Introduction
Quality of care has become an international priority 1. This is due to evidence that poor-quality health services are restricting progress in improving health in countries at all income levels 2. One of the aspects or dimensions of quality in health services, and an important contribution to this problem, is patient safety (PS). Adverse events due to unsafe healthcare represent a major source of morbidity and mortality globally 3-5.
The evident relevance of PS for health outcomes has prompted a considerable array of initiatives both at international, national, and local levels, aimed to raise awareness of the problem and improve PS practices. The promotion of PS culture (PSC) and the creation of an infrastructure for PS are two of the possible initiatives that are common and transversal for any PS program. It is assumed that PSC may facilitate adherence to good safety practices and lead to a reduction of adverse events 6,7. According to the National Quality Forum (NQF), promoting PSC in healthcare settings includes the following four interventions: (1) implementing structures and leadership systems to promote PSC. These leaders, in turn, should (2) monitor the level of PSC, publish its results, and conduct opportune interventions; (3) educate health professionals regarding the acquisition of safety and teamwork skills; and (4) identify and continuously reduce the risks and hazards present in healthcare.
PSC can be defined as an individual or collective set of values, attitudes, perceptions, competencies, and behavioral standards that determine the commitment, style, and competence of a health organization in promoting safety 8. PSC involves overcoming the culture of blaming individuals in the face of PS incidents and adopting a culture that favors a systemic approach 9. This approach recognizes that the main factors related to errors and adverse events are the structure of health organizations and their operating processes, and it is necessary to insert barriers to reduce their probability of occurrence 10. The measurement and improvement of PSC have thus become a good practice standard for PS, but like many other actions for PS, its effective implementation remains problematic. A systematic review shows that the available studies are heterogenic in terms of interventions and types of reported results, demonstrating the need for new studies on interventions to improve PSC 11. Moreover, regarding other areas of quality in general and PS in particular, most studies are at the local level. Few studies seek to assess the effect of national program 12. The literature on health services research in Brazil has assessments of PSC 13 describing the situation but without discussing improvements or interventions to improve. Therefore, empirical evidence on the effectiveness of interventions in improving PSC remains weak, particularly concerning external initiatives that must be considered by public policymakers, stakeholders, and health system managers.
In 2013, the Brazilian government implemented the National Patient Safety Program (NPSP) which aimed to improve the quality of care, PS infrastructure, and the PSC 14. The NPSP promoted actions in line with the NQF recommendations. However, implementation in hospitals has been variable and has not been assessed. This study observes and describes the changes in the specific structure for PS and PSC survey results at three Brazilian hospitals, before and 15 months after the NPSP was launched.
Methodology
Design
An observational, longitudinal, and descriptive study with two assessments of the PSC in three hospitals, one carried out 6 months before and another 15 months after the launch of the NPSP (in April 2013), was conducted. Therefore, the study period, in which changes in the structure of PS were monitored, ranged from November 2012 to June 2015.
Context
The study was conducted in three selected hospitals (one state hospital [SH], one federal hospital [FH], and one private hospital [PH]) in the state of Rio Grande do Norte (RN). RN is situated in northeastern Brazil and is ranked eighteenth in gross domestic product out of 26 states and the Federal District (capital of Brazil), with a human development index of 0.684 (considered medium), slightly below the Brazilian average (0.727) 15.
The SH is a 270-bed public hospital, the largest of the 24 SHs in RN. It has an emergency department and is a regional referral center for traumatology.
The FH is also the largest of the four federal facilities in RN. It is a 242-bed university hospital owned by the federal government. Unlike the SH, it does not have an emergency department.
The PH is one of the three largest hospitals in this category in RN. It is an 86-bed general hospital managed by a medical cooperative, with an emergency department. Its target population is middle-class citizens with health insurance, and it does not treat patients from the National Health System (SUS). The PH was the only hospital in the state with a seal of accreditation, awarded in 2012 (just a few months before our first PSC assessment). The accreditation was at level 1, the lowest of the three levels awarded by the Organização Nacional de Acreditação (National Organization of Accreditation). Accreditation level 1 is awarded when compliance with the accreditation standards is at least 70% 16.
The NPSP is a federal system-wide initiative to improve PS. It was established by the Brazilian Ministry of Health in April 2013, translated to norms, and regulated by the National Health Regulatory Agency (Anvisa) on July 25, 2013, and made mandatory on January 25, 2014. The objectives of the NPSP 14 are to (1) promote safe healthcare by creating PS units (PSUs) at health facilities, establish PS strategies, implement PS protocols, and adhere to a mandatory adverse event notification system. It is the instance of the health service created to promote and support the implementation of actions aimed at PS. (2) Involve citizens in their safety; (3) include PS in the curriculum for health professionals; and (4) increase patient health safety research. One of the NPSP’s explicit strategies under objective 1 is to promote a culture of safety. Other actions of objective 1 include having a PS plan (PSP), implementing protocols for patient identification, safe medication, safe surgery, hand hygiene, fall prevention, pressure ulcer prevention, training on PS, health surveillance, incident reporting, patient identification, and drug identification.
Participants
Three selected hospitals and their staff representing the three main types of hospital ownership in Brazil (public state, public federal, and private) participated. The participating institutions were chosen for being hospital references in the region, for presenting data about PSC before the implementation of the NPSP, as well as for carrying out internal changes based on the NPSP.
Data Collection
Changes in Unit Infrastructure and Actions for PS
We inquired of the hospital management (clinical director) about the implementation of the organizational changes proposed in the NPSP (namely the establishment of a PSU, PS incident reporting (PSIR), and PSP) as well as the recommended protocols and training activities on PS (PS protocols: patient identification, safe medication, safe surgery, hand hygiene, falls prevention, pressure ulcer prevention; training for PS topics: PS, health surveillance and incident reporting, patient and/or drug identification). The period of inquiry was from the onset of the study (first PSC measurement, before the launch of the NPSP) to the second measurement of PSC (15 months after the NPSP became mandatory).
The variables used to characterize the sample of respondents were years in the profession, years working at the hospital, years working in the department, hours worked per week, profession (physician, nurse, pharmacist, and others such as physiotherapist, nutritionist, and psychologist), and unit or department (medical, surgical, intensive care unit, pharmacy, and others).
Changes in PSC
The instrument used to assess PSC was the Hospital Survey on Patient Safety Culture (HSOPSC) questionnaire proposed by the Agency for Healthcare Research and Quality (AHRQ) 17, adapted to Brazil with the same dimensional structure as the original 18. The HSOPSC contains 42 questions that measure 12 PSC dimensions (D: see the first column of Table 1), one question about the overall rating of PS (0-100), another on the number of adverse events notified in the previous year, and socioprofessional data. The average completion time was 10-15 min.
