Introduction
Mucosal defect closure after endoscopic submucosal dissection (ESD) may reduce the likelihood of delayed bleeding and perforation [1]. Several devices are currently available for the closure of mucosal defects, including through-the-scope (TTS) and over-the-scope (OTS) clips, and OTS endoscopic suturing devices. However, defect closure can be technically demanding, with TTS clips typically limited to defects up to 20 mm, whereas OTS clips and suturing equipment require endoscope removal for device placement. More recently, the X-Tack Endoscopic HeliX Tacking System™, a novel TTS suturing device, has emerged as a potential tool for overcoming technical issues related to previous closure devices. We present 2 cases of gastric post-ESD defect closure with X-Tack, highlighting the technical challenges and main steps required to achieve high-quality closure without exposed submucosal tissue.
Case 1
A 73-year-old woman with a 15-mm Paris 0-IIb dysplastic lesion of the posterior wall of the antrum was referred for ESD (Fig. 1a). En bloc ESD was performed (Fig. 1b), and the 25-mm mucosal defect was closed with X-Tack in a “Z” pattern (Fig. 1c). However, the placement of the tacks was suboptimal leading to closure of the central part of the scar, leaving two areas of exposed submucosa at the edges. High-quality closure was achieved with the additional placement of four TTS clips at the edges, only possible due to the previously achieved proximity (Fig. 1d).
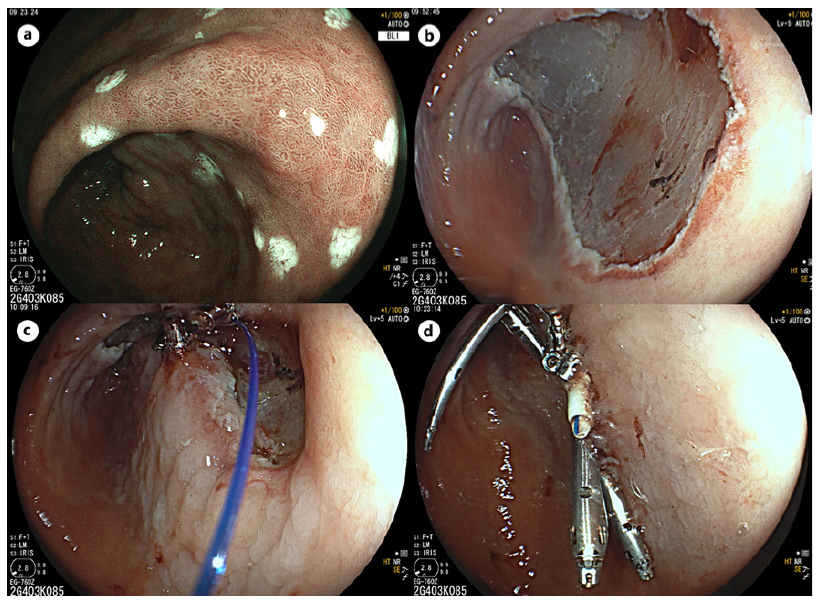
Fig. 1. a 15-mm Paris 0-IIb dysplastic lesion of the posterior wall of the antrum. b Post-ESD mucosal defect. c Mucosal defect after closure with X-Tack system: visible submucosal tissue at the edges of the defect due to tack suboptimal placement. d Complete closure of the defect after placement of TTS clips at both edges.
Case 2
A 55-year-old man was referred for ESD of a 13-mm Paris 0-IIa dysplastic lesion of the lesser curvature of the antrum (Fig. 2a). En bloc ESD was successfully performed (Fig. 2b). The 25-mm mucosal defect was subsequently closed using X-Tack in a “Z” pattern (Fig. 2c and online suppl. Video 1; for all online suppl. material, see https://doi. org/10.1159/000541865). High-quality closure was achieved with additional placement of one TTS clip (Fig. 2d).

Fig. 2. a 13-mm Paris 0-IIa dysplastic lesion of the lesser curvature of the antrum. b Post-ESD mucosal defect. c Mucosal defect after closure with X-Tack system. d Complete closure of the defect after placement of one TTS clip.
Both patients were discharged the following day and presented with no complications at 1-month follow-up. The risk of delayed bleeding post-gastric ESD ranges from 5% to 10% [2]. Routine coagulation of visible vessels at the end of the procedure has been shown to significantly reduce the risk of delayed bleeding [3]. There is currently insufficient evidence to support the routine implementation of additional techniques, such as mucosal closure using suturing devices. Despite limited data, mucosal closure with the new X-Tack device may be considered as a potential add-on to coagulation of visible vessels at the end of gastric ESD especially in patients at higher risk of delayed bleeding, such as those receiving antithrombotic therapy.
The X-Tack comprises four steel helix tacks connected by a 3-0 polypropylene suture, allowing the placement of tacks into adjacent healthy tissue, followed by cinching to hold the suture securely [4]. This method allows the management of sizable and deeper defects where conventional TTS and OTS clips may be insufficient. Studies in porcine models have confirmed the effectiveness of X-Tack in closing mucosal defects ranging from 20 mm to 50 mm [5]. More recently, a multicenter study concluded that the X-Tack provides a practical approach for repairing defects of up to 30 mm [6]. Larger defects may warrant additional sutures or a double-closure technique for optimal quality in up to 25% of cases [6]. Despite a lack of standardized suturing technique, “Z” patterns have been previously reported as more adequate for linear defects rather than for circular or irregular defects [7]. Nonetheless, precise tack placement is paramount to avoiding visible submucosa, precluding high-quality closure (Fig. 1c). Based on our initial experience, we recommend that the closure sequence of gastric post-ESD defects in the antrum should be as detailed in Figure 3.
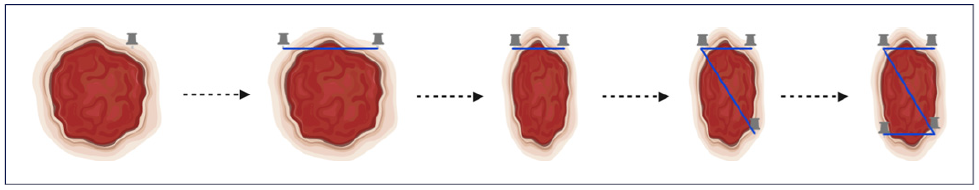
Fig. 3. X-Tack placement: the first tack should be placed distally to the margin, while the second tack should be placed vertically aligned (and not diagonally) with the first tack. The third tack should be applied diagonally to the second one, but also outside of the proximal edge of the lesion, while the fourth tack should be placed aligned and not diagonally to the third one (Z pattern).
Although this device has demonstrated safety and effectiveness, allowing for earlier discharge of patients, the X-Tack appears to be best suited for addressing superficial rather than full-thickness defects. While successfully closed perforations or post-intervention defects revealed sustained long-term outcomes (7.2 ± 3.3 months), recent data showed that fistula closure was linked to lower success rates (57.1%) [8]. This is understandable, as the helical tacks are designed to achieve mucosal apposition by engaging the muscularis propria, which may limit their effectiveness due to the lack of full-thickness anchoring.
In conclusion, these cases underscore the ability of X-Tack to offer a practical solution for closing large mucosal defects after endoscopic resection. While demonstrating efficacy in managing sizable defects, further research is needed to comprehensively evaluate its performance in comparison with other emerging alternatives like clip-endoloop and zipline techniques, especially concerning the ability to handle full-thickness defects and ensure long-term outcomes.















