Introduction
Tuberculosis (TB) is one of the top 10 causes of death worldwide and the leading cause among infectious diseases. Its control has been weakened by the increase of cases with resistance to rifampicin and isoniazid, the main treatment drugs (1).
Multidrug-resistant TB (MDR-TB) is defined as TB with resistance to at least rifampicin and isoniazid. Extensively resistant TB (XDR-TB) is increased by resistance to ≥1 fluoroquinolone and at least 1/3 second-line injectable drugs used to treat TB (capreomycin, kanamycin, and amikacin) (2).
Treatment for MDR/XDR-TB can last almost 2 years and is more expensive, more toxic, and less effective than treating TB caused by drug-sensitive bacilli (3). Moreover, a patient with MDR and comorbidities, such as human immunodeficiency virus (HIV), takes 20 tablets and 1 injectable drug daily which, in turn, reduce a patient’s compliance and quality of life, making treatment management difficult for the health-care team (4).
In Portugal, despite the significant reduction in TB indicators in the last decade, TB is still a public health problem. Most of the TB cases occur in the districts of Lisbon and Porto (5).
This study aims to analyze patients’ narratives about the challenges they face during the treatment of MDR-TB and XDR-TB and identify the support factors that help them.
Methods
This was a qualitative descriptive study with purposive sampling. The Consolidated Criteria for Reporting Qualitative Research (COREQ) were applied to ensure study rigor (6).
Research was conducted at tuberculosis outpatient units (CDP), which are reference units for the diagnosis, treatment, and prevention of TB and MDR/XDR-TB in Lisbon and the Tagus Valley region (LVT).
Participants older than 18 years who were undergoing treatment for MDR/XDR-TB and spoke and understood Portuguese were included. Participants who were not living in the Lisbon District, and those with serious mental illness or cognitive limitations were excluded.
Data were collected through semi-structured interviews conducted between November 2017 and May 2018. The interviews were conducted using an original script that drew on the available literature and group discussions. We did 2 pilot interviews-and revised the interview guide. Before each meeting, the researcher explained the content and purpose of the interview to the interviewees. All the interviews were conducted individually and face-to-face by the first author, and audio-recorded. Theoretical saturation was used as a criterion for interrupting further interviews (7). All interviews were transcribed verbatim using anonymous participant identifiers.
The interview guide was composed of 2 parts. The first part has structured questions about the clinical and demographic variables: sex, age, country of origin, date of beginning the treatment, marital status, number of people residing at his/her residence, years of study, occupational status, monthly household income, type of residence (own/rent/municipal housing), location of residence, HIV status, previous treatment for TB, other TB cases in the family, and drug resistance category. The second part has questions about the disease history, knowledge, experiences, and feelings of the patient in relation to his/her treatment.
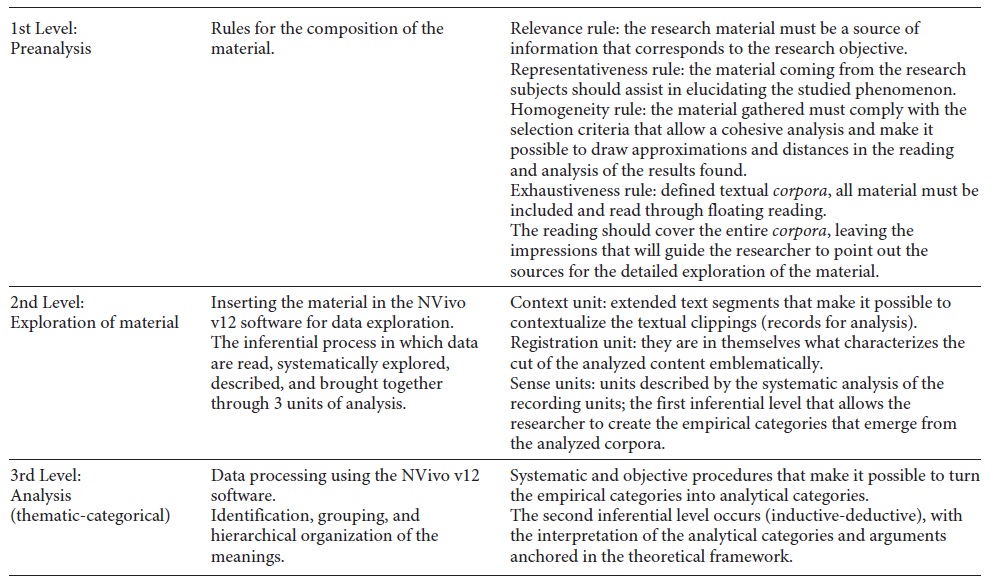
The analysis was conducted according to the thematic content analysis stages: pre-analysis, exploration, data analysis process, and interpretation (Table 1) (8). The software Nvivo v12 was used to code and cross-reference themes with participant characterization data. The themes were derived from interviews and were discussed by 3 researchers until unanimity was reached. Participants’ clinical and demographics were analyzed by means of descriptive statistics.
Results
Twenty patients were treated at the CDP in the study period. Nine participants were invited; 8 agreed to participate in the interview and 1 was excluded due to cognitive limitations. The patients were interviewed until theoretical saturation occurred. There were 5 males and 3 females aged between 21 and 63 years (median 45 years). The group of interviewees was composed of 6 people of Portuguese origin, 1 of Angolan descent, and 1 of Cape Verdean origin. Patients were at different stages of treatment, i.e., varying from the 4th to the 21st month.
Regarding marital status, 4 (50%) were married or living in a stable union, and 5 (62.5%) lived with ≥5 people in the same residence. Only 1 patient lived alone. All patients had some level of education, ranging from the 4th grade to technical courses.
As for occupational status, 3 were on social security (a domestic, a cleaning professional, and a panel beater), 1 was a student, and 4 were unemployed. The monthly household income was, at the most, the minimum wage, and only 1 had no income.
Portugal has a housing policy whereby municipalities offer rental properties to low-income families at prices lower than the official market. Of the patients interviewed, 3 lived in publicly owned houses. Sintra was the most common place of residence (5 patients; 62.5%). Only 2 patients had a previous history of TB, and the other 6 had other cases of TB in their families during the interview period. Two patients had HIV coinfection and 2 had XDR-TB.
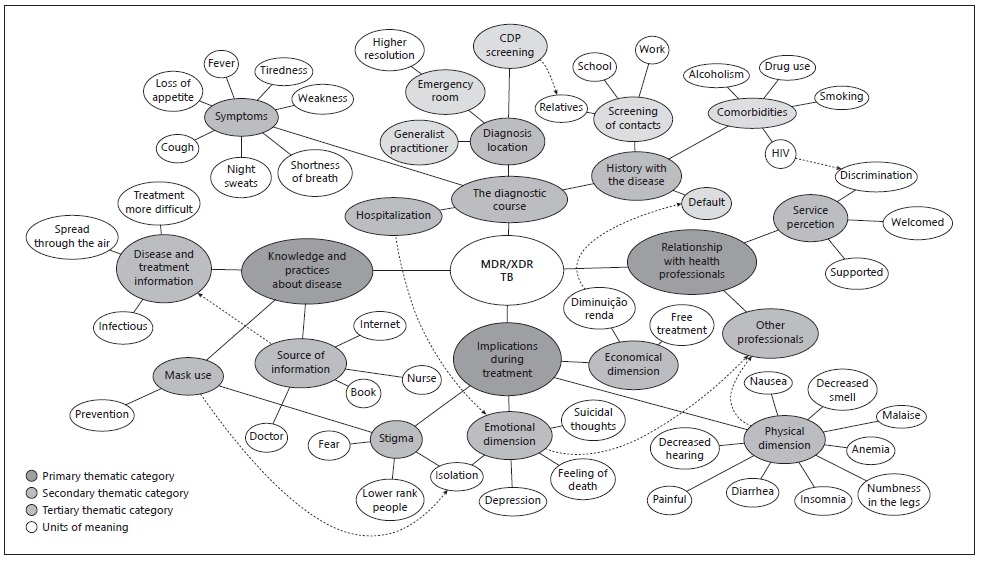
The thematic content analysis of the interviews made it possible to structure a tree of thematic nodes. From the thematic-categorical analysis framework, it was possible to structure a discussion based on 4 thematic categories that address the patient’s experience during treatment, knowledge about the disease, the relations established with the health professionals, and the consequences of the disease and treatment.
The primary, secondary, and tertiary thematic categories, and the units of meaning are displayed in Figure 1. The dotted arrows seek to establish, in a more dynamic way, the relationships between the themes and units of meaning. From this, it is clear that the themes are not static, and that they influence >1 of the issues highlighted
The diagnostic course category encompassed the reported symptoms, adverse events until diagnosis, hospitalization, and behaviors that advanced or delayed the initial process of disease development and treatment.
Among the symptoms, most patients (62.5%) reported tiredness or weakness as the most striking symptom, followed by cough (50%) and loss of appetite/weight loss, shortness of breath/difficulty breathing, fever, and night sweats (25% each).
Five (62.5%) patients were diagnosed in the hospital. Two had previously sought health care, but the diagnosis was allergic cough and flu. When the condition of one patient persisted, he reported that he had gone to the health unit, but after the worsening of his clinical condition, he resorted to the hospital emergency room.
In this study, we observed that requiring immediate resolution of their health problems was the crucial factor that led patients to seek medical care.
As for hospitalization, although there is no legal norm in Portugal, it is recommended that patients resistant to multiple drugs remain hospitalized until the direct sputum examination is negative in 3 consecutive samples. Hospitalization is proposed to the patient, but not imposed; if they do not want to be hospitalized, the health-care team goes to their home. Of the 8 patients interviewed, 6 (75%) were hospitalized.
Regarding the history of the disease, the statements referring to contact screening, comorbidities, and previous nonadherence were categorized. In total, 7 (87.5%) patients reported that relatives or colleagues from school or work had undergone TB screening. Six (75%) patients had relatives with MDR-TB.
The most-reported comorbidities were alcoholism (37.5%) and smoking (12.5%). Two patients were employed in the construction industry. They attributed possible contagion to the habit of sharing drink bottles and smoking cigars.
Two patients reported having had drug-sensitive TB, 1 of whom stopped his TB and AIDS treatment because he thought he was already better.
I was feeling good. I never worried about these treatment things, and I wasn’t caring about these treatment things, these things... After first tuberculosis I got, I was fine, feeling good... I went back to work; only then, I stopped doing HIV treatment.(PAC2)
The knowledge and practices about the disease category made it possible to identify the level of information patients have about the disease and how it may affect treatment. All patients proved to have some degree of knowledge about the disease. The most prevalent information was that TB is an airborne disease (63.5%) and is infectious (50%), and that MDR-TB treatment is more difficult than that for TB caused by drug-sensitive bacilli (50%).
I know it’s multiresistant, it’s the strongest of all. It’s harder to treat, right, this is not simple. The nurse told me that a “bug” (bacillus) made a small bag inside the lung that, after treatment, it was still there. That’s why treatment takes so long to make sure you even get the “bug” inside.(PAC1)
Regarding the source of information about the disease, 6 (75%) patients received this from the health-care team and 2 (25%) reported having researched it via books and the Internet. During hospitalization, respondents said that the nursing staff focused on health education to inform them about TB.
All patients underwent supervised treatment. In the initial phase, where injectable medications are used, when the patient was not hospitalized, the nursing staff performed home visits. In the oral medication phase, 4 (50%) patients reported going to the health unit daily to take the medication. Three patients (37.5%) received daily home visits from the health-care team. One (12.5%) patient with walking difficulties, had to have the medication given to their mother who was also responsible for supervision.
The nurses at the health center kept the medicine, and they went there (at the patient’s house) to make me take medicine every day… and they had to watch me take it, and I got an injection every day… That was six months, always like this. Injections(PAC1)
The use of a face mask appeared in the reports of 4 (50%) patients as an instrument associated with the prevention of disease transmission.
Imagine they are all there on the transport. People are all coughing and breathing. So, the mask is to protect us and not to contaminate anyone. Even the Chinese wear a mask. People look a little but don’t stare...(PAC6)
The relationship with the health professionals has to do with patients’ feelings during treatment. Overall, 7 (87.5%) patients said they had felt welcomed by the health-care workers. Three (37.5%) stressed that they would not have been able to perform the treatment had it not been for the support and constant presence of the professionals.
If I had not had the nurse, I would not have made it, and it’s tough two or three days, then it is hard to come down… But after a week it was hard... If the nurse wasn’t there every day, saying I have to take it, go slow because it was about ten or so and big. And then she would say one at a time, swallowing. And then only when I was done, she went away. She had to see me taking all (medicines). If there wasn’t someone there supporting me, I don’t think anyone can do it on their own.(PAC1)
In turn, 1 (12.5%) patient said she had felt discriminated against for having HIV.
Sometimes there is a doctor who has a heart…but not all have it. It’s like in hospitals. Not everyone sees a person who has HIV with kind eyes. But a health professional should not do this… but many are indifferent. They say discrimination doesn’t exist; that’s what they say. Do you think not?(PAC2)
At CDP, the health team is composed only of doctors and nurses. Four patients (50%) reported that they needed the help of other professionals to solve problems directly or indirectly linked to the disease. Two required a social worker to assist with benefit-related issues. Two patients required a psychologist to treat depression, 1 a psychiatrist to treat addiction, and 1 a physiotherapist to treat swelling and pain in the lower limbs due to the side effects of the medication.
The indications of the treatment category made it possible to identify how the patient was affected during the treatment, either emotionally or physically as well as including statements that reflected the stigma of the disease. In this sense, TB appeared to be associated with “fear” and as a disease of “lower rank people.” Half of the patients reported that only family and close friends had known about the disease, and that they hid the fact that they were sick from neighbors. The association of the disease with death was also present in the narrative of 3 (37.5%) patients.
I know that tuberculosis is a disease that kills. And you can pass it on to other people. I know it’s a dangerous disease because in the past many people died from it. (PAC1)
The use of a face mask appeared as a stigma when a patient asked the professionals to allow him or her to put on the mask only when they entered his or her home.
At first, they (nurses) went there wearing a mask (at the patient’s house). They were wearing a mask, and my neighbors would comment, and they came to ask what it was. I never told them what it was. I don’t have to say, right?! And then there was a time when I asked them just to wear the mask at the entrance (after entering the patient’s home). (PAC6)
Six (75%) patients reported emotional difficulties. The length of stay in isolation was considered extremely difficult by 3 (37.5%) patients who described the difficulty of being secluded for long periods as a feeling of impending death, deep sadness, and suicidal thoughts.
Regarding the physical dimension of treatment, the main adverse events described by the patients were the following: malaise (75%), nausea, loss of appetite (62.5% each), numbness in the legs (37.5%), and anemia (37.5%). Treatment was reported to be painful and exhausting by patients as well as causing severe physical limitations.
Then, following the injection, the person is in such a bad state that afterward, it is difficult for a person to move there for a long time... Because the injection is strong and painful... It has to be given very slowly for us to feel... If the nurse doesn’t know how to do the injection, it’s too fast, and it hurts a lot. And then you must get some rest...(PAC3)
Regarding the treatment and its costs, in Portugal, the health system works on the basis of coparticipation, i.e., some is paid by the patient. However, for public health diseases, treatment and additional tests are completely free. No patient reported having difficulty doing the tests or there being a lack of medication during treatment.
Discussion
The narrative of the journey from symptoms, to diagnosis, to adverse events associated with treatment, can provide a broader view of the available resources and the difficulties faced by MDR-TB patients in Lisbon.
