Background
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disease (COVID-19) outbreak has posed a serious threat to global health 1, with an unprecedented impact on health, society, and the global economy 2. By January 31, 2022, the pandemic had resulted in more than 370 million confirmed cases and over 5.6 million deaths globally 3.
On March 2, 2020, Portugal registered the first case of contagion by SARS-CoV-2. Nine days later, on March 11, 2020, the date on which the World Health Organization (WHO) declared COVID-19 as a pandemic 4, the number of confirmed cases was 59. By the end of the year 2020, Portugal had 420,629 confirmed cases and 6,972 deaths 5. However, the beginning of 2021 was even more severe; by February 15, 2021, the number of confirmed cases has summed up to 788,561 and the number of deaths was 15,522 6.
The global economy suffered major disruptions, whose effects are expected to last for a long period 7, with direct implications for the health systems and society.
Health systems and hospitals around the world have adapted and reorganized to meet the challenges of this pandemic. We highlight, as an example, the increase in the capacity of intensive care unit (ICU) beds, the setting up of field hospitals, the creation of new circuits, and the development of COVID-19 units to isolate and treat infected patients, ensuring the safety of the diagnosis and treatment of patients without COVID-19 and of healthcare professionals 8. Along with the clinical and organisational challenges, hospitals and health systems have seen costs rise with the increased need to hire health professionals and to purchase and make available medical equipment (e.g., ventilators and protective personal equipment) for the treatment of COVID-19 patients 9. In addition, in many countries, hospitals had to cancel elective procedures, leading to revenue shortfalls 9.
These challenges have intensified financial pressures on health systems, and in particular in hospitals, whose financial capacity was already vulnerable.
The National Health Service (NHS) is the main healthcare system in Portugal (which coexists with health subsystems and private health insurances) and is predominantly financed by taxes. The NHS financing system is processed through the Ministry of Finance, which annually sets a budget for health, essentially based on the expenditure history. The budget is then distributed by NHS institutions through the Central Administration of the Health System and Regional Agencies using a prospective contracting model. The inpatient production reimbursement of NHS hospitals is, generally, determined by the base price set under the commissioning contract multiplied by the average case-mix of the specific institution 10.
The COVID-19 pandemic has occurred during a period of unprecedented financial pressure on the NHS in Portugal. In the first quarter of 2020, debt overdue for more than 90 days (arrears) by the 54 health entities of the Portuguese NHS was over 169 million EUR (corresponding to 11.9% of total debts to external suppliers, which amounted to 1.4 billion EUR), alongside an average payment period to suppliers of 138 days 11. In August 2020, the debt overdue for more than 90 days had increased by over 292 million EUR (corresponding to 19.4% of total debts to external suppliers, which amounted to 1.5 billion EUR). Studies published so far tend to examine out-of-pocket or the additional cost that insurers pay for COVID-19 admissions; few have assessed the financial impact on health systems 12).
Knowing the financial impact of the COVID-19 pandemic on the health system is essential to inform and support policymakers on possible adjustments of budgets dedicated to health systems and in particular to hospitals. In this context, this study aimed to characterize the cost of admissions by COVID-19 patients in a Portuguese hospital.
Methods
Study Design, Data Sources, and Selection Criteria
In this observational study, we have characterized the cost of COVID-19 inpatient admissions. We used data from inpatient admissions in a Portuguese Tertiary Care University Centre between March 1, 2020 and May 31, 2020. This tertiary hospital centre, the second biggest in the country, is located in Lisbon and is composed of six hospitals: two are dedicated to maternal and child care, one to cardiovascular pathologies, and three to general typology for adult care. It delivers multipurpose emergency care for adults, paediatrics, and obstetric-gynaecological, and provides healthcare in various medical and surgical specialities. This hospital centre has around 1,300 beds and an average of 3,900 inpatient admissions per month. The catchment population varies from 284 thousand to 1.8 million, depending on the medical speciality. It also serves as a backup to other hospitals with a lower level of specialisation.
We constructed a database that initially contained summary data of 330 pseudonymised inpatients diagnosed with COVID-19, including information such as diagnosis and procedures coded according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), sex, age, length of stay, and discharge disposition.
We have excluded admissions from patients under 18 years old, admissions with incomplete records (missing Diagnosis Related Group [DRG]), admissions from patients who had been transferred to or from other hospitals, or those whose inpatient stay was under 24 h. Pregnancy, childbirth, and puerperium admissions were also excluded, as well as admissions from patients who had undergone surgery. The final sample contained 223 admissions, which represented 2.4% of the total admissions during this period of analysis. There were 21% of episodes that were not coded, therefore we estimate that, in this period, the total COVID-19 admissions (without any exclusion criteria) corresponded to 4.6% of the total number of admissions.
