Introduction
The majority of complications of cirrhosis such as acute variceal bleeding (AVB), ascites, and hepatic encephalopathy (HE) arise from portal hypertension and are responsible for important changes in the natural history of the disease, reflected in higher short- to medium-term mortality and recurrent hospital admissions [1, 2]. One of the most common and fatal complication is AVB which leads to an increase in short-term mortality from 20 to 30% [2, 3]. Despite advancements in the management of AVB over time, treatment failure with uncontrolled and recurrent bleeding remains a risk factor and predictor of high mortality [1]. Probably, the greatest step forward regarding the management of bleeding from portal hypertension is the placement of a preemptive transjugular intrahepatic portosystemic shunt (pTIPS). Making a side-to-side shunt between the hepatic and portal veins, the pTIPS can efficiently decrease the portal pressure gradient, creating an artificial shunt between portal and systemic circulation avoiding liver parenchyma, and therefore controlling variceal bleeding and preventing rebleeding [4]. First introduced in the 1960s as a salvage therapy for AVB refractory to standard treatment [5], this procedure was redefined by a landmark study by Garcia-Pagan et al. [6], which revealed the crucial role of pTIPS in the management of AVB. According to the Baveno VII consensus, it is recommended that patients presenting with esophageal varices and type 1/ 2 gastroesophageal varices should undergo pTIPS using polytetrafluorethylene covered stents within 72 h if they meet the following criteria: Child-Pugh class C <14; Child-Pugh class B >7 when active bleeding is observed during endoscopy, or the hepatic venous pressure gradient exceeds 20 mm Hg at the time of bleeding [7]. The advantages of pTIPS extend not only to the prophylaxis of rebleeding but also to the reduction of mortality and the prevention of de novo ascites, without a significant increase in the risk of HE [8, 9]. This study aimed to evaluate the effectiveness, regarding survival outcomes and early rebleeding, of pre-emptive TIPS compared to delayed TIPS placement or no intervention in patients with cirrhosis and high-risk AVB admitted to a tertiary referral center.
Materials and Methods
Study Design and Patients
This observational study included consecutive patients with liver cirrhosis admitted to our hospital due to bleeding from esophageal varices and type 1/2 gastrothe pTIPS group.
esophageal varices who meet any of the following criteria (pTIPS criteria): Child-Pugh class C 10-13 or Child-Pugh class B 8-9 plus active bleeding at initial endoscopy, according to Baveno VII consensus (study group) and a control group:
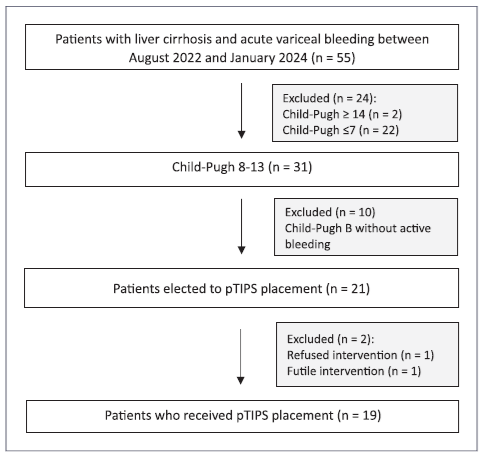
Group pTIPS (study group): patients who received preemptive TIPS placement within 72 h, between August 2022 and January 2024, prospectively included. Figure 1 represents a flowchart of the enrolled patients.
Control group: patients retrospectively selected between 2016 and 2022, who did not undergo pTIPS placement although fulfilled the pTIPS criteria. This group was then divided in 2 subgroups of patients: those who did not undergo TIPS placement during the course of their illness (subgroup A) and those who were submitted to TIPS placement due to rebleeding (subgroup B).