It should be noted that it was the symptoms of TB that made the patients seek medical help. Diagnoses were made at GP practices or at the hospital where there are specialists. Although most of the patients interviewed went to their GP, 2 patients went to hospital because of their worsening clinical condition and were then diagnosed.
In recent years, there has been an expansion of the primary health-care network designed to assign family health-care teams to all people living in Portugal. Between 2010 and 2017, the percentage of the Portuguese population assigned a family doctor went from 85.8 to 92.7%. Despite this increase, the LVT region has the lowest coverage in the country, 82.5% (9). Nevertheless, the hospital network is half an hour away from any home; this, in turn, facilitates access to emergency appointments for people residing in the LVT region (10).
In the basic health unit, 2 patients received a first diagnosis of flu and allergic cough. A study conducted in Portugal found an average time span of 33 days between symptom onset and first contact with the health service. The same study also found a 17-day period between the patient’s first contact with the health service and the beginning of treatment. In total, the median was 68 days between symptom onset and treatment onset (11). Reducing the time to diagnosis, primarily by continuous training of TB professionals, has been one of the challenges of disease control faced by the country (5).
After diagnosis, cases with positive smear are hospitalized. This was the case for most of the patients interviewed. In Portugal, in addition to cases associated with disease severity and social issues, hospitalization is recommended for cases of contagious-stage MDR-TB. Although there are no legal mechanisms that oblige the patient to undergo treatment, none of the respondents questioned this measure. On the one hand, hospitalization in the contagion period is a way of preventing the spread of the disease. On the other, it can cause physical and emotional damage to some patients.
Hospitalization involves isolating the patient, sometimes for several months. This was very difficult for patients. Prolonged isolation was associated with a feeling of impending death, deep sadness, and suicidal thoughts. A study of hospitalized MDR-TB patients found that 26% of them had symptoms of depression and/or anxiety (12). Another study of 45 patients with MDR-TB and HIV coinfection indicated that 16% had symptoms of depression (13).
In addition, some of the drugs used to treat MDR-TB can cause psychiatric disorders such as psychosis and depression (14). Teams involved in treating MDR-TB patients should be trained to apply appropriate mental health assessment tools, especially early on, so that psychiatric disorders can be identified as soon as possible (13).
Moreover, patients on MDR-TB treatment may commonly experience the symptoms of stigma, discrimination, and psychological distress (14). In our work, the social stigma can be confirmed by the fact that most patients did not tell their friends and acquaintances about the disease. The face mask also appeared in interviews as a symbol of social stigma, because while protecting the patient, it also exposes the disease. In the contagion period, patients should wear a mask if they come into contact with other people. The patients interviewed preferred to be more secluded. This voluntary isolation may be the result of a feeling of self-discrimination, which leads the patient to anticipate the isolation that society will impose on them (15).
Only of the patients with HIV coinfection expressed feeling they were discriminated against. Like TB, HIV is stigmatized in this context because it is linked to other undervalued characteristics, which are also social determinants of health. TB can also be perceived as a marker of HIV positivity in areas of high disease prevalence. Therefore, HIV-associated stigma can also be transferred to individuals infected with TB (16).
Stigma is one of the most common barriers in the fight against tuberculosis. Among the causes are the associations of TB with poverty, malnutrition, immigrant status, and lower social class (16). Even though stigma is often viewed as natural, intractable, or easily overcome with an overall improvement in the quality of or access to health services, it must be identified and addressed with educational measures (17).
Although treatment failure is the central hypothesis regarding the development of resistance to multiple drugs, only 2 patients reported having had previous TB treatment and only 1 defaulted. In Lisbon, the predominance of primary infection can be explained by the endemic circulation of MDR strains of TB (18).
In our study, there was a high intrahousehold transmission rate. Of the 8 patients interviewed, 6 had family members with MDR-TB. All patients, however, reported that family members and other contacts had been called to the CDP for disease and infection screening. Recent studies conducted in Portugal, combining a strain genotyping analysis with epidemiological data from MDR-TB cases, have confirmed strong epidemiological links (19).
Nonadherence to treatment was not a recurring problem in the sample studied. Only 1 patient abandoned his previous treatment, claiming he had felt better and needed to go back to work. Understanding the disease itself and its consequences is vital for the patient to acknowledge the importance of maintaining treatment (20). We observed that the patients were aware of the transmission of the disease and the greater difficulty of treating MDR cases. In our analysis, it was possible to verify that some patients researched the disease themselves, in books and on the Internet, but most cited the health-care team as the source of information. On the basis of the communication with the health professional, patients build ideas around their diagnosis and treatment (21). The perception of the disease itself and the importance of treatment depend on receiving the correct information, and so there must be a good relationship between the patient and the health-care team (22).
In Portugal, TB treatment is free, which contributes to improving treatment adherence, but that alone is not enough. As a strategy for TB control, all patients undergo directly observed treatment (DOT) and, at the CDP in Lisbon, they receive transport tickets for their appointments. The patients in our sample highlighted that the most important factor for the continuity of treatment was the support provided by the health-care team. The interviewees were satisfied with the team, emphasizing that their support had been essential for the continuity of treatment, especially in the first phase of the scheme which includes drug injections as well as taking a large number of pills. DOT can provide the patient with a moment to express their doubts and problems and allow the health professional to identify other needs, thereby strengthening the continuity of treatment (23).
Finally, treatment for MDR-TB is long and painful, with a high frequency of adverse events (24). Second-line medications are often associated with adverse events, ranging from mild to fatal, requiring temporary or permanent drug discontinuation (25). In our study, adverse events were reported by 87.5% of the patients interviewed. The patients said they had had careful clinical follow-up, and that, when necessary, had been referred to other specialists. Although there was no multidisciplinary team at the CDP, patients were referred to specialized services when needed. Even a high proportion of adverse events which sometimes disrupted routine activities, did not prevent the continuity of treatment.
Some limitations of our work should be acknowledged. Before the interviews, we tried to encourage patents to relax and we provided them with opportunities to express their thoughts. Health professionals were not present during the interviews, but then again, someone in a position of authority can also deter patients talking openly. Although this study has a small sample that does not necessarily represent the perceptions of all patients, it is a starting point for identifying patients’ needs and expectations during TB treatment.
Conclusion
This study showed that depression, social discrimination, and side effects of drugs were challenges faced by patients with MDR-TB. Nevertheless, the good relationship of patients with the health team and supervised treatment were factors found to be relevant for better adherence to treatment. This finding indicates that it is key that health services acknowledge and tackle patients’ emotional and social needs during treatment.
Suggestions for future interventions include building health team capacity to identify symptoms of depression early, increasing public awareness of the disease, expanding the multidisciplinary team at the CDP, and increasing the possibilities of individualized social support for patients. In addition, it is important to investigate whether patients’ perceptions vary with time, age, support, and treatment stage. Likewise, it is also key to analyze what are the moderating or mediating impact of variables that could mitigate the effects of treatment on patients.
Acknowledgements
We thank the LVT Regional Reference Centre for MDR-TB and the Department of Public Health of the ARSLVT. Our very special thanks to all the professionals at CDP LVT, especially Dr Maria da Conceição Gomes, Dr Carlos Gomes, nurse Isabel Louro and nurse Cristina Figueiredo.
Statement of Ethics
The Ethics Committee for Health of Lisbon and Tagus Valley Region Health Administration approved the study (ref. 11101/CES/2017). All participants were fully informed about the content of the study. The voluntary and confidential nature of the study was stressed, and the participants had the right to withdraw from the study at any time. In addition, the fact that refusal or withdrawal from the study would not influence the care the patients received was also emphasized. Verbal and written informed consent were obtained before the interviews.
Author Contributions
M.B., A.F., and R.D. conceptualized and designed the study; V.S. contributed to the study methodology and interpretation of results; M.B., V.S.J., and F.B.A.S. contributed to qualitative analysis; M.B. handled the database, did the data collection, and wrote the manuscript. All authors critically reviewed the paper and read and approved the final version.