Variables
The outcome of interest was the cost of COVID-19 admissions.
A COVID-19 admission was defined if the principal diagnosis code U07.1 from ICD-10-CM was present. This code was created exclusively for COVID-19 confirmed cases 13.
To estimate the cost of each inpatient admission, regarding diagnostic and therapeutic procedures, Ordinance No. 254/2018 was used. This ordinance approves the Regulations and Price Tables of Institutions and Services Integrated into the NHS, proceeds to the regulation of the Integrated Management System for Registrants for Surgery, and sets the prices and conditions under which the additional activity is carried out by clinical teams 14. To estimate the cost of inpatient medicine consumption, we considered all the medicines that were administered to the patient by a direct assignment. The value of medications was based on the average purchase price.
Regarding the costs related to clinical consumables, personal expenses, and indirect costs, without the possibility to direct assignment per episode, we obtained the unit costs based on the calculation of direct costs of the different cost centres. The expenses directly attributed to the patient (medicine consumption and diagnostic and therapeutic procedures) were excluded from these direct costs. Indirect costs (expenses with the operation of some clinical support services across the various units, and expenses with general support services and administration) were shared by higher-level cost centres based on their value (homogeneous sections method approach). After calculating the direct and indirect expenses (total expenses), these were divided by the work units of each cost centre and allocated to the patient according to the number of days of hospitalisation. Similarly, regarding the determination of these costs to the emergency department, they were allocated to each episode by dividing the total amount of costs by the total of episodes.
Data Analysis
We characterized admissions by sex, age group, presence of chronic obstructive pulmonary disease (COPD), diabetes or hypertension as a secondary diagnosis, Comorbidity Charlson Index, admission at ICU, and hospital mortality. The characterization of COPD, diabetes, and hypertension is related to the fact that these pathologies are among the most common comorbidities of COVID-19 hospitalized patients (15, 16).
We also estimated the average length of hospital stay, the length of stay at ICU (for patients admitted at ICU), and the cost per admission. We also analysed the distribution of costs per financial rubric: emergency department, medicines, diagnostic and therapeutic procedures, clinical consumables, human resources (HR), other direct costs, and indirect costs.
Since most COVID-19 admissions were assigned to the DRG 723 (Viral Illness), the length of hospital stay and cost per admission by the severity of illness was also the subject of analysis. The DRG classifies admissions in four levels of severity: minor, moderate, major, and extreme.
For continuous variables, we reported means with standard deviations and medians with interquartile ranges, and for categorical variables, we reported absolute numbers and percentages.
Descriptive analyses were performed using R (version 4.0.3).
Results
We identified 223 patients diagnosed with COVID-19. Although not all COVID-19 admissions were coded, these represent 2.4% of the total admissions during the study period.
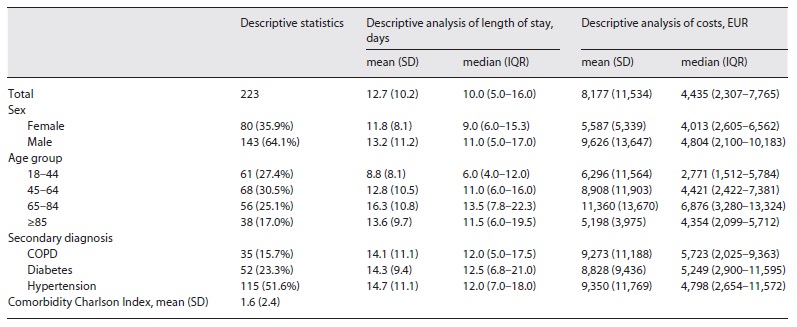
Table 1 summarizes the description of COVID-19 admissions. The average length of hospital stay was 12.7 days (SD = 10.2) and the average cost per admission was EUR 8,177 (SD = 11,534). Twenty-one patients (9.4% of the admissions) had an estimated cost per admission greater than EUR 20,000, accounting for 44% of the total costs.
Most admitted patients were men (64.1%) and aged 45-64 years (30.5%). 51.6% of the patients admitted were diagnosed with hypertension and 23.3% with diabetes.
On average, men were hospitalized for a longer period (M = 13.2 days, SD = 11.2), associated with a higher average cost per admission (M = EUR 9,626, SD = 13,647), when compared to women. The age group that had the higher length of hospital stay and cost per admission is 65-84 years old (M = 16.3 days, SD = 10.8).
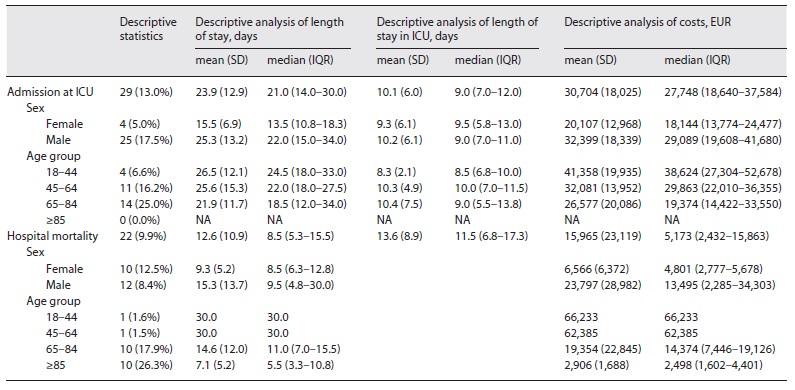
As shown in Table 2, around 13% of patients diagnosed with COVID-19 were admitted to ICU, with men accounting for 17.5% and patients aged 65-84 years accounting for 25.0%. Among the patients admitted at ICU, men showed a higher average length of hospital stay (M = 25.3 days, SD = 13.2), higher average length of stay in ICU (M = 10.2 days, SD = 6.1), and higher average cost per admission (M = EUR 32,399; SD = 18,339), when compared to women. Patients aged 18-44 years admitted at ICU had the highest average length of hospital stay (M = 26.5 days, SD = 12.1) and cost per admission (M = EUR 41,358, SD = 19,935). However, patients aged 65-84 years presented the highest average length of stay in ICU (M = 10.4 days, SD = 7.5).
The hospital mortality rate among COVID-19 patients was 9.9%, with a higher prevalence in women (12.5%) and patients aged 65 years or older. Patients with COVID-19 who died at the hospital were hospitalized on average 12.6 days (SD = 10.9) with an average cost per admission of EUR 15,965 (SD = 23,119). Patients who were admitted to ICU and died were on average 13.6 days (SD = 8.9) in the unit.
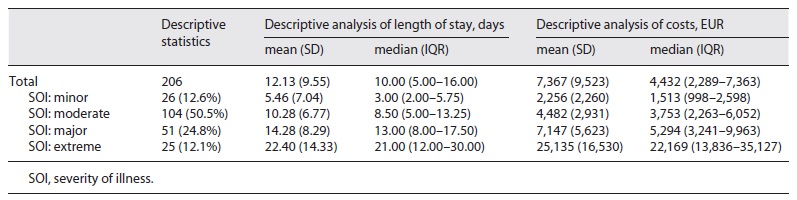
Of the 223 admissions, 206 (92.4%) were assigned to the DRG 723 (Viral Illness). Table 3 shows the descriptive statistics and analysis of COVID-19 admissions coded DRG 723. An increase in the average length of hospital stay and the average cost per admission according to the increase in the severity of illness was observed. On average the cost per admission coded as minor severity of illness was EUR 2,256 (SD = 2,260), while the cost per admission of those coded as extreme severity of illness was EUR 25,135 (SD = 16,530).
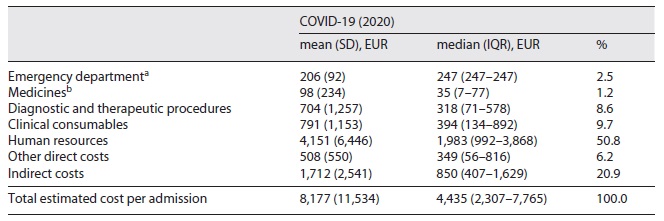
As shown in Table 4, the highest proportion of the total costs in COVID-19 admissions was in human resources, accounting for 50.8% of the total, with an average cost per admission of EUR 4,151 (SD = 6,446). The clinical consumables accounted for 9.7% of the total costs, with an average cost per admission of EUR 791 (SD = 1,153). The financial rubric that accounted for the lower cost was medicines (M = EUR 98, SD = 234).
Discussion
In this study, we have characterized the cost of COVID-19 admissions in a tertiary hospital centre in Portugal.
We considered 223 patients admitted with a diagnosis of COVID-19, between March 1, 2020 and May 31, 2020. Our results indicate that these admissions involved high costs for the NHS. The average cost per admission was EUR 8,177 (SD = 11,534) and the median cost per admission (by any patient) was EUR 4,435 (2,307-7,765). These results are lower than those reported in the international literature. For example, a study in the Kingdom of Saudi Arabia 12 found a median cost of EUR 8,979 (6,958-12,193) and a study in the USA 17 reported a median cost of EUR 12,585 (11,865-13,253).
The differences in the reported costs between studies may be related to the costing methodology used and also, as highlighted by Khan et al. 12, by the significant differences in the cost of treatment protocols, personnel costs, and utilization rates of healthcare resources and their prices between countries, which complicate the estimation and comparison of direct medical costs globally.
When we analysed the median cost per admission by age group and compared it with the Bartsch et al. 17 study, we found that patients aged 85 years or older had the lowest cost (EUR 2,498 [1,602-4,401] in our study, and EUR 10,424 [9,714-11,243] in the Bartsch et al. study). Bartsch et al. 17 explained the lower costs per admission of 85-year-old or older patients by the fact that a person of this age has a lower probability of ICU admission, which is also observed in our sample since there is no record of admission to the ICU for patients aged 85 or older.
The rate of patients with COVID-19 treated in the ICU was 13.0%, which is similar to the 14.2% reported by Richardson and colleagues (15). At the beginning of the pandemic, the WHO estimated that about 15% of patients infected with COVID-19 would have severe disease that requires oxygen therapy or other inpatient interventions; and about 5% would have a critical disease that requires mechanical ventilation 18.
The average length of hospital stay for COVID-19 patients was 12.7 days (SD = 10.2) and for the patients admitted to ICU, the average length of stay at ICU was 10.1 days (SD = 6.0). Our results regarding the length of hospital stay and ICU length of stay are consistent with the literature, which indicates a median duration ranging from 5 to 29 days and 5 to 19 days, respectively 19.
The hospital mortality rate of COVID-19 patients (9.9%) was lower than the rates found in the literature, which are over 20% 15,16. We hypothesize that this difference may be related to the fact that our sample only includes admissions codified, leaving out of the analysis a significant number of patients who were admitted during the period under analysis.
In our findings, 92.4% of the admissions were assigned on the DRG 723 (Viral Illness). According to Ordinance No. 254/2018, the price for inpatients whose admission is assigned on the DRG 723, is EUR 575.36 for minor SOI, EUR 896.86 for moderate SOI, EUR 2,063.8 for major SOI, and EUR 9,283.73 for extreme SOI. These prices are lower than those we assessed in our findings, namely EUR 2,256 (SD = 2,260), EUR 4,482 (SD = 2,931), EUR 7,147 (SD = 5,623), and EUR 25,135 (SD = 16,530), respectively. These findings may highlight the need to readjust the DRG prices to incorporate the costs with COVID-19 inpatients.
Our findings show that the highest proportion of the total costs in COVID-19 admissions were human resources, which may be related to two main strategic decisions: on March 16 (15 days after the first hospitalization in Portugal), the Government determined the suspension of non-urgent assistance activity (effective until May 2); the NHS hospitals started to reinforce the pool of human resources to face the pandemic. Thus, a decrease in efficiency is expected, as a result of the increased cost of HR and the decrease in hospitalizations (units of production). The dimension of this inefficiency is not known until this time.
According to the data available, at a national level, the rate of hospitalization for confirmed cases of COVID-19 was around 13% to 16% in the period of this study. This rate is in line with the literature that indicates a 14% hospitalization rate of COVID-19 patients in the first year of the pandemic 20. Assuming a 13% to 16% hospitalization rate, we can estimate that in Portugal, until the end of the year 2020, between 54,682 to 67,301 patients were admitted to hospitals, which results in a global cost of around 447 to 550 million EUR with admissions by COVID-19 patients.
According to Ordinance No. 254/2018, the inpatient base price, which is a proxy for the cost of admission with a relative weight of 1, is EUR 2,285. This price, updated by the relative weight of 2018 admissions (1.0444), is EUR 2,386. Thus, considering the 447 to 550 million EUR spent on COVID-19 admissions, it would have been possible to treat 187,363 to 230,600 patients, which means that for each COVID-19 inpatient it would have been possible to treat three patients hospitalized for other causes.
In addition, the direct costs associated with the measures to recover unattended care activity will have a significant financial impact. In this context, on June 6, 2020, the Economic and Social Stabilization Program was published in the Portuguese official gazette 21. Within this Program, which has foreseen measures to reinforce the NHS, an amount of around 100 million EUR was estimated, of which 33.7 million EUR for the recovery of 25% of surgical activity and all lost first consultation activity. This program also includes infrastructural investments that allow the expansion of intensive care services, the hiring of health professionals, and the purchase of computer equipment.
