Introduction
Schizophrenia is a severe mental disorder, characterized by DSM-V as the presence of at least two of the following symptoms: (1) delusions, (2) hallucinations, (3) disorganized speech, (4) disorganized behaviour, and (5) negative symptoms, in which at least one of the symptoms is one of the first three. The level of functioning is markedly below the level previously achieved, in areas such as interpersonal relationships, work, or self-care, for a considerable period of time 1. Cognitive and affective symptoms that worsen functional impairment are also common 2.
This condition is a leading cause of disability worldwide, and the global burden of disease is substantial, accounting in 2019 for 1.8% of total years lived with disability (YLD) 3. The peak burden of disease is observed between the ages of 30 and 40 years 4. Early disease onset, low remission rates, and high disability burden contribute to the high overall burden associated with schizophrenia 4.
A systematic review of the literature concluded that the high economic burden of schizophrenia suggests inadequate health services for these patients worldwide 5. In Portugal, for example, psychosocial rehabilitation services are scarce and those that exist are inaccessible to most of the population. It is important to promote informed policy decisions that lead to the growing recognition that schizophrenia has a high global economic and epidemiological burden and that it is necessary to adopt strategies that reduce this burden 4,5. For the economic and epidemiological burden of the disorder to decrease, continued and integrated care by health services is necessary for the person and family. This follow-up includes preventing functional disability and promoting psychosocial rehabilitation and community integration. Since the lack of awareness of the disease and low adherence to therapy are recurring problems that lead to relapses 6,7, interventions that promote awareness of the disease and adherence to therapy should be planned and implemented to prevent relapses. Family support is another essential factor for psychosocial rehabilitation, and psychoeducation should be given priority, not only for the patient 8, but also for the family 9. Other interventions, such as metacognitive training 10,11 to manage delusions and social skills training 12, among others 13, should be considered according to individual and family needs. In this way, psychosocial and occupational disability is prevented, reducing the overall burden of disorder and decreasing YLD.
Several international studies prove the severe impairment in functioning of people diagnosed with schizophrenia, especially regarding social and/or occupational functioning 10,14-17. Negative symptoms were pointed out in a systematic review of the literature as persistent predictors of worse functioning when compared to positive symptoms 18. It is also known that each relapse further worsens the previous functional level 2. Another systematic review of the literature found that functional impairment in schizophrenia is not only related to mental functions, but is also due to activity and participation domains 15, so it is important to assess factors related to these domains as well.
In addition to the above, limitations in psychosocial function are significant, and people with schizophrenia are more likely to be unemployed, homeless, live in poverty, have difficulties performing domestic chores and self-care, and are dependent on continuous support from family caregivers and mental health services 4. As an aggravating factor, the greatest burden of schizophrenia is among 25- to 54-year-olds, an age when individuals are most likely to be economically productive, leading to significant socioeconomic deficits 4. In Portugal, a recent study with a sample of 282 people with schizophrenia from the north to the south of the country, with a mean age of 46.15 years, showed a low rate of people with professional/academic occupations (9.2%), and only 14.2% were married or had a partner. As for cohabitation, 55.6% lived with their parents (37.2%) or in institutions (18.4%) 17.
Research in the area of schizophrenia and mental health services has been increasingly focusing on psychosocial rehabilitation, one of the goals of which is to improve functioning, making it essential to evaluate it as a way to identify health gains 19. Recovery is multidimensional, and at least two areas should be considered: clinical remission and social functioning. The functional outcome should be a priority target for intervention in schizophrenia, and it is essential to assess treatment response, remission and functional recovery. Clinical and functional outcomes in schizophrenia can be achieved only through an integrated, multifaceted approach involving pharmacotherapy, psychosocial interventions and attention to environmental factors 20.
The World Health Organization developed the International Classification of Functioning, Disability and Health (ICF) to standardize the assessment of functioning and disability worldwide. The components that make up this assessment include body functions and structures; activities and participation; and contextual factors (environmental and personal). Disability is evaluated according to impairments, activity limitation or participation restriction 21.
The constructs that comprise the dimensions related to body functions and structures, activities and participation, and environmental factors are qualified according to Figure 1, classifying the problem in its extension or magnitude 21.
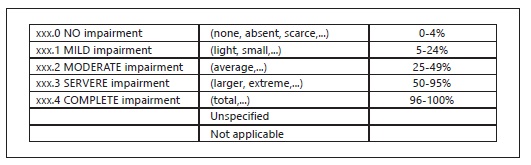
Fig. 1 Classification scale of the categories (example). xxx, domain number of the second level. Source: WHO 21.
To evaluate the functioning of people with schizophrenia, a group of experts defined a Core Set composed of the constructs that best fit the pathological and functional characteristics of this disorder, which was later reduced to be more easily and quickly applied in clinical practice. Thus, the Brief ICF Core Set for schizophrenia was created, consisting of 25 categories, to provide an international standard for assessing the functioning of people diagnosed with schizophrenia 22.
However, neither the ICF nor the ICF Brief Core Set for schizophrenia clearly defines criteria for assessing the degree of disability of the person in each of the categories. For this reason and to have greater precision and standardization in the evaluation of the functioning of the person with schizophrenia, this study aimed to develop a classification scale of the degree of disability for each of the categories of the Brief ICF Core Set for schizophrenia (named Schizophrenia Functioning Core Set).
Materials and Methods
Design
To meet the aim of the study, the authors initially developed the criteria for assessing the degree of functional disability for each of the categories of the Brief ICF Core Set for schizophrenia. Subsequently, we used the modified e-Delphi method, applying an online structured questionnaire to a group of experts in the field of schizophrenia to assess the degree of agreement with each criterion. There are three reasons for using an e-Delphi, rather than a classic Delphi: (1) convenience for the e-Delphi administrator and research participants; (2) time and cost savings; and (3) ease of data management 23. Modified Delphi should be used when basic information regarding the target question is available 24. In this study, we used the previously developed Brief ICF Core Set for schizophrenia 22 and developed the evaluation criteria for each item.
Development of Criteria for the Evaluation of the Degree of Functional Disability
In a first step, the categories of the Brief ICF Core Set for schizophrenia were analysed, and classification criteria for the different degrees of disability in each one were developed. The definition of the criteria was based not only on the specific characteristics of this disorder described in DSM-V and the International Classification of Diseases (ICD-11), but also on the analysis of the items of the Personal and Social Performance Scale (PSP), the Quality of Life Scale (QLS) and the Psychotic Symptom Rating Scales (PSYRATS), specific international reference instruments for the assessment of the person with schizophrenia. The PSP was developed in 2000 to assess psychosocial functioning, with four domains: socially useful activities; personal and social relationships; self-care; and aggressive behaviours 25. The QLS was developed in 1984 to evaluate functioning, taking into account the negative symptoms of the disorder, regardless of the presence or absence of psychotic symptoms. It has four dimensions: intrapsychic functions; interpersonal relations; occupational roles; and common objects 26. It is the most used instrument in studies that evaluate the functioning of a person with schizophrenia 27. The PSYRATS evaluates psychotic symptoms and has two domains: hallucinations and delusions 28. In addition to the above, we based the evaluation of some of the items on the Elderly Nursing Core Set, developed by one of the authors of this study 29,30, since they are also appropriate for people with schizophrenia.
After developing the rating criteria for each of the 25 categories of the Brief ICF Core Set for schizophrenia, we named the instrument the “Schizophrenia Functioning Core Set.”
Modified e-Delphi Method
The Schizophrenia Functioning Core Set was subjected to expert validation using the modified e-Delphi method. For this purpose, we conducted an online structured questionnaire that was sent by email to 44 experts in the field of schizophrenia, from different professional categories, in modified Delphi round 1. The period for answering the questions in the first round ran from September 22 to October 18, 2020.
The questionnaire sent to the experts aimed to assess the degree of agreement with the defined classification criteria, which was assessed using a 5-point Likert scale: totally agree (1); partly agree (2); neither agree nor disagree (3); partly disagree (4), and totally disagree (5). Each question asked for suggestions for improvement, if any, in free text. The following question was also asked: “Considering the use of the Schizophrenia Functioning Core Set as a clinical assessment instrument, do you think that the ICF Environmental Factors should be included in the final rating of the person’s functional assessment?” In this case, the response options were: “It is of clinical interest and they should be part of the final rating of the functional assessment of the person with schizophrenia”; “It is of clinical interest, but they should be assessed separately since they do not assess factors related exclusively to the person” or “It is of no clinical interest and they should be eliminated.”
After analysing the results of the first round, adjustments were made to the criteria for classifying the categories, according to the suggestions, and the second round was carried out. The questionnaire for the second round was sent on October 20, 2020, to the 30 experts who participated in the first round, with a 2-week deadline for response.
Results
Development of Criteria for the Evaluation of the Degree of Functional Disability
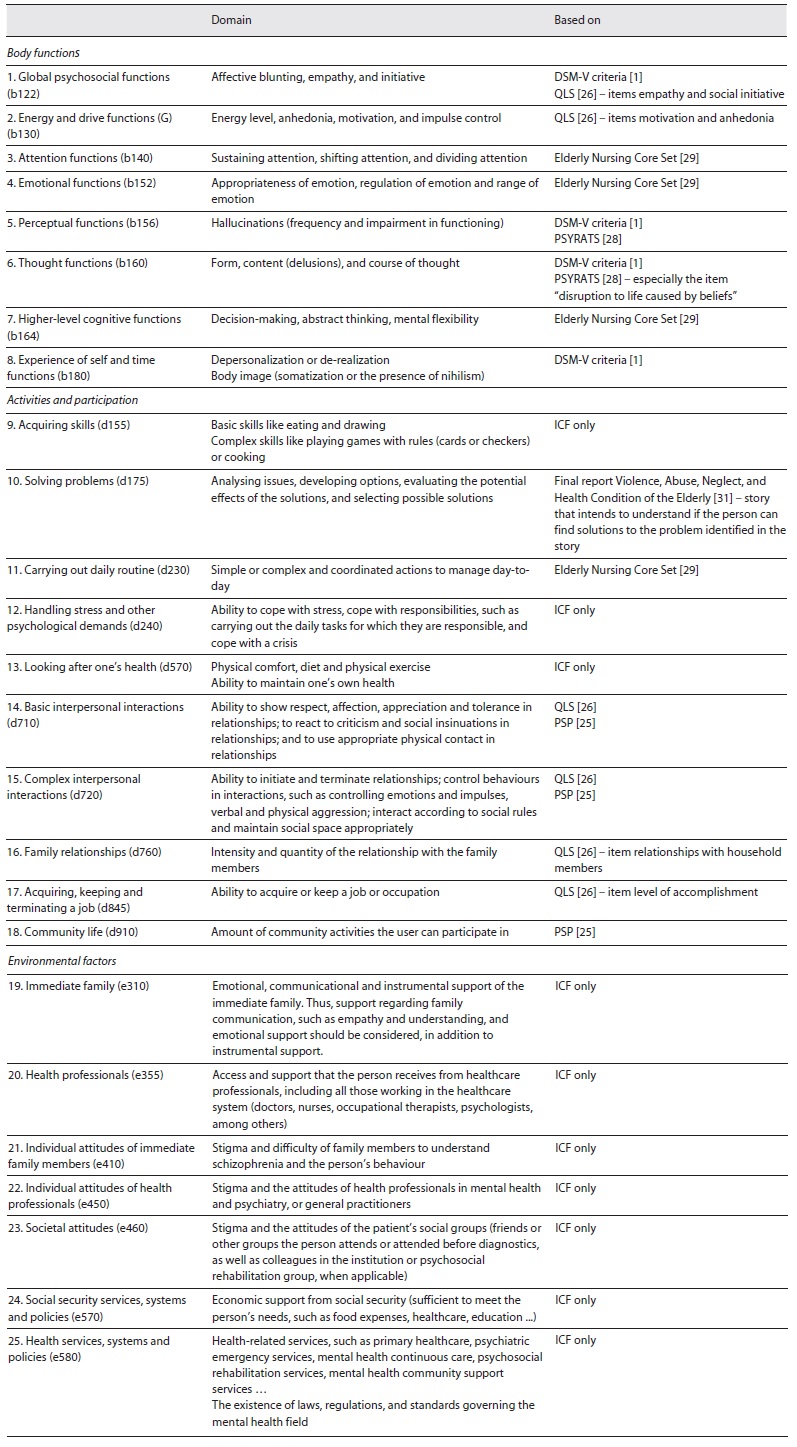
In developing the evaluation criteria for the Schizophrenia Functioning Core Set, the definition of each of the categories found in the ICF was respected. In the body functions and activities components, the definition of the degree of severity is related to the frequency and degree of impairment in functioning for the domain being assessed. Table 1 shows the domains that should be assessed in each of the items and the instruments we used to construct the rating criteria.
Modified e-Delphi Method
Thirty experts participated in the first round (participation rate of 68.2%), aged 27-62 years, with a mean age of 43.92 years (SD = 9.10). The academic qualifications of the experts were as follows: Bachelor’s degree (n = 7), Master’s degree (n = 21) and PhD (n = 2). Regarding profession, the results were as follows: psychopedagogue (n = 1), occupational therapists (n = 2), psychiatrists (n = 3), university professors (n = 4) and mental health and psychiatric nurses (n = 20).
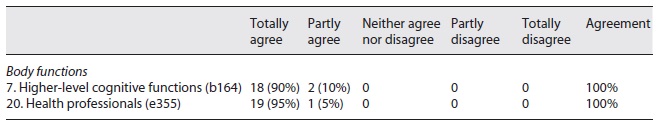
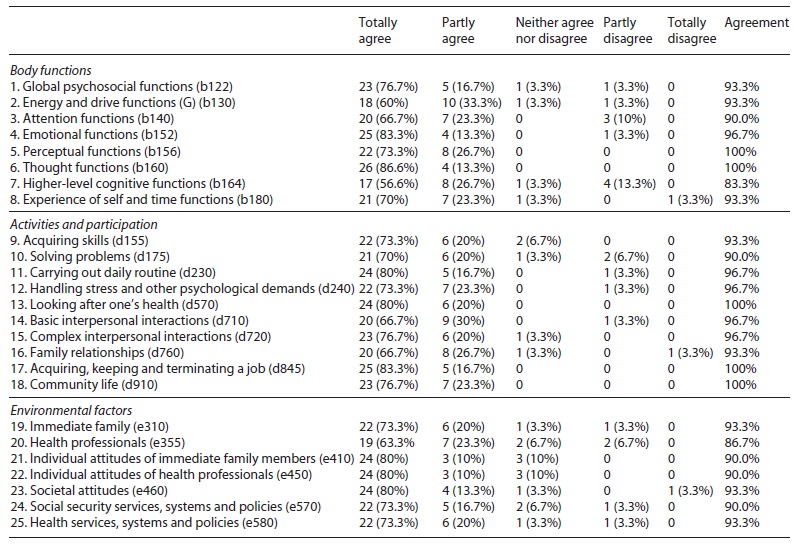
Table 2 shows the results of the responses from the first round, showing that all constructs had a degree of agreement (“totally agree” and “partially agree”) ≥90%, except for the constructs “(7) Higher-level cognitive functions (b164)” and “(20) Health professionals (e355).”
