erosion of the gastric mucosa is defined as a type III dysfunction: minor erosion represented by type IIIa; major erosion, more than half of the band/ring circumference, represented by type IIIb [4]. Types II, IIIa, and IIIb can be identified later after surgery, and although classically managed by surgery, endoscopic approach has been reported to be safe and feasible [4-6].
Management of band dysfunction by endoscopic dilation has been reported by Campos et al. [6]. They published a series of 35 patients with gastric pouch outlet stenosis (type II dysfunction) due to ring slippage after gastric bypass. All patients were treated with multiple 30 mm pneumatic balloon dilations with a 100% efficacy rate. On average, patients required two sessions of endoscopic dilation. Adverse events occurred in 14.3% (n = 5) and included asymptomatic ring erosion in 11.4% (n = 4) and self-limited upper digestive tract hemorrhage in 2.8% (n =1). However, all the patients managed in this series had undergone gastric bypass surgery, while our patient underwent BSG. We attempted to relieve the mural ring compression with endoscopic dilatations with balloons with progressively bigger diameter without success.
Stent-induced intragastric band/ring erosion has been previously described with different types of stents [4, 7-9]. In all of the series, a two-step approach was advocated: with initial deployment of a metallic or plastic stent to progressively induce necrosis and intragastric erosion of the band and a subsequent endoscopy to cut and retrieve the eroded ring [4, 7-9].
One of the few published manuscripts related to metallic stents describes a series of 15 patients. Stents measuring 120-155 mm in length (fully and partially covered) were used. In the first half of the patients, two metal stents were placed, both 120 mm in length and 22-23 mm wide, with a goal of achieving at least 50 mm overlap, to increase circumferential pressure and avoid migration. On the second half, in an effort to avoid esophageal overlap, which seemed to cause pain in some patients, only a 120-mm stent was used but with phalanges to avoid migration. Reported success rates were 87% but with a relatively high adverse event rate of 33%, mainly substernal chest pain, migration, nausea and vomiting, and stricture [7].
Blero et al. [4] described a plastic stent-based approach, specifically in patients after BSG. The study involved a limited number of patients with type II dysfunction (6 patients), but who were all successfully managed with this strategy, without major adverse events [4]. Marins Campos et al. [9] in another study reported the use of the same plastic stents in 41 patients with noneroded rings but in the context of banded Roux-en-Y gastric bypass. The stent remained in place for a mean of 15 days, and the results showed successful ring removal in all patients, no migration, vomiting, or abdominal pain in 22% of patients (n =9), and fibrotic strictures after stent removal in 22% (n =9)treatedwith endoscopic dilation [9].
Due to the lack of improvement after the initial dilations, unavailability of the plastic stents, and high adverse events of previously published metallic stent methods, we attempted to induce intragastric ring mi-gration with the partially covered Luso-Cor® esophageal metal stent, measuring 240 mm in total length with 30 mm diameter proximal and distal flares and 20 mm main body diameter. We believed that the proximal flare, which includes a 5-mm uncovered portion near the proximal edge, would maintain the stent in the distal esophagus. However, early distal migration of the stent occurred and only partial erosion of the silastic ring was achieved. We hypothesized that if the Luso-Cor® stent had remained for more time, circumferential erosion of the mucosa over the stent could have been possible, since most successful cases report a time of 2-4 weeks for stent placement [4, 7-9]. However, the mural pressure exerted by the Luso-Cor® stent may have been sufficient to relieve the luminal pressure of the silastic ring, realigning the ring with the remnant gastric tube, con-sequently contributing to the resolution of the patient’s symptoms.
In conclusion, band and ring dysfunction after bariatric surgery is a well-known adverse event and the approach to these patients should be multidisciplinary discussed. Endoscopic management is effective but the ideal choice of endoscopic procedure is unclear, with dilation and stents being the most effective. We hope this case report of this rare clinical entity may help to better understand the efficacy of specific covered metallic stents in the management of these patients.
References
1. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013; 23(4):427-36.
[ Links ]
2. Fink JM, Hetzenecker A, Seifert G, Runkel M, Laessle C, Fichtner-Feigl S, et al. Banded versus nonbanded sleeve gastrectomy: a randomized controlled trial with 3 years of follow-up. Ann Surg. 2020;272(5):690-5.
[ Links ]
3. Lemmens L, Van Den Bossche J, Zaveri H, Surve A. Banded sleeve gastrectomy: better long-term results? A long-term cohort study until 5 years follow-up in obese and superobese patients. Obes Surg. 2018;28(9):2687-95.
[ Links ]
4. Blero D, Eisendrath P, Vandermeeren A, Closset J, Mehdi A, Le Moine O, et al. Endoscopic removal of dysfunctioning bands or rings after restrictive bariatric procedures. Gastrointest Endosc. 2010;71(3):468-74.
[ Links ]
5. Collado-Pacheco D, Rábago-Torre LR, Arias-Rivera M, Ortega-Carbonel A, Olivares-Valles A, Alonso-Prada A, et al. Endoscopic extraction of adjustable gastric bands after intragastric migration as a complication of bariatric surgery: technique and advice. Endosc Int Open. 2016;4(6): E673-7.
[ Links ]
6. Campos JM, Evangelista LF, Ferraz AA, Galvao Neto MP, De Moura EGH, Sakai P, et al. Treatment of ring slippage after gastric bypass: long-term results after endoscopic dilation with an achalasia balloon (with videos). Gastrointest Endosc. 2010; 72(1):44-9.
[ Links ]
7. Wilson TD, Miller N, Brown N, Snyder BE, Wilson EB. Stent induced gastric wall erosion and endoscopic retrieval of nonadjustable gastric band: a new technique. Surg Endosc. 2013;27(5):1617-21.
[ Links ]
8. Talib A, de Ridder R, Straathof JW, Bouvy ND. Stent-induced compression necrosis for the endoscopic removal of a partially eroded Lap-Band. BMJ Case Rep. 2018; 2018:bcr2018224670.
[ Links ]
9. Marins Campos J, Moon RC, Magalhães Neto GEJ, Teixeira AF, Jawad MA, Bezerra Silva L, et al. Endoscopic treatment of food intolerance after a banded gastric bypass: inducing band erosion for removal using a plastic stent. Endoscopy. 2016;48(6):516-20.
[ Links ]
10. Buchwald H, Buchwald JN, McGlennon TW. Systematic review and meta-analysis of medium-term outcomes after banded rouxen-Y gastric bypass. Obes Surg. 2014;24(9): 1536-51.
[ Links ]