Beyond the financial impact, the COVID-19 pandemic has and will have long-lasting consequences on the health system and the health of populations, not only related to the complications of this disease but also by the disruptions of care for thousands of patients without COVID-19, including the cancellation and postponement of non-urgent care and the mistrust and avoidance of healthcare services by patients 22,23.
Given the proven benefits of home-based hospitalization on better outcomes and lower costs, this delivery of care model has been pointed out as the best possible solution to reduce the spread of the virus and maintain the health of patients who need a hospital stay 24,25. Thereby, home-based hospitalization, similarly to remote appointments, presents a way to mitigate the negative impact of this pandemic on the health of the population.
There are several limitations to our study. The main limitations relate to the sub-coding of 2020 admissions and the fact that the study only included data from patients admitted to a single hospital, reflecting its current structure and resource consumption options, so different costs may be incurred in different hospitals with differing characteristics to that studied. The costing methodology is another limitation, as it was not possible to determine direct inpatient costs per patient, only a median cost based on the allocation to cost centres. The indirect costing approach used only permits a small level of cost disaggregation without linkage between cost centres and standardized production centres 10.
Other limitations to our study include that it only focuses on the initial wave of the COVID-19 pandemic. New policy and treatment options that have been adopted throughout the pandemic are not captured here (such as the opening of new beds, human resources mobilization, and new therapeutic approaches). The COVID-19 variants that emerged had distinct clinical characteristics that could have led to different costs. Vaccines started to be administered in Portugal in December 2020, and it is reasonable to assume that it would take six months or more to see any impact on the costs of hospitalizations. Expanding the analysis to more than the initial three months would allow us to visualize possible changes in costs and associate them with the progress of the pandemic; in this sense, choosing a short period right at the beginning of the pandemic is a limitation of this study. Nonetheless, our results provide an insight into the initial direct financial impact of the pandemic and give perspective to the cost associated with possible future pandemics similar to COVID-19.
This study did not capture broader financial impacts of COVID-19 on the health system as we did not include information such as the additional costs in primary healthcare or long-term care, vaccination costs, contract costs with the private sector (especially costs with tests for COVID-19 detection and treatment of COVID-19 and non-COVID-19 patients), and post-discharge costs for associated healthcare use (e.g., additional admissions, outpatient visits, rehabilitation). It also did not focus on the economic impact of COVID-19 since it did not take into consideration other costs, such as productivity losses.
However, this is, to the best of our knowledge, the first study to assess COVID-19 admission costs, making an important contribution to supporting the decision-making process, regarding the financing of health institutions in the current context.
Regardless of the contributions of the present study, we consider it is crucial to analyse data of a longer period, in particular, due to changes in the therapeutic approaches observed from the first to the subsequent waves of the pandemic. We also consider that it could be a great contribution if future studies contemplate a more comprehensive approach, analysing the costs of emergency visits without hospitalization; day hospital care and outpatient consultation. We also suggest that further studies compare COVID-19 admissions with non-COVID-19 admissions, and the post-2019 non-COVID-19 admissions to 2019 non-COVID-19 admissions, since, during the pandemic, it is expected to have an increased cost of clinical consumables, even for the treatment of non-COVID-19 patients.
Conclusions
In conclusion, our results demonstrate a substantial financial burden associated with COVID-19 admissions. Moreover, the price set for DRG 723 (Viral Illness) admissions is not adjusted to the cost of COVID-19 patients. These findings highlight the need for financial reinforcement of health institutions, in particular those that had treated COVID-19 patients.
Our findings also underline the need to consider the cost opportunity of COVID-19 admissions, once this pathology has taken precedence over other pathologies.
Acknowledgements
The authors are grateful to Centro Hospitalar Universitário Lisboa Central, E.P.E. for the data provided and to NOVA National School of Public Health, Universidade NOVA Lisboa, in particular to Professor Baltazar Nunes for the contributions regarding data analysis. The authors would also like to express their gratitude to Paulo Espiga and Professor Fernando Maltez for the important insights and for willingly sharing their experiences.
Statement of Ethics
Consent to participate is not applicable since pseudonymised inpatient data was used in the study. The utilization of the data was approved by Centro Hospitalar Universitário Lisboa Central, E.P.E. (study design proposal approved by the Ethics Committee).