Introduction
Refractive error is the more frequent eye condition worldwide 1 and in Portugal 2. Despite the need for more robust epidemiological data on eye conditions in Portugal, the prevalence of refractive error in the country is estimated to be 43% 3. Considering the burden of refractive error within the population, and the ongoing need of these patients for services and devices 4, the necessity to frame refractive services within universal health coverage is demonstrated. Refractive error is the leading cause of vision impairment worldwide, and despite the lack of data on vision impairment due to refractive error or uncorrected refractive error in Portugal, for health planning, it is important to consider the global burden of this condition 1,4. The demographic trends of an ageing population, the worldwide increase in the refractive errors of myopia and high myopia, and other chronic eye diseases over the coming decades require urgent actions to develop innovative delivery of services that respond to the population’s needs 5.
The concept of services integration into the national health service (NHS) obeys to the principles of universal health coverage. It aims to ensure access and coverage to the promotive, preventive, treatment, rehabilitation, and palliative health services needed, when and where they are needed, and with financial protection. Access to health services can be divided into three dimensions 6‒8:
Physical accessibility: availability of quality and effective health services within reach of those who need them and with appointment/referral systems, waiting times, and other aspects of the service organization and delivery that allow people to obtain the services when they need them.
Financial affordability: the ability to pay for health services and medical devices without financial hardship. Indirect and opportunity costs, such as the costs of transportation or time away from work, are considered.
Acceptability: awareness and willingness to seek care. Acceptance and behavioural insights of the individual or community can have a determined action. A health condition, such as a refractive error, or the use of an optical device can be determined by a person or community’s specific health-related actions. Understanding how and why people and communities behave in their respective contexts allows to develop behavioural-informed strategies 9.
To ensure universal health coverage, health services must be physically accessible, financially affordable, and acceptable to users. Other countries, such as the UK, recognized a long time ago the need to develop primary eye care to manage chronic eye conditions with relatively simple interventions, such as refractive error, and prevent people from resourcing to the hospitals for that. Primary eye care in the UK’s NHS, where refractive services are based, is currently provided by optometrists, general practitioners, and ophthalmic medical practitioners. Over recent years, there was a demand to increase the skills and competencies of optometrists for them to take on more advanced roles and responsibilities 1,10-15. First, it is important to emphasize that in the Portuguese NHS, there are no specific services to address refractive errors 15. The management and treatment of refractive error occur at the level of eye care general services, without specific assessment or referral. In this way, on the same waiting list and in the same order of priorities, there are people with ongoing refractive error needs and people with pathologies that can cause irreversible blindness in a short time, like glaucoma. Most of the refractive care delivered in Portugal occurs in the private sector, divided between the private medical sector and the optical sector, without any referral system, integration within the NHS, or the national health plan 16. Additionally, eye care services available within the Portuguese NHS are almost entirely secondary care level and fully hospital-centred, providing refraction services without differentiation of care 15. There are two formal initiatives currently taking place at the primary care level: screening interventions for infants/children and the systematic screening of diabetic retinopathy for people with diabetes. There is an evident absence of eye care at primary care, limited to the recent screening initiatives. For that reason, there is an openness and the realization of the need to implement a methodology capable of proposing new measures and improving the system as a whole, based on strong primary eye care 2. To the best knowledge of the authors, this is the first approach to the analysis of refractive services in Portugal, and the integration of those services into the NHS, available in the literature. It aims to start a research line and to contribute to monitoring the commitment of Portugal with the global target for 2030 of increasing by 40% 1 the effective coverage of refractive error 17.
Materials and Methods
A situation analysis of the Portuguese NHS capacity to address refractive error was conducted. The World Health Organization (WHO) Eye Care Situation Analysis Tool (ECSAT), which supports countries in the planning and evaluation of eye care services, served as a basis for that analysis. The information for the situation analysis was proactively collected from accessible and official sources from the Ministry of Health, such as national reports, national strategies and planning documents, and workforce inventory frameworks, among others. Official organization databases were systematically searched to retrieve all potentially relevant reports/documents about refractive error services in Portugal. The information was divided according to ECSAT components. ECSAT components are informed by, and categorized under, the six WHO health system-building blocks. Three of those building blocks were used to conduct this situation analysis:
Service delivery access: number of NHS centres providing refractive services and waiting times for an eye care/refractive care assessment
Service coverage: distribution of the available services by geography and population density
Workforce: number of eye care personnel in the NHS centres providing refractive services
These three building blocks were selected based on the nature of the services to be assessed. The objective of this situation analysis is to give a comprehensive overview of the availability of refractive services in the country’s NHS 18.
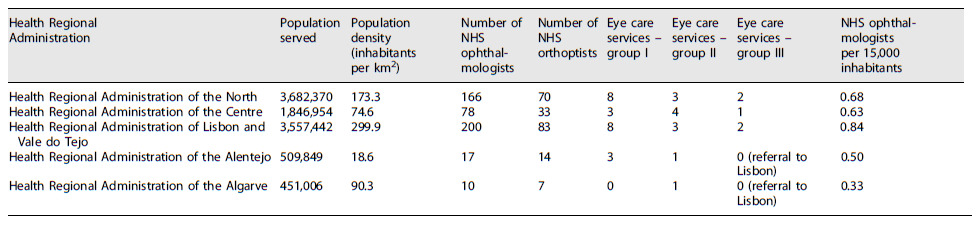
A strengths, weaknesses, opportunities, and threats (SWOT) analysis was performed based on the existent evidence to identify the internal and external factors that can potentially facilitate or hinder the possible integration of refractive error within the NHS. A systematic search was conducted in multiple national and international electronic scientific databases, such as MEDLINE/PubMed, Web of Science, Scopus, and Google Scholar, among others, to retrieve all potentially relevant publications about refractive error services. A comprehensive search strategy was conducted combining terms related to the eye condition (refractive error, myopia, hyperopia, presbyopia) and terms related to the outcome of interest (refractive error services, primary eye care, eye care services) combined by Boolean operators (OR, AND) or not. No time interval for the study’s conduction has been defined. For every publication or paper found, the reference list was reviewed searching for additional studies or data in an attempt to retrieve all the relevant information. Information was extracted and categorized according to the SWOT domains:
Strengths: positive impacts and effects in the health system and population health status
Weaknesses: disadvantages and negative effects in the health system and population health status
Opportunities: elements that can be used in advantage to improve the health system and population health status
Threats: elements that can cause disadvantages and compromise the health system and population health status
Priority areas to be addressed were defined based on the situation analysis, including workforce. For workforce planning, the number of eye care personnel to integrate was calculated considering the minimum ratio recommended per population:
Results
Current Capacity of the Portuguese NHS to Address Refractive Error
NHS eye care services in Portugal are hospital-centred and divided into three large groups, according to technical differentiation, the technology required, and workforce capacity. Group I ophthalmology services cover an area of minimum 75,000 inhabitants with daily service of basic eye care interventions, such as refraction or general assessments, and according to a referral protocol centralized by a group III service has fewer resources, both technological and workforce. Group II ophthalmology services are medical-surgical daily services that cover all eye care interventions except for oncology, transplantation, paediatric glaucoma and cataract, retinopathy of prematurity, and rare diseases; they have more resources than group I. Group III ophthalmology services are responsible for all eye care interventions and have more resources, both technological and workforce, than the previous groups 15. According to the last National Strategy for Eye Care, from 2018, Portugal had 22 group I ophthalmology services, 12 group II, and 5 group III 2. It is also important to emphasize that at the NHS level, the integrated workforce is composed of ophthalmologists and orthoptists, together with nurses and other general paramedical assistants 2.
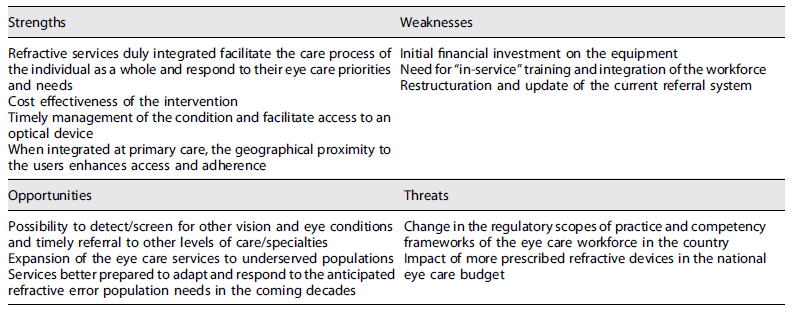
Purely analysing the geographical distribution of NHS eye care services in Portugal, fundamental limitations of coverage and centralization of services, mainly in urban areas, were identified (Fig. 1). Data from 2021 show that only 3 Portuguese municipalities have more than 1 NHS eye care service and 35 have 1 NHS eye care service, which leaves 240 municipalities (in the mainland), especially those in the most rural and remote areas, underserved 2,15.
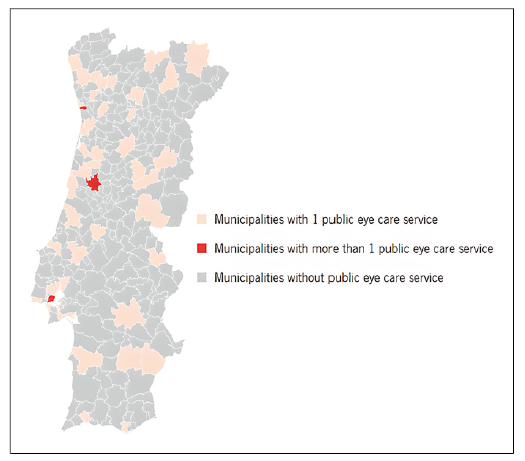
Fig. 1 Total number and distribution of NHS eye care services in the country (elaborated based on official data on waiting times from the Ministry of Health) 21.
When analysed the geographical areas, the total population served by the direct influence of the NHS eye care services, and the available workforce within the NHS eye care services (Table 1), a shortage in the workforce per inhabitant was observed. According to the 2016 National Network of Hospital Specialty and Referral - Ophthalmology, the minimum ratio recommended is 1 ophthalmologist per 15,000 population 15,16. Additionally, WHO recommends a ratio of 1 optometrist per 50,000 population in 2020 19,20. There are no recommended ratios for allied ophthalmic personnel (where orthoptists are included). It is important to emphasize that these recommendations for the workforce are always assessed considering the coexistence of the professional groups: ophthalmologists, optometrists, and other allied ophthalmic personnel. However, although in the absence of one, other(s) could address the condition and that do not represent an emerging problem, the lack or inexistence of all of them translates into important barriers to accessing services.
Table 1 Distribution of NHS eye care services and NHS ophthalmologists (elaborated by the authors based on official data from the Ministry of Health, the 2016 National Network of Hospital Specialty and Referral - Ophthalmology, and the 2018 National Strategy for Eye Care) 2,16,21
In every NHS Regional Administration of the country, it is observed a shortage of eye care workforce, for ophthalmologists (ratio per 15,000 inhabitants <1) and optometrists (inexistent). The ratio of orthoptists per 15,000 inhabitants is 0.3.
One of the consequences of not providing refractive services as differentiated care, with a proper and functional referral system, is the extensive waiting lists for a general eye care assessment that compromises timely delivery of care, not only for refractive error but for other conditions that are placed at the same list of priority. Between the years 2016 and 2017, referrals from primary care to ophthalmology increased from 313,941 to 327,431, showing a demand for eye care. Of those, 181,824-223,228 were left unattended, respectively, and the median waiting time has increased from 171 days to 180 days, with a maximum of 783 waiting days for an eye care assessment 16. More recent data from 2021 show that 52% of the hospitals providing eye care services do not meet the recommended response times 21.
Centring the NHS eye care at the secondary care level is known to be an ineffective and expensive use of eye care resources. A simple comparison with the UK model clearly evidences the Portuguese NHS shortcomings 22. Evidence shows that the delay in the use of primary eye care provided by optometrists is associated with a greater probability of resorting to general practitioners, as an indicator of missed opportunities to detect potentially serious eye conditions 23.
Current Refractive Error Services Available in Portugal
Furthermore, access to the prescribed optical devices is often compromised once their acquisition is fully made through out-of-pocket payments for the majority of the population. The NHS limitations force patients to turn to the private medical sector and optical shops, with the increase in the costs and financial risks associated. In addition to the exposure to financial risk, the inexistence of a specific regulation that defines the prescriber, training requirements, guidelines, and medical devices dispensing regulation that includes optical devices exposes patients to considerable risks to public health 16.
Formal, government-approved training in public universities, that train professionals with knowledge and competencies to provide refractive services in autonomy, are available in Portugal since 1988 24. However, the lack of concertation between the Ministries of Science, Technology and Higher Education and Health does not consider these professionals as a regulated health workforce.
Despite the formal academic training, optometry remains the only eye care discipline unregulated in Portugal and with no legislative framework that ensures guidelines for practice 25. Recognizing that the majority of refractive devices prescriptions in Portugal occur in the private sector and optical shops, the inexistence of specific policies and regulations exposes the population to considerable risks of inadequate health services provision and unnecessary financial burden.
Problem Analysis and Setting Priorities (SWOT Analysis)
Due to the impossibility of maintaining the current practices regarding refractive care, and eye care, the provision in the NHS imposes a paradigmatic shift that breaks with previous overcome practices and with the permanent insufficiency in the provision of these services. It is consensually assumed that better cost-benefit practices must be implemented but more important than that is the requirement of changes that protects public health, patients, and professionals, that provides care where is needed, when is needed, not exposing the user to financial risks.
Scientific evidence, technical recommendations, and standards for good practices 4,26, (27, as well as socio-economic impact analysis 16, show the same actions: a solid primary care-based eye care, that covers differentiated and multidisciplinary care, duly integrated not only within the NHS but within other sectors, such as education or labour 28. The reform of health systems and health policies has been proven to be challenging 29. Regarding eye care, and refractive services specifically, the solution that is immediately reachable for Portugal is to take advantage of the workforce already trained and existing infrastructures in the country and implement policy and regulatory changes to address this condition.
Refractive error services are becoming a worldwide priority, due to the prevalence of this condition, and once it is a simple, easy, and cost-effective intervention, with substantial and measurable impact on the quality of life 4,17,30. In addition to that, it is also an intervention that makes possible the periodic screening of vision and eye conditions that can be duly addressed if timely detected and referred, representing health gains for the patient and efficiency gains for the health service 23. Given the predicted increase in the need for refractive services, considering the anticipated increase in the prevalence and population demographic variations, it is also fundamental to prepare eye care services to rapidly adapt and respond to the expected demand 1.
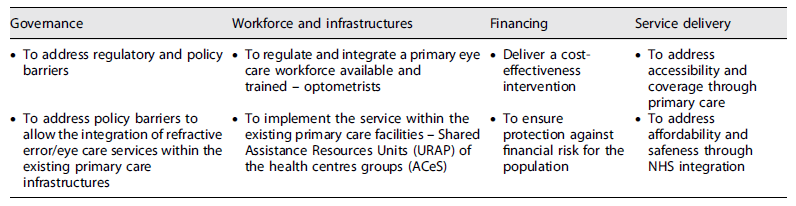
An analysis of the strengths, weaknesses, opportunities, and threats - SWOT analysis (Table 2) - based on the existent evidence 28,30-34 was made to identify the internal and external factors that can potentially facilitate or hinder the possible integration of refractive error within the NHS. Table 3 summarizes the actions to be made to implement refractive services within NHS according to relevant WHO health systems building blocks 35.
Discussion
Resources and Action Plan for Refractive Services
The problems and barriers identified in the access to refractive error services within the NHS were as follows:
Inexistence of primary eye care that can address refractive error at a primary care level, in a context of proximity to the population.
Physical barriers to accessing the services with centralization of eye care services in urban hospitals and an undifferentiated referral system with no priorities defined by conditions or severity.
Workforce shortage that limits the coverage of eye care services and contributes to the extensive waiting times for services to respond.
Refractive services need to be properly integrated across relevant health programmes, such as child health or healthy ageing and non-health programmes such as social services, education, or labour. The refractive error should be addressed from a public health perspective, enhancing equity in the access, quality of the services, and effective coverage. Interventions to address refractive error are considered essential and should be included within NHSs as they are frequently and periodically required by the population and can benefit a large number of individuals 28,30,41. Evidence emerges of the need to reorient refractive services towards primary health care, where they can be more accessible to the community 28,30. In order to provide a proposal that ensures universal access to refractive error care, with health and financial protection, this work presents a concrete recommendation, based on scientific evidence, technical recommendations, and experiences from other countries. The recommendation is the integration of refractive services within the NHS primary care network.
Refractive Error Service Delivery: Access and Quality
Previous experiences show that addressing refractive services in short-term programmes or in settings without regulation compromises sustainability and service delivery 28,30. Addressing a refractive error is not only essential due to the high prevalence among the population but also because it represents an ongoing need that requires more than an isolated intervention. Refractive error patients need periodic assessments and updating of devices, demanding sustainable services that are easy to access and of effective coverage, both in capacity and quality.
The declaration of Alma-Ata 42, adopted by the WHO, defines primary health care as “the first level of contact of individuals, the family and community with the national health system bringing health care as close as possible to where people live and work, and constitutes the first element of a continuing health care process.” The promotion, prevention, and treatment of refractive error fall within this level of care and the integration into the NHS grants the sustainability and service delivery needed to ensure long-term provision.
Sustainable service delivery in refractive error is a critical element to improve population health status, along with other factors, including social determinants of health. To ensure well functioning, the country’s network of refractive services duly integrated into primary care centres should have the following characteristics 36,37:
Comprehensiveness: provides not only refractive services but also detection and screening of other vision and eye conditions and timely referral to other levels of care/specialities, through a functional referral system. Eye care promotion and prevention activities, appropriate to the needs of the target population, are also essential to raise awareness and acceptance.
Accessibility: refractive services must be permanently and directly accessible to the population, delivered at a primary level, with no physical barriers of geography or exposure to financial or health risks.
Coverage: refractive services must be designed to cover the entire population, with or without the condition, since this is a condition with a high prevalence, will most probably affect every person during their life cycle, and represents an ongoing need for care.
Continuity: refractive services must provide continuity of care not only over the lifecycle and the ongoing need but also across the different services and conditions experimented by the individual. This highlights the need for integration within a vast system of health.
Quality: refractive services must be effective, safe, timely delivered, and people centred. Effectiveness and safety are intimately linked with the regulation and policies that normalize the provision of care.
People-centredness: refractive services must be centred on the individual and not the condition or financing. Adopting a user perspective allows services to be responsive and acceptable.
Coordination: usually the primary care provider is the entry point into the health system and facilitates the route through the needed services. Coordination with the different levels of care and a totally functional referral system is essential for a well-functioning refractive service.
Accountability and efficiency: refractive services must be managed to achieve core elements and address population needs with minimum wastage of resources.
Refractive Services Workforce and Operational Implementation
To address the Portuguese population’s refractive needs and respond to the eye care shortage within the NHS, a new professional eye care category must be integrated within NHS to work alongside medical-surgical professionals - ophthalmologists - and the other allied ophthalmic personnel. Worldwide, optometry has been the major provider of refractive services, Portugal included even though from a private sector setting 38. The population of trained optometry professionals in Portugal was estimated at 1,690 individuals in 2018, according to data from the International Agency for the Prevention of Blindness, with minimum academic qualifications of a Bachelor in Sciences 39.
The use of the optometry workforce by the NHS is justified by the population’s refractive needs but has to be driven by a regulatory and policy framework that allows integration, protecting the professional, the user, and the services themselves. Placing the optometrist at primary care not only enhances the management of refractive error immediately without clogging the system but also allows the possibility to detect/screen for other eye conditions and timely referral to other levels of care or medical specialities 28. Integration of optometrists also represents budget savings for the government and use of the resources invested, since this is a qualified workforce trained in governmental academic institutions, without the latter taking advantage of its competencies 16. The UK, for instance, has generated evidence over the past years that confirms the effectiveness of optometrists providing primary eye care. With fewer ophthalmologists in the UK, optometrists with suitable training and accreditation demonstrate to be as safe and effective in the management of chronic eye conditions, not only refractive error but also glaucoma or diabetic retinopathy 10,43-45.
The implementation of refractive services in the NHS should occur within the already existing organizational framework, to facilitate the path of the user within the system. Since 2008, primary health centres are organized into groups, health centres groups (ACeS) with the main objective of improving their performance. The ACeS is constituted by a set of functional units with administrative and technical autonomy. One of these units, and the more complex and distinct from the others since it outlines a wide range of specialized skills, is the Shared Assistance Resources Units (URAP). URAP articulates directly with all the other functional units and contributes to a timely and full response, to the ongoing need for care and proximity, which results in a reduction of costs, number of hospital referrals, and number of complementary means of diagnosis and therapeutics, contributing to the NHS sustainability, better quality services, and better health outcomes for the population. URAP is formed by different professions to address the population’s ongoing needs of care, such as psychologists, physiotherapists, oral health technicians, nutritionists, and social workers, among others 40. The wide range of specialized skills reflected in the URAP, and its goals, place these units as the ideal setting to integrate refractive services.
ACeS geographically covers the entire country (Fig. 2), in a logic of proximity, both in urban and rural areas, duly integrated into the community and represents the first level of care for NHS users. Data from 2012 show 357 health centres and more than 1,000 extensions, duly aggregated into ACeS. Every municipality in the country has at least 1 health centre 46. Its distribution within the entire country allows for delivering care in a more efficient way, reducing transportation expenses and work absence losses for the user, which results in more adherence, acceptance, and compliance with the intervention or care.
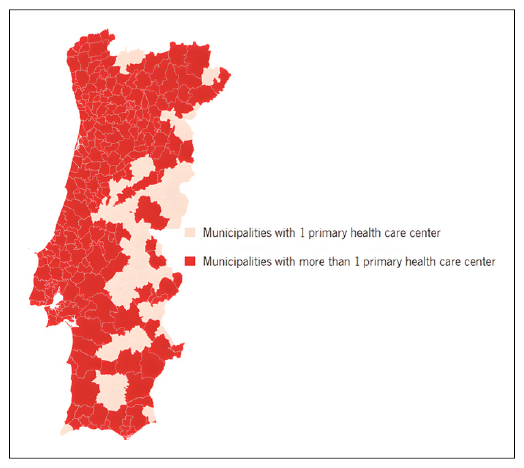
Fig. 2 Total number and distribution of NHS primary health care centre in the country (elaborated based on official data from the Ministry of Health) 40.
Integrating refractive services within the URAP units of the ACeS will allow taking advantage of the specific health policies of these units to cover another area of care and take advantage of the existing infrastructure and referral and access systems. Additionally, it will allow a total geographical coverage within the country, offering refractive care in the community and in a logic of proximity to the population and their ongoing needs for this type of care.
Following the minimum ratio recommended for eye care workforce per population previously approached in this work, safeguarding the population density, the integration of 200 optometrists within the NHS, at URAP level, would allow addressing the minimum needs of refractive error at primary care (Table 4), complying with the minimum recommendation of 1 optometrist per 50,000 inhabitants according to the refractive error needs to be estimated for 2020 19,20. It should be noted that the number of ophthalmologists is maintained at the current one, but an increase in the number of professionals is needed to meet the recommended minimum ratio of ophthalmologists per population.
Table 4 Proposal for distribution of NHS eye care services, hospitals, and primary care centres and recommended NHS eye care workforce for primary eye care (elaborated by the authors based on official data from the Ministry of Health, the 2016 National Network of Hospital Specialty and Referral - Ophthalmology, the 2018 National Strategy for Eye Care, and the Primary Health Care Identity Card (Bilhete de Identidade dos Cuidados de Saúde Primários) from the Shared Services of the Ministry of Health) 2,16,21
From a health-economics point of view, refractive error intervention represents one of the most highly cost-effective vision-restoring interventions and, along with cataract surgery, would solve more than 90% of unmet eye care needs 5. Integration of refractive error services within the NHS will also remove one important barrier to accessing those services, the financial barrier 5. Globally, uncorrected refractive error poses an enormous economic burden on society with annual global productivity losses from uncorrected myopia in adults and presbyopia alone estimated to be USD 244 billion and USD 25.4 billion, respectively 12,13. This provides a strong health economic rationale for increasing coverage of these eye care interventions 32,33,47,48. In addition, the compensation of refractive error, vision improvement, and optimization of vision functional ability leads to improvement in employment prospects, enhanced work productivity, increased household income, and enhanced economic productivity of both individuals and nation. That happens not only for people able to meet their full visual potential but also for those with vision impairment 49.
Considering the country’s economic and financial situation in the past years and the sustainability of the NHS, it is imperative to guide the health systems towards strong primary care. Evidence indicates that primary-centred health systems are more cost effective, more responsive to health care needs, and ensure more equity in access 26.
A factor that could facilitate the implementation of refractive services in the Portuguese NHS is recent Portugal's favourable position, in the WHO 74th World Health Assembly, to the endorsement of the new global eye care targets, one of them being the effective refractive error coverage 17,35,50. In summary, the Portuguese NHS has all the requirements to reorientate refractive care from the current hospital-based model to primary care. The country also has a trained and qualified workforce to address this condition. Evidence demonstrates that the provision of refractive services at primary care is efficient and effective and translates into an opportunity to identify other visual conditions.
Statement of Ethics
This research did not involve human participants, not requiring ethical approval or consent from participants.