Introduction
The American Academy of Pediatric Dentistry (AAPD) defines special healthcare needs as “any physical, developmental, mental, sensory behavioral, cognitive, or emotional impairment or limiting condition that requires medical management, health care intervention, and/or use of specialized services or programs” 1. Evidence suggests that patients with special needs are at an increased likelihood of oral diseases 2. This requires dentists and dental team members to tailor the expertise to individual patients with special needs.
In Trinidad and Tobago, the findings of the most recent national census indicate that there are over 52,243 persons living with a disability 3. The School of Dentistry of The University of the West Indies (SoD) has a dedicated special needs clinic (SNC) that addresses the dental needs of patients with special needs as part of a competency-based curriculum for the training of dental students. At this clinic, patients with varying degrees of intellectual, developmental, and physical disabilities are treated for urgent or episodic issues or dental needs are approached comprehensively. Patients/guardians presenting for urgent and episodic care are encouraged to return for comprehensive treatment. Comprehensive treatment planning would normally happen after intervention either through pharmacological means or dental treatment to alleviate the signs and symptoms of acute disease. Anecdotal evidence based on the appointment schedules of these patients suggested that many patients would attend only for urgent or episodic problems, with a smaller proportion of patients having comprehensive dental management.
Many persons with special needs frequently experience barriers to oral health care. Barriers noted in a review of the literature include cost, fear or anxiety, the perceived need for care, location and distance to health facilities, and waiting time 4.
The aims of this study were to (1) determine the treatment needs of patients with special needs attending a dental teaching hospital, (2) determine the unmet need (treatment gap) in treatment provided compared to treatment planned for patients with special needs, (3) investigate the barriers to the completion of planned treatment for patients with special needs.
Materials and Methods
A retrospective chart audit of paper-based dental records was conducted of patients attending the SNC of the SoD in the period from August 1, 2015 to July 31, 2017. The University’s Ethics Committee granted an exemption to ethical approval (CEC769/11/18). Individual records were included in this retrospective audit once the following inclusion criteria were met: a recorded medical history inclusive of the patient’s disability, a comprehensive treatment plan, working telephone contact included in the records, and a patient/guardian who was willing to give consent via telephone for a short interview by the principal investigator. Charts were not included for audit if the patient or guardian could not be reached via telephone or no comprehensive treatment plan was completed for the patient.
Treatment needs were assessed by review of recorded treatment plans. Treatment notes were used to ascertain how much treatment was completed. Treatment notes were used to identify the difference between planned treatment and the completed period over the selected period. Comprehensive treatment plans were dissected to understand the relative proportions of various types of treatment required, such as continued urgent care, preventive and restorative treatment.
Urgent treatment in this setting included procedures that alleviate pain, infection, and discomfort, such as extraction, pulpal extirpation, and prescription of antibiotics and/or analgesics. Preventive treatment included oral hygiene instructions and dietary advice to the patient and/or guardian, scaling, fluoride application, and the placement of fissure sealants. Restorative treatment was further parsed into operative treatment to manage dental caries, endodontic, periodontic, fixed and removal prosthodontic treatment. The number of patients requiring a certain type of treatment was calculated as a percentage of the total number of patient records audited. Completed treatment was calculated as a percentage of a particular type of treatment completed of the total number of records audited. The measured outcomes of interest were (1) type of treatment planned and (2) unmet treatment, i.e., treatment not received.
Barriers to care were assessed using a short telephone interview format, with one open-ended question, “What prevented you from returning to the Special Needs Clinic?” to ascertain the reasons for not returning to the clinic to complete care of the planned treatment. The answers were recorded and categorized into main barriers of cost, accessibility, psychosocial issues, dental knowledge, perceived clinical competence, and other reasons. Patients/guardians were allowed to state more than one reason for not returning for treatment. Individual answers were collated and presented as percentages relative to the total number of patients/guardians interviewed.
Data was entered into Statistical Package for Social Sciences (SPSS) version 27. Frequency distributions were used to rank types of treatment needs and self-reported barriers to care. A non-parametric McNemar change test for related samples at an alpha level of 0.05 was used to ascertain if there were significant differences between treatment required and treatment provided for specific types of treatment (unmet treatment).
Results
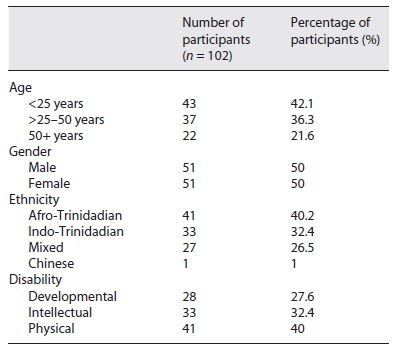
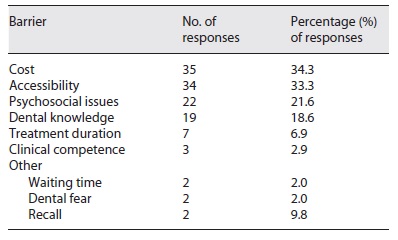
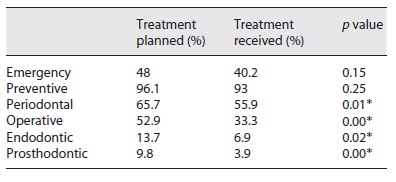
Of the 300 files assessed during the review period, only 102 charts (34%) met the inclusion criteria. The remainder of patients either could not be contacted (54%) or only received urgent treatment (12%). The age of patients in this audited sample ranged from 7 to 82 years. Table 1 shows the demographic information and types of disabilities of the patients whose records were audited. Table 2 shows the percentages of types of treatment planned versus the percentages of treatment received together with significance. When types of treatment were ranked, most patients required preventive treatment followed by periodontal, restorative, and urgent care in that order. Endodontics and prosthodontics - fixed or removable - were treatments least planned for patients with special needs. Table 3 lists the percentages of self-reported barriers described by patients/guardians in completing dental treatment at the clinic. Major identified barriers to accessing continued care at this clinic included cost, accessibility, and psychosocial issues.
Table 2 Percentage of patients showing treatment planned vs. treatment received together with significances (p values with asterisks indicate significances between planned and received treatment)
Discussion
Clinical audits can measure patient outcomes and facilitate quality improvement in healthcare. Dentistry has followed the lead of medicine and used clinical audit as a measure to ensure that care is being provided in line with best care standards 5. Specifically, clinical chart audits can ensure that quality improvements in patient management are continuous and align with quality care for all patients 6.
Within the competency-based curriculum, at the SoD students are taught to comprehensively manage the dental needs of patients holistically, taking into consideration other factors such as the medical and social health of the patient. Within the clinical teaching curriculum, all patients should be planned for comprehensive treatment or encouraged to return for comprehensive treatment planning and care.
This clinical audit of treatment plans for patients with special needs revealed that preventive treatment was planned for most patients attending the clinic. Vozza et al. discuss the general principles of health promotion and disease prevention when individualized risk assessment is taken into consideration 7. Comprehensive treatment planning for patients with special needs that incorporates risk assessment in formulating treatment plans including prevention can facilitate acceptance of treatment plans by patients and guardians. The audit revealed that most patients who had been planned to receive preventive care did have such care delivered. This augurs well for this population being studied given that recent evidence suggests that persons with special needs continue to demonstrate a high risk for the development of oral diseases 8. This is evidenced by high prevalence rates of oral diseases ranging from 48 to 67% depending on age 8. Preventive treatment in a population of patients with special needs would most likely also have higher rates of acceptance amongst both patients and guardians, similar to a population of younger children, given the noninvasive nature of preventive treatment strategies 9. It would be particularly relevant for the groups of patients with intellectual disabilities who have higher reported issues in dealing with dental procedures 10.
There was no statistically significant difference between patients who had planned and received future urgent care. This meant that most patients requiring future urgent treatment received such treatment. This contrasts with reported literature, where many patients with developmental and intellectual disabilities require urgent management under general anesthetic due to a lack of cooperation with dental personnel 11,12. This could be explained by the sample of patients under review. Patients with physical disabilities are more likely to be cooperative compared to those with intellectual disabilities to sit for comprehensive examination and treatment planning. This statistical non-significance between planned and received urgent care could be attributed to the relatively high percentage of persons (40%) with physical disabilities only in this sample.
The treatment needs of this audited population align with that of other studies and local populations of patients with special needs 13. This audit confirmed that patients with special needs had treatment needs consistent with high rates of caries and periodontal disease 14. Statistically significant differences were noted in planned and received treatment for operative dentistry, periodontics, endodontics, and prosthodontics, meaning that such planned treatment was not received. Generally, special needs patients with developmental or intellectual disabilities receive restorative care such as placement of restorations and periodontal management under general anesthesia 15. In this clinical audit, patients with intellectual and developmental disabilities accounted for 60% of patients with special needs. At the SoD teaching hospital, services requiring general anesthesia are not readily available for patients with special needs and dental services under general anesthesia must be rationalized within a wider and under-resourced hospital setting in terms of operating room availability and trained anesthetists.
Significant observations in unmet need could also be attributed to self-reported barriers to access continued care. Cost of care was reported as the main self-reported barrier. Although the cost of dental services at the SoD is heavily subsidized as compared to treatment at private dental offices, 34.5% of patients still found that the cost was prohibitive. Some parents and patients noted the lack of insurance and government assistance/grants made it impossible to pay for patient care or prioritize over medical health care. This is in contrast to other jurisdictions where dental management of patients with special needs is fully funded by government agencies 16.
Approximately one-third of the respondents indicated that accessibility was a major challenge, specifically the distance to the clinical facilities, cost of transportation, and lack of transport. This is in keeping with the work of de Gutierrez et al., who suggested certain patients with special needs, such as those with cerebral palsy, report greater physical barriers in accessing dental care 17. de Gutierrez, however, did not find transportation to be a major barrier to accessing dental care by patients with special needs 17.
Psychosocial issues were identified in 21.6% of respondents as a barrier to continuing treatment. These issues may be defined as concerns involving or relating to both the social and psychological aspects of a patient’s and/or guardian’s life such as occupational or financial stress or perceptions of need 18. Patients and guardians stated illnesses, lack of time off from work, no familial support system, and dental fear or patient behavior as some of the psychosocial issues which prevented them from returning for treatment.
Exactly 18.6% of respondents to the telephone interview reported unawareness that further treatment was planned or did not understand the importance of further planned dental care. This highlights the importance of communication with patients and caregivers regarding holistic dental management. Communication must also include oral health education and promotion with an emphasis on the importance of returning for continued care to mitigate against further severe disease.
Only a small proportion of respondents listed dissatisfaction with the perceived clinical competence of dental students, interns, or dentists providing treatment. This could be related to the fact that care happens within the confines of a teaching hospital. Dental management of patients with special needs within the SoD is facilitated mainly with the use of behavioral management and modification of treatment strategies. Since students themselves are now learning these strategies, patient management can take long periods. The exposure of dental students to patients with special needs in the undergraduate curriculum however can improve future access of patients with special needs to dental care 19.
Limitations of the study include the use of a non-probability or convenience sample of patients attending a single clinic. Such sampling frameworks can reduce the external validity of the study and not make the study’s findings broadly generalizable to the wider population. Since only 34% of all available charts were included for audit based on the inclusion criteria this could lead to selection bias. In this instance given that the sample of patients being reviewed formed less than half of all patients seen during this period, a true and complete representation of perceived barriers was not captured by this research. For this reason, the authors suspect that unmet dental treatment need is much higher and additional identified barriers of care could be uncovered. Future research should focus on assessing the treatment needs and perceived barriers to care of a greater proportion of patients attending the SNC.
Conclusions
This retrospective chart audit revealed that patients with special needs attending the SoD for dental treatment had mainly preventive and urgent treatment completed at the SNC. There was an unmet need for restorative and periodontal treatment. Major self-reported barriers to dental care included cost, accessibility to care in terms of transportation issues, and psychosocial issues. Provision of preventive care can mitigate against the development of future dental disease; however, strategies need to be developed to understand how other identified treatment needs of patients with special needs can be addressed to alleviate disease progression
Statement of Ethics
The study protocol was reviewed by the Ethics Committee of The University of the West Indies, St. Augustine and granted an exemption from requiring full ethical approval (CEC769/11/18). Approval was given to obtain the verbal consent of respondents for the short telephone interview.
Data Availability Statement
The data that supports this work can be found at the data repository, Harvard Dataverse: https://doi.org/10.7910/DVN/HCMEQQ.