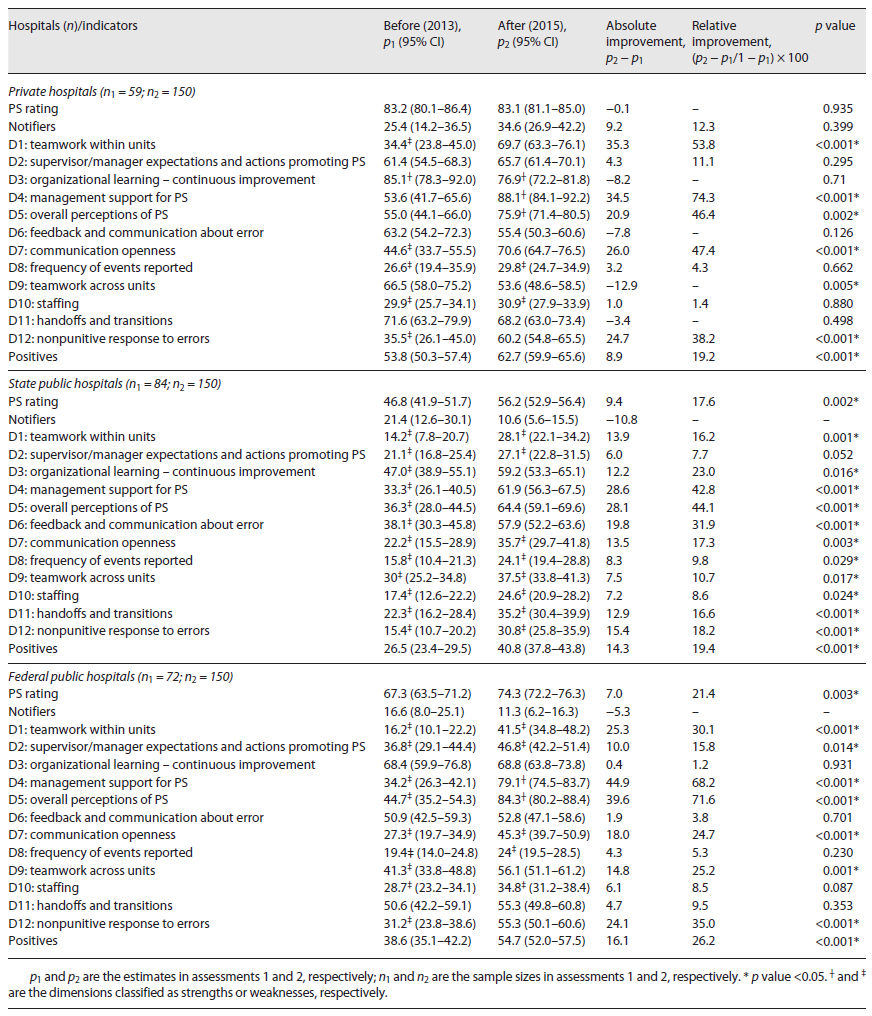
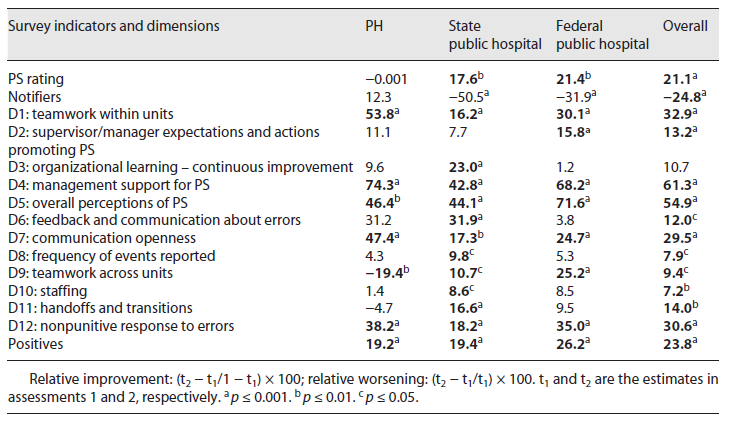
Table 1 Changes (relative improvement or worsening) in PSC after implementation of the NPSP, Brazil, 2012 and 2015
On both occasions, before and after the implementation of the NPSP, the questionnaire was emailed to the full- and part-time healthcare professionals of each hospital, including those involved in care and in management, excluding temporary professionals (the professional categories involved in the collection were all assisting with direct patient contact). It was mandatory for all responding professionals to have an email address as it was there that they received the invitation to the survey with the link to the questionnaire. To obtain the maximum number of responses, three emails were sent to each hospital at 7, 10, and 15 days. Data were personally collected by five evaluators (researchers involved in the translation and adaptation of the questionnaire) at each institution during the three shifts, to increase the sample size. Tablets and smartphones containing ad hoc software were used for data analysis 18. The software limited the response to only one attempt. Personal data, such as complete name, email, and profession, were registered in the application before the answers to the survey, and this information was used to control and avoid repeated responses. Before answering the questionnaire, all participants signed an informed consent form, and the collection software ensured the anonymity of the participants.
Data Analysis
For the progress in infrastructure for PS and implementation of the actions contemplated in the NPSP, we mapped a timeline of occurrence of events regulated by the NPSP, comparing the three hospitals and the dates of the main milestones related to the NPSP (approval, regulation, and enforcement). Concerning changes in PSC, we analyzed, in both measurements, the following indicators: % of positive responses by dimension, overall PSC rating (arithmetic mean of ratings on a 0-100 scale), % of professionals who notified adverse events in the previous year (“notifiers”), and a composite indicator (“positives”) calculated as the average of the percentage of positive responses in all 12 dimensions (agreeing or totally agreeing to questions worded positively or disagreeing or totally disagreeing to questions worded negatively). The 12 dimensions were additionally classified as strengths (≥75% positive responses) or weaknesses (<50% positive responses). This analytical approach followed the standard recommendations and indicators used by the AHRQ 17 and pilot tested in our adaptation of the HSOPSC survey 17. Each dimension was composed of several items/questions, and the response options varied on a Likert scale.
We calculated point and interval (95% confidence) estimates of all the indicators for the two assessments (before and after the NPSP implementation). The differences between the two assessments were calculated in terms of absolute (difference between the two assessments = p2 − p1) and relative improvements 19, the latter calculated as the percentage of the absolute improvement over the baseline room for improvement (1 − p1). In the case of negative differences, the % of relative worsening was calculated over p1. The significance of absolute improvements was assessed using Student’s t test for independent samples in the case of normally distributed variables and with the Mann-Whitney test for nonnormally distributed variables, after the application of the Kolmogorov-Smirnoff test of normality. For “notifiers,” the one-tailed z test was used to test the hypothesis of improvement. A 5% significance level was adopted for all tests, and the null hypotheses were rejected when the p value was less than 0.05.
Response rates in the two surveys were adjusted for nonresponse by profession and years working in the facility. We calculated indicators weighted by the actual proportion of the categories of these variables in the surveyed populations at the time of the surveys. Data were analyzed overall and stratified by the hospital, to better assess changes considering the different internal contexts.
Results
Changes in Structure and Activities to Improve PS
The timeline of events at the three participant hospitals from 2012 to 2015, as well as external events related to the NPSP and PSC measurements, are described in Table 2. Overall, it seems that the NPSP prompted the creation of infrastructure and the implementation of activities for PS improvement in all three hospitals, even though the pace of implementation was different in each one. At the outset of the study (November 2012), there was no specific infrastructure for PS in any of the three hospitals. The PH that had just been accredited had a unit for quality management that in theory included concerns and initiatives for PS. However, no specific activities for PS were identified.
Table 2 Timeline of events in the internal and external context of hospitals during the study period
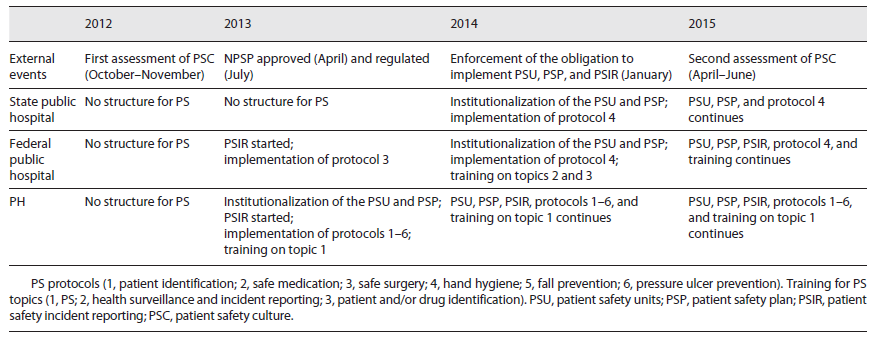
In 2013, the NPSP was approved (April) and regulated (July). During that year, the PH institutionalized a PSU, started a PSIR system, and devised a PSP, including the implementation of the six protocols proposed by the NPSP and the initiation of training in PS. The SH remained without either a PSU or any visible activities to improve PS. The FH however started its PSIR system and the implementation of the protocol for safe surgery, even though a PSU and PSP were not yet in place.
At the end of January 2014, the NPSP was made mandatory. Both public hospitals then institutionalized a PSU and devised a PSP. The range of activities to improve PS was different though. The FH initiated training on health surveillance and incident reporting, as well as on patient identification, whereas the SH did not include training for PS. Both implemented some protocols for improving PS. The PH completed the structure for PS (PSU, PSP, and PSIR) and continued with training on PS and the implementation of protocols to improve PS. In 2015, we conducted the second survey for measurement of the PSC in the three hospitals, as shown in Table 2.
Changes in PSC
Sample of Respondents and the Response Rate
A total of 665 questionnaires were answered. The response rate increased significantly in the second survey. The overall response rate was 26% (215 of 827 professionals) in the first evaluation (PH = 26.3%, SH = 22.6%, FH = 29.1%) and 70.9% (450 of 635 professionals) in the second evaluation (PH = 81%, SH = 32.6%, FH = 99%). Most of the respondents in the two assessments (n1 = 215; n2 = 450) were female (p1 = 72%; p2 = 79%), and the most represented professions were front line workers, such as nurses (p1 = 50.7%; p2 = 72.1%). Most respondents had 1-5 years of working experience at the hospital (p1 = 51.7%; p2 = 61.2%).
Changes in Safety Culture (Table 1)
The PSC increased over the first assessment in all dimensions in the two public hospitals and all but two dimensions in the PH. Relative improvements summarizing changes by dimension and hospital are described in Table 1, along with changes in overall PS ratings, % of “notifiers,” and the composite indicator “positives.” Some particular findings are worth underlining. First, even though changes were generally positive, there were differences between hospitals. The FH that started implementing PS activities 1 year before the SH improved most, while the PH that had the best PSC results in the first assessment was the only one with decreasing results in two dimensions and the overall PS rating but maintaining the best PSC results overall. Figure 1 depicts these differences and also shows that despite the significant improvements, there were still noticeable gaps requiring improvement in all hospitals, particularly in the SH.
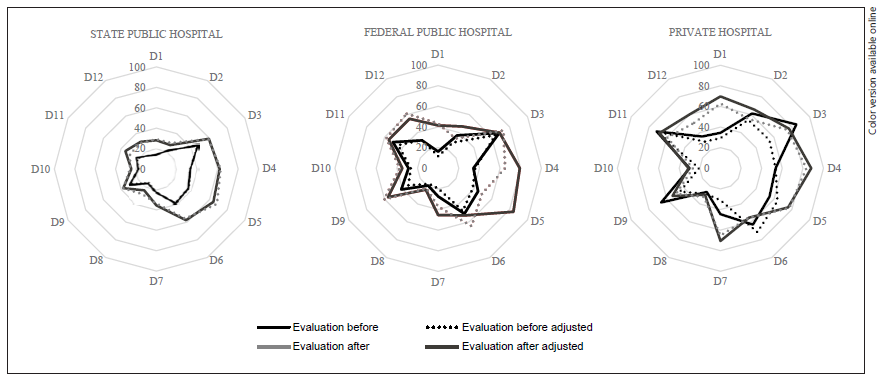
Fig. 1 Changes in the results of the PSC survey before (2012) and after (2015) the implementation of the NPSP in Brazil.
On the other hand, the two dimensions that improved most in public hospitals were the “overall perceptions of PS” and “management support for PS” (this also had the highest relative improvement in the PH), followed by “nonpunitive response to errors” and “teamwork within units” (that was also the second-highest relative improvement in the PH). Finally, the indicator “% of notifiers” was the only one with negative results in the public hospitals, particularly in the SH that had not implemented a PSIR by the time of the second survey. Overall (Table 1), in the PH, five dimensions (out of 12) improved significantly, and one decreased, while in the public hospitals, 11 dimensions improved significantly in the SH and seven in the FH. The indicator “positives” improved significantly in all hospitals, and the overall PS rating increased significantly only in PHs.
Table 3 describes the detail estimated by dimension and hospitals in the two assessments, as well as the absolute and relative improvements. The positive evolution of PSC was also evidenced by the variation in the number of strengths and weaknesses in the 12 PSC dimensions measured by the HSOPSC. The PH increased from one to three strengths and decreased from five to two weaknesses. The FH rose from zero to two strengths and declined from nine to three weaknesses. The state public hospital, which lagged behind the other two in the implementation of PS infrastructure and PS improvement activities, decreased from 12 to eight weaknesses but did not reach a level of strength (≥75% positive responses) in any of the dimensions. The dimensions that became strengths in the second assessment in the FH (and also in the PH) were “management support for PS” and “overall perceptions of PS” as shown in Table 3. The complete description of adjusted and unadjusted survey data, as well as the study database, can be accessed online (https://figshare.com/s/9361f1e664866a87bb93).
Discussion
This study contributes to the understanding of how external regulations may influence changes in PS that include but may go beyond mandating the existence of a visible structure for PS. The mandated structure probably should precede and condition other changes such as the one we measured in PSC. Because the original longitudinal and multicentric design was used, it brings some insights into the probable effects of the NPPS not yet studied in Brazil. It was possible to identify hospitals with different ownership, structure, and levels of PSC and then exposed to the same national health regulation for PS. The study design, without control hospitals not exposed to the external regulation, which was impossible given the nation- and system-wide nature of the NPSP, limits the strength of our conclusions. However, we believe that there are sufficient elements, which give consistency to the results, following change theory based on the literature 7. The increase in the response rate in the second collection may be related to the actions of sensitization of the PSU to completing the questionnaire, aiming to analyze the PSC in their institutions as well as greater dissemination of the instrument in the institutions.
According to the NQF recommendations to improve PSC 7, NPSP strategies can be classified as follows: (1) “leadership structures and systems for PSC,” including the creation of organizational structures (PSUs and committees) to promote safety at the health facility level; (2) “safety skills and teamwork training,” including the promotion of PS education in technical, undergraduate, and graduate courses; (3) “identify and reduce risks,” including mandatory PSPs at health facilities, risk management, protocols based on international safety objectives, and a national incident reporting system. Concerning the NQF recommendation “assessment, feedback, and intervention in a PSC,” there was no direct NPSP strategy.
Following this framework, the first reason for the improvement of PSC must have been the implementation of “leadership structures and systems for PS.” 7 The NPSP nationally instituted the PSU at municipal, state, and federal departments of public health, as well as at health facilities 14. These new organizational units seem to have been important in defining new values for participating hospitals, new behaviors, and causing changes in the PSC of institutions 20. Another reason for the positive changes was the institutionalization of risk management practices in hospitals 7. The PSPs that hospitals developed included promoting incident reporting and learning, investigating “never events,” and implementing at least six safety protocols based on the WHO’s global PS goals 21. The NPSP’s strategy to improve PS can be classified within the strategic domain of “regulation and standards,” according to the six domains framework for quality improvement proposed by the WHO 22.
However, not all the NPSP components were implemented in the three hospitals at the same pace or was the starting point before the NPSP similar concerning both the structure and activities for PS. One example was the PSU itself that was first instituted in the PH, then in the FH, and finally in the SH. The same occurred with the incident reporting system and the implementation of safety protocols. All this was reflected somehow in the results of the PSC surveys. The PH had the best results of the three hospitals at the outset but improved less (good results are more difficult to improve than low results) than the public hospitals, and among these, the SH improved the most (starting from the worst results) but still lagged behind the other two. It is noteworthy that the two dimensions with greater improvement were “management support for PS” and “overall perceptions of PS,” both dependent on the overall PS policy in the institution. On the other hand, the poor performance in notifying PS incidents 15 months after implementation of the NPSP also demonstrates the complexity of establishing these systems in any context, as reported in other studies 23.
The higher PSC level at the PH may be related to its autonomous administration, better infrastructure, and the level of human resources and because it faces greater demands from the regulatory agency. They adopted the NPSP recommendations faster than the other two hospitals. This hospital was also the only institution that participated in a nongovernmental accreditation program that evaluates the quality and PS standards 16. However, other factors may have influenced better positive responses, such as the instability of the contracts of professionals in this setting, who may be reluctant to criticize hospital safety. This kind of social desirability bias 24 may have influenced also, for other reasons, responses in the public hospitals, particularly after the NPSP was made mandatory. However, the consistency of results by dimension, improving more those related to overall policy and less those dependent on infrastructure (“notifiers” and “staffing”), suggests that this potential bias alone, if present, may not explain the PSC results.
Our data suggest that the effect was positive. It was objectively positive for creating a structure for PS, a necessary but not sufficient condition for quality 25 and also for creating awareness about PS and probably improving PSC. Some drawbacks were related to the little attention paid to other strategic domains like providing enough funding for the development of information systems for the national incident reporting system and training. Another missing component was the absence of a government strategy for periodically monitoring, providing feedback, and intervening in the PSC 7. Providing feedback to professionals is an important factor in improving quality, decreasing risks of adverse health events, and enhancing outcomes 26. The interventions considered in the NPSP may seem basic and incomplete, but they were innovative in the Brazilian context since the participating hospitals did not have a PSU, PSPs, PS protocols, incident reporting systems, or specific safety training for the health professions in PS 14. Although this may seem common in developed countries and Brazilian hospitals of excellence, it was an innovation for the country as a whole. The findings of this study confirm that the proposed national interventions make sense 7, but they also reinforce the need for a wider strategy and adequate funding to overcome the challenges of implementing the NPSP 27.
It should also be noted that for improvement in PSC, the objective should not be just to evaluate the culture but to evaluate and improve by making interventions in continuous improvement cycles, as recommended by the NQF (2010) 10. Most respondents had at least 1 year of work at the hospital, which gives greater validity to the assessment as people had some experience in their context and the systems that were implemented.
This study has some limitations. The first is that the study design, observational without control facilities, does not allow concluding that the changes in PSC are attributable to the NPSP 28. These changes however seem closely related to the NPSP milestones, which prompted, in turn, objective changes in the hospitals’ structure for PS. On the other hand, the response rate for the first PSC assessment was low. We dealt with a possible nonresponse bias, adjusting the survey results by the characteristics of the respondents, and found that the results were rather similar. Regarding the number of professionals per hospital typology, we dealt with a barrier that was the outdated hospital information system (CNES), which meant that we did not have the exact number. Finally, our results cannot be extrapolated to other Brazilian hospitals since other states may have different socioeconomic environments, and the facilities may have different internal contexts 16.
In conclusion, this study describes an improvement in the PSC in three Brazilian hospitals after the implementation of the NPSP. The improvements were apparently related to changes in structure and activities for improving PS in the three hospitals, induced by external regulatory pressures. Despite significant improvements, several weaknesses and a wide scope for improvement in PSC were also detected, confirming the need to strengthen the policy and initiatives for PS. The results showed the relevance that national initiatives such as the NPSP may have for PS.
Statement of Ethics
This study protocol was reviewed and approved by the committee of the Onofre Lopes University Hospital, approval number 54053616.0.0000.5292. Secondary data from hospital PS centers were used.