Table 2 Analysis of the experts’ answers to the first round of questions about the Schizophrenia Functioning Core Set
The last question obtained the following answers:
It is of no clinical interest and they should be eliminated: n = 1 (3.3%).
It is of clinical interest, but they should be assessed separately since they do not assess factors related exclusively to the person: n = 11 (36.7%).
It is of clinical interest and they should be part of the final rating of the functional assessment of the person with schizophrenia: n = 18 (60%).
The questions with a degree of agreement lower than 90%, as well as this last question, were submitted to the second round, with the participation of 20 experts. The results are shown in Table 3.
Regarding the question about environmental factors, 70% of the experts considered that it has clinical interest and should be part of the final rating of the functioning of the person with schizophrenia. The final instrument can be found in online supplementary Appendix 1 (see https://www.karger.com/doi/10.1159/000524422 for all online suppl. material).
Discussion
The Brief ICF Core Set for schizophrenia can be considered as a minimum standard to describe the functioning of the person with schizophrenia in any setting 22. Its utility is multifaceted, and it can be applied in clinical practice, for example, to support intervention planning or to define the goals of rehabilitation and patient care. It can also support health reporting and be used in research 22.
The definition of the categories for the Brief ICF Core Set for schizophrenia has produced a health tool that can contribute to a paradigm shift away from concentration on signs and symptoms to a more integrative perspective, considering not only the biomedical aspects of recovery but also the impact on activities and participation and factors related to the person’s environment 22.
With the definition of criteria for the assessment of the degree of disability in each of the categories performed in this study, we made its evaluation more rigorous, reducing the probability of a subjective evaluation that could be interpreted in different ways by different professionals.
The inclusion of environmental factors in the final rating of the functioning of the person with schizophrenia was the question that generated the most diversity of opinions, although the majority agreed that they should be included. Indeed, social and cultural contexts are still considered important forces that shape the experience of schizophrenia 31. Models of care for the person with schizophrenia should include improving the quality of family support, given the family’s influence on outcomes and their typical role as caregivers 32. Family psychoeducation is one of the interventions that can improve the quality of that support, allowing the family to have a deeper perception of schizophrenia 9. As far as other environmental factors are concerned, studies have shown that the higher the perception of social support or satisfaction with it, the better the effectivity and quality of life 33-36. It should be noted that the categories that assess family, health professional and societal attitudes evaluate the stigmatization of the person. Studies indicate that higher levels of internalized stigmatization are associated with decreased help-seeking behaviour and lower adherence to pharmacological and psychosocial treatment 37-39, which may worsen functioning and limit rehabilitation. Another study concluded that the greater the internalized stigma, the worse the functioning 40.
The limitations of this study are that all the experts who participated in the Delphi technique were Portuguese, and, therefore, the evaluation criteria are validated for application in Portugal. Nevertheless, they may be considered by other countries if they are suitable, since the Brief ICF Core Set for schizophrenia can be used internationally. It is necessary to adapt the environmental factors to each country.
Conclusion
The development of the Schizophrenia Functioning Core Set reduces the subjectivity in the assessment of the functioning of people with schizophrenia, standardizing the application of criteria to assign the degree of disability in each of the categories.
Mental health policies must focus on the psychosocial rehabilitation of people with severe mental disorders, such as schizophrenia, allowing for a decrease in the overall epidemiological and economic burden of the disease, providing a better quality of life for patients and their families. To this end, a paradigm shift is essential in health systems, starting to adopt integrated and continuous care focused on the person in his/her context. The assessment of functioning as presented in the Schizophrenia Functioning Core Set contributes to facilitating the assessment of the different categories of the Brief ICF Core Set for schizophrenia.
Acknowledgement
The authors would like to thank all experts who participated in the e-Delphi method.