A 78-year-old Portuguese woman, phototype II Fitzpatrick, presented to our Dermatology Department with an asymptomatic reddish depression on her right thumb, which had persisted for more than thirty years. The patient denied previous chemical or physical trauma. Her medical history was unremarkable. Physical examination revealed a 14 × 10 mm, nummular, well-circumscribed erythematous patch with a slightly depressed surface on the volar aspect of her right thumb (Fig. 1-A). Under polarized light, dermoscopy showed homogeneous, structureless erythema with linearly distributed whitish spots and sparse dotted vessels (Fig. 1-B). In addition, a stepped desquamation at the edge of the lesion was seen. On histopathological examination, the periphery of the lesion revealed an abrupt stair-like thinning of the stratum corneum, forming an area of hypokeratosis in the center (Fig. 1-C). Dilated capillaries were present in the upper dermis. There was no parakeratosis or keratinocyte atypia.
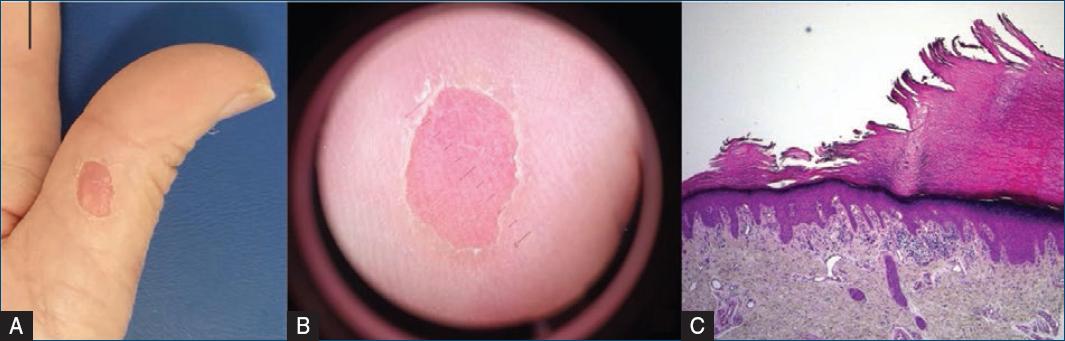
Figure 1 A: clinical findings: A nummular, well-circumscribed erythematous depression is observed on the volar aspect of right thumb. B: dermoscopy findings: a homogeneous, structureless erythema with linearly distributed whitish spots and sparse dotted vessels surrounded by a rim of stair-like desquamation. C: histopathologic findings: The periphery of the lesion revealed an abrupt stair-like thinning of the stratum corneum forming an area of hypokeratosis in the center. Dilated capillaries were present in the upper dermis. (haematoxylin and eosin (H&E), original magnification ×40).
Topical treatment with 5-fluorouracil 5% in combination with salicylic acid 10% was started; however, no significant improvement was noted after 12 weeks.
This is a typical case of circumscribed palmoplantar hypokeratosis (CPH), a rare skin condition, first described in 2002 by Perez et al.1. The etiopathogenesis of CPH remains unknown but has been proposed to be a localized disorder of a clone of keratinocytes1. It predominantly affects middle-aged women and is characterized by a well-demarcated, depressed, erythematous lesion, rimmed by a hyperkeratotic border localized on the palms or, less commonly, on the soles2.Clique ou toque aqui para introduzir texto. The main clinical differential diagnosis includes Bowen disease and porokeratosis of Mibelli1,2.
Dermoscopy is a non-invasive technique that may increase accuracy in the differential diagnosis. It reveals whitish streaks and white dots with regular distribution over a light erythematous background surrounded by a rim of stair-like desquamation1.Histopathologic examination is distinctive and essential for the diagnosis. It is characterized by a marked decrease of the horny layer thickness, forming a sharp step with the adjacent normal horny layer, which closely correlates with the dermoscopic findings2.
Treatment of CPH is challenging, and many modalities have been recommended, including local steroids, retinoids, keratolytics, emollients, cryotherapy, and surgery1,2. However, these treatments have shown variable efficacy, and lesions usually last for years1,2.