All patients were initially treated with standard-of-care treatment: vasoactive drug (terlipressin), antibiotics (mainly 1 g of ceftriaxone), restrictive blood transfusion, and endoscopic band ligation. According to the Baveno VII consensus and European Society of Gastrointestinal Endoscopy (ESGE) guidelines [10], all patients were submitted to upper digestive endoscopy within 12 h of presentation.
Terlipressin administration was continued for up to 5 days and antibiotics for 5-7 days. Exclusion criteria were age less than 18 or more than 80 years, pregnancy, Child-Pugh score <8and>13 points, inability to control bleeding at index endoscopy, previous portosystemic artificial shunt, bleeding from isolated gastric or ectopic varices, hepato-cellular carcinoma outside the Milan criteria, active sepsis, heart failure, and known total portal vein thrombosis.
All patients with AVB were studied with abdominal imaging, preferably contrast enhanced cross-sectional imaging to exclude splanchnic thrombosis, advanced hepatocellular carcinoma, and to map portosystemic collaterals in order to guide interventional treatment. Afterward, patients in pTIPS group continued on vaso-active drugs until a polytetrafluorethylene-covered TIPS was placed within 72 h after diagnostic endoscopy. TIPS procedures were carried out by four interventional radiologists experienced in this technique. Clinical/laboratory data and other relevant information during this period were used for the analysis. The control group was included in an outpatient endoscopic variceal band ligation program. Patients were followed up in a mini-mum period of 6 weeks, until March 2024 or death.
Study Outcomes
The primary outcome was survival at 6 weeks. This was considered mainly due to the follow-up time. Secondary outcomes included rates of early rebleeding (from day 5 to day 42), readmission for AVB, and development of HE. HE was diagnosed following American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver practice guidelines. HE was defined as occurrence of de novo typical neuropsychiatric symptoms due to the cognitive deficits and impaired neuromuscular function. Only overt (West Have grade ≥2) encephalopathy was considered. Subsidiary outcome was the duration of hospitalization in days.
Statistical Analysis
Categorical variables were described with frequencies and percentages, and continuous variables were expressed as mean and standard deviation or as median and interquartile range expressed in Q25-Q75 according to the distribution. Comparison of continuous variables was performed with Student’s t test or Mann-Whitney U test as appropriate for parametric and nonparametric data. Comparison of categorical variables was performed with χ2 test and with Fisher’s exact test when one group had <20 elements. A p value <0.05 was considered to be statistically significant for all analyses. Statistical analysis was performed using the Statistical Package for Social Sciences version 26.0.
Results
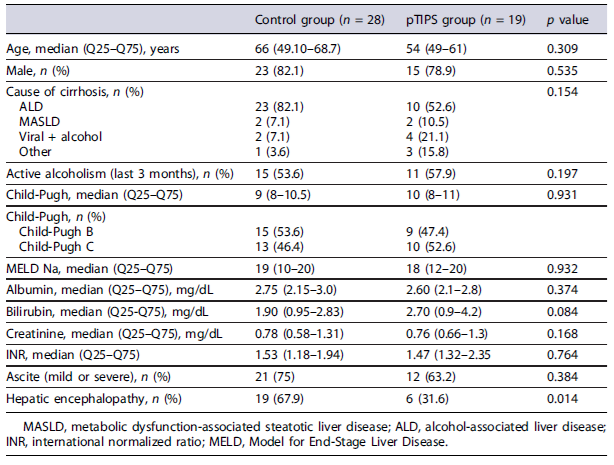
A total of 47 patients were included and divided into pTIPS group - 19 (40.4%) patients and control group - 28 (59.6%) patients. There were no differences in baseline characteristics between the two groups, except HE at admission, that was significantly higher in the control group when compared to the pTIPS group (67.9% vs. 31.6%, p = 0.014) as described in Table 1.
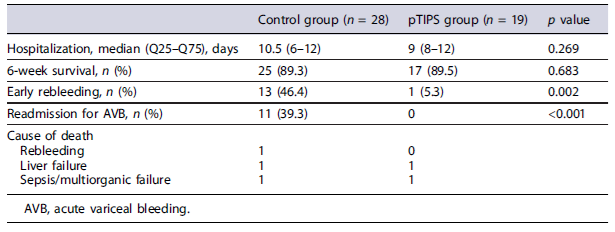
A total of 3 (10.8%) patients in the control group died, compared with 2 (10.5%) in the pTIPS group (p = 0.683). Therewerenosignificant differences in 6-week survival between the two groups. Patients in the control group remained hospitalized for a median of 10.5 days (6-12) compared to 9 days (8-12) in the pTIPS group (p = 0.269). Eleven patients (39.3%) in the control group were readmitted for AVB versus none in the pTIPS group (p < 0.001). Causes of death and outcomes, in both groups, are summarized in Table 2.
In the control group, 13 (46.4%) patients experienced early variceal rebleeding episode, and one died during the follow-up period due to uncontrolled bleeding. In 3 patients, TIPS was used as a rescue therapy. In this group, 11 (39.3%) patients underwent elective TIPS for recurrent bleeding from varices refractory to medical and endoscopic therapy, and the remaining 17 (60.8%) were not submitted to the procedure (subgroup A).
On the pTIPS group, one (5.3%) patient had variceal rebleeding episode. This patient was admitted to an intensive care unit and the rebleeding occurred 3 days after pTIPS placement. When there was this clinical suspicion, an upper digestive endoscopy was performed to confirm the bleeding. Accordingly, therapy was done. Therefore, TIPS revision was requested, but it was not possible to be done right away. Afterward the bleeding was controlled, so it was not considered mandatory. No deaths related to procedure or bleeding were observed. A markedly reduced incidence of this end point in the pTIPS group versus the control group was observed (p = 0.002).
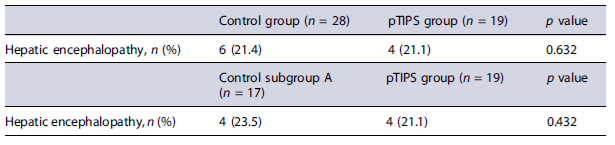
In the control group, 6 (24.4%) patients developed HE while in the pTIPS group, only 4 (21.1%) (p = 0.632). In the subgroup A, 4 (23.5%) patients developed HE. When comparing this subgroup to the pTIPS group, there were no significant differences regarding development of HE (p = 0.432). These results are explained in Table 3.
Discussion
Considering the high mortality rate inherently linked with AVB, it is vital to identify a subgroup of patients at risk of treatment failure. Any supplementary measures to avert or lessen the likelihood of future bleeding are essential to improve survival and quality of life [11-13]. Using the well-known score of Child-Turcotte-Pugh, and endoscopic findings (high-risk defined as Child-Pugh C cirrhosis <14 or Child-Pugh B>7 cirrhosis with active bleeding), Garcia-Pagan et al. [6] redefined the role of pTIPS in this subgroup of patients with AVB. A recent multicenter large study underscored this important role of the pTIPS [14]. In the study by Monescillo et al. [15], the authors compared pTIPS with standard-of-care (endoscopic plus pharmacologic treatment) and demonstrated a significant reduction in treatment failure and rebleeding (3% vs. 45%) and 1-year survival (86% vs. 61%). The discoveries in this pivotal study marked a significant shift, sparking renewed enthusiasm for the use of preemptive TIPS in clinical settings as a subject for ongoing clinical research. Later, Garcia-Pagán et al. [11] developed a post-RCT surveillance study to evaluate the earlier findings and found similar lower incidence of rebleeding and failure to control bleeding (7% vs. 50%; p < 0.001). However, 1-year survival failed to reach statistical significance (86% vs. 70%, p = 0.056), like other study of 31 patients admitted to an intensive care unit (1-year survival 66.8% vs. 74.2%, p = 0.78), although it achieved lower rebleeding rates [12]. Similarly, a recent published UK-based RCT by Dunne et al. [9] concluded that preemptive TIPS intervention does not confer sur-vival advantage. On the other hand, a meta-analysis by Deltenre et al. [16] and recently by Nicoară-Farcău et al.[17] confirmed the significant survival advantage of pTIPS in these high-risk patients. Our study corroborates that the use of pTIPS improves the outcome of these patients in terms of rebleeding, but there was no significant difference in 6-week survival.
HE is a frequent issue following TIPS, with an estimated 35-50% of patients likely to experience HE after TIPS insertion [1, 18]. In the context of rescue TIPS, this risk is generally accepted, given the clinical advantages and the life-saving nature of the TIPS procedure. However, in the case of pTIPS, HE is a valid concern for a patient who is otherwise stable and has received standard care. As such, the benefits of pTIPS must be carefully weighed against the risk of HE [1]. Also frequent in AVB, HE is a factor associated with low survival rates and the related studies mention that pTIPS improves outcomes without increasing the cumulative incidence of HE [11, 14-16]. Finally, a recent study by Rudler et al. [19] support these findings with incidence of HE being similar between patients treated with pTIPS versus endoscopic plus drug treatment (38.2% vs. 38.7%, p = 0.972), even in patients with HE at admission. Our findings are in line with data from the aforementioned studies with similar rates of HE in all groups. Furthermore, we carried out a sub-analysis with patients who did not receive TIPS throughout their illness (subgroup A) and, even in these, the results were in concordance.
Being a high-specialized and challenging technique, it is difficult to adopt the pTIPS concept, even in tertiary centers. This is reflected on real-life numbers, with less than 7% of eligible patients receiving the procedure in a French audit with 964 patients [20]. The future of the technique should involve the transference of patients to high-volume centers. On the other hand, the cost-effectiveness of pTIPS is not the object of extended studies. Harman et al. [21] performed a retrospective analysis over a 1-year period and estimated that pTIPS insertion would save GBP 534.70 per patient per year (p < 0.0001), using a 3.2% rebleeding rate and remained cost-effective even with a rate of 12%. These findings favor the use of pTIPS in terms of global healthcare cost. Despite not addressing the issue of cost-effectiveness, our study demonstrates that the pTIPS group had fewer readmissions due to rebleeding. Consequently, we can infer that it is likely that the costs might be inferior in the pTIPS setting. It is known that these patients do not require an endoscopic variceal band ligation program and have improvement of ascites. All these factors may translate into less use of healthcare services and associated costs. However, we did not analyze objectively healthcare costs. Therefore, it is not possible to draw this conclusion.
As a tertiary center, the strong achievement of our experience lies in the 24-h availability of an interventional radiologist team for procedures like pTIPS. In all patients that fulfilled the pTIPS criteria, it was possible to place pTIPS. As far as we know, this is the first study published in a Portuguese tertiary hospital, outside the clinical research setting. This real-life study shows that Baveno VII recommendations can be implemented. These points reinforce the value of this study, with an acceptable number of patients, considering the difficulties to introduce new complex procedures in this setting. However, our study has some limitations. Having a larger number of enrolled patients could strengthen our statistical findings. On the other hand, to achieve strong conclusions in terms of pTIPS benefits, other outcomes such as de novo and worsening ascites should be considered, as well as a larger follow-up time. Besides, the retrospective nature of the control group might have created a bias due to difficulties in accessing clinical data. We must assume the possibility of a potential bias in the sub-group B because we did not isolate the two sub-groups in the baseline characteristics table. However, the important comparison is between subgroup A (of patients who were not submitted do TIPS) and the study group.
This real-life study highlights the potential benefits of pTIPS placement in decreasing early rebleeding, without increasing HE and thereby lowering morbidity, and complications. Our findings advocate for the proactive incorporation of pTIPS into clinical practice to optimize patient outcomes following AVB, making pTIPS a more attractive option in the long term.