Introduction
Acne vulgaris is a chronic inflammatory skin disease that often affects adolescents and young adults1. It originates in the pilosebaceous follicle and is characterized by increased sebum production, follicular hyperkeratinization, inflammation, and bacterial proliferation of propionibacterium (P. acnes)2. There are several predisposing factors that have been considered, from environmental to hormonal, dietary, and genetic factors1. Clinically it is manifested by noninflammatory (open and closed comedones), inflammatory (papules, pustules, nodules, and cysts) and residual lesions (scars, hyperpigmented macules), which appear on the face, chest, and upper part of the trunk2,3. Scars and keloids can affect the quality of life and be associated with depression, anxiety, and suicidal ideation1,3.
The approach and treatment depend on the location, morphology, and severity of acne2. Isotretinoin is a first-generation retinoid (vitamin A derivative) that acts directly on the pilosebaceous follicle, with decreased sebum production and a comedolytic effect.2 Oral isotretinoin is used in the treatment of severe or refractory nodular acne2,4. The most frequent side effects are xerosis, xerophthalmia, cheilitis, headache, dyslipidemia, and increased hepatic transaminases2,4. Psychiatric pathology, such as depression and suicidal ideation, may be related to the use of isotretinoin, however, this association is not yet clarified2,4.
In this sense, it was considered relevant to review the existing scientific evidence on the association between isotretinoin and the risk of depression in patients with acne.
Methods
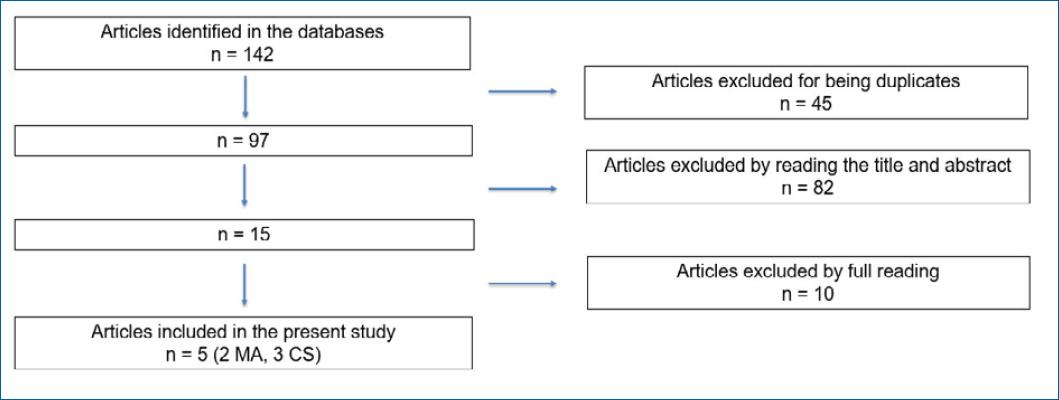
A nonquantitative systematic search was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations5. Clinical guidelines, systematic reviews, and original studies were searched in Pubmed, Cochrane Library, Embase, Scopus, National Institute for Health and Care Excellence Guidelines Finder, National Guideline Clearinghouse, Canadian Medical Association Practice Guidelines InfoBase, Database of Abstracts of Reviews of Effectiveness (DARE), Bandolier, British Medical Journal Clinical Evidence, Evidence-Based Medicine Online, published between January 2017 and January 2022. The MeSH terms isotretinoin, acne, and depression were used. The PICO model was used to formulate the research question: (i) Population: patients with acne vulgaris; (ii) Intervention: treatment of acne with isotretinoin; (iii) Comparison: other acne treatments; (iv) Outcome: risk of depression in acne patients under treatment with isotretinoin. Studies in Portuguese, English, or Spanish, with full text and carried out in humans, were included. The following exclusion criteria were considered: duplicate articles, opinion articles, classic review articles, clinical cases, and articles in disagreement with the objective of the review.
The selection of articles was made in duplicate by the first and third authors who, in case of doubt, would discuss the inclusion/exclusion of the article with the second author. The agreement rate between authors in the selection of articles was 100%. All authors performed the full reading and assessed the quality and level of evidence (EL) of the selected articles and the strength of recommendation according to the American Family Physician’s Strength of Recommendation Taxonomy (SORT) scale9.
Results
A total of 142 articles were obtained, of which only five met the inclusion criteria and did not present exclusion criteria: two meta-analyses and three cohort studies, two prospective and one retrospective. The article selection phases are demonstrated in Figure 1.
The systematic review and meta-analysis by Li et al.3, carried out in China, investigated the association between the use of isotretinoin and the risk of depression in patients with acne. A search was carried out in PubMed, Cochrane Library, and Embase databases, and 20 studies were selected. The study suggested that while isotretinoin could theoretically cause depressive disorders, the risk of depression could be outweighed by its favorable outcome in acne patients. Acne negatively affects the quality of life and self-esteem and can have a significant psychological impact and lead to psychiatric illnesses such as depression. In such matters, isotretinoin can improve the depressive symptoms caused by acne through the improvement or resolution of the associated lesions. The lack of randomized clinical trials, the heterogeneity of the studies (namely in dose and duration of treatment and depression scores), and some of the studies with a small sample size are important limitations of this study.
The most recent study included in this review was carried out in Taiwan by Che et al.4. This is a retrospective cohort study following for 16 years 29943 patients with acne, of which 9981 received treatment with isotretinoin and 19962 constituted the control group. Patients with a history of psychiatric illness, aged less than 20 years, and treated with isotretinoin for less than 1 month were excluded. There was no increased risk of psychiatric illness in patients treated with isotretinoin, even with higher dosages or longer duration of treatment. The retrospective character is a limitation of this study.
The systematic review and meta-analysis by Huang et al.6, carried out in Thailand, evaluated the relationship between the treatment of acne with isotretinoin and the risk of depression. A bibliographic search was carried out in the Pubmed and Cochrane Library databases, and 31 studies were selected that indicated the prevalence of depression or that used depression scales. They concluded that acne treatment with isotretinoin is not associated with an increased risk of depression and that acne treatment appears to improve depressive symptoms. This review’s limitations were the great variability of the included studies (for example, regarding the assessment instruments used) and the fact that there was no randomized clinical trial.
Alghofaili et al.7 performed a prospective cohort study in Saudi Arabia, which included 179 patients of whom 119 were treated with oral isotretinoin, at a daily dose of 0.5 mg/kg, and 60 with different topical treatments (tretinoin or tazarotene). The Beck depression inventory scale was applied before 3 and 6 months after the start of treatment. It was concluded that there is no correlation between isotretinoin treatment and the development of depression and that acne treatment (regardless of drug) is associated with improvement in depressive symptoms. Nonetheless, the small sample size and study design are limiting factors (non-randomized, non-blinded).
In Saudi Arabia, Algandi et al.8 performed a prospective questionnaire-based cohort study from November 2019 to March 2020 to assess the risk of depression in acne patients treated with isotretinoin, at a daily dose of 0.5 mg/kg, versus doxycycline in a daily dose of 100 mg (control group). The study included 29 patients with moderate to severe acne aged between 18 and 30. Patients with a personal or family history of psychiatric illness, regular use of antipsychotics or antidepressants, or previous treatment with isotretinoin were excluded. Patient Health Questionnaire 9 (PHQ-9) was administered before and 8 weeks after the start of treatment. Eighteen patients (nine men and nine women) completed the study, of whom 12 received treatment with isotretinoin and six received doxycycline. There was no statistically significant difference between the PHQ-9 scores of the two groups concluding that there is no direct relationship between isotretinoin and the development of depression. The small sample size is one of the limitations of this study.
Table 1 summarizes the characteristics and results of the selected studies.
Table 1 Summarized description of selected articles
| Authors, year | S | Target population and study design | Results/conclusions | Limitations | EL |
|---|---|---|---|---|---|
| Li et al., 20193 | MA | 20 studies | Isotretinoin improves symptoms of depression in acne patients. | RCT not included; some studies with small samples; heterogeneity of studies. | 1 |
| Huang et al., 20176 | MA | 31 studies | No association between Isotretinoin and depression. | RCT not included; great heterogeneity of studies. | 1 |
| Chen et al., 20224 | CT | (n = 29943) Retrospective study | No association between Isotretinoin and an increased risk of psychiatric illness, including high doses or prolonged duration. | Study in a specific population (Taiwan); risk of suicidal ideation not assessed. | 2 |
| Alghofaili et al., 20217 | CT | (n = 179) Retrospective study BDI Scale | Isotretinoin for acne does not appear to be associated with a statistically significant risk of depression. Acne treatment improves depressive symptoms. | Small sample size; non-randomized, open-label study. | 2 |
| Algamdi et al., 20208 | CT | (n = 29) Prospective study, questionnaire PHQ-9 | No direct relationship between isotretinoin and the development of depression. | Small sample size. | 2 |
S: study type; EL: level of evidence; SR: systematic review; MA: meta analysis; CS: cohort study; RCT: randomized clinical trial; PHQ-9:- patient health questionnaire 9; BDI: Beck depression inventory.
Discussion
The risk of depression associated with isotretinoin treatment in patients with acne has been a concern and a controversial topic3,6 which motivated this systematic review.
After a detailed analysis of the included studies, we found that there is no evidence that isotretinoin is associated with depression3,4,6-8.
Chen et al.4 carried out a cohort study with a larger sample size and, in addition to depression, studied the risk of other psychiatric illnesses (anxiety, bipolar disorder, mania, personality disorder, schizophrenia, and suicide). They concluded that there is no evidence of an increased risk of depression or other psychiatric illnesses linked to isotretinoin.
Li et al.3 reported heterogeneity of studies in terms of dosage and duration of isotretinoin treatment and were unable to draw conclusions regarding these variables. On the other hand, Che et al.4 studied the influence of the dosage and treatment duration and showed that there was no increased risk of depression and other psychiatric diseases regardless of the dosage and duration of isotretinoin treatment. In the remaining studies, these variables were not evaluated.
Although the individual susceptibility to depression during treatment with isotretinoin cannot be ruled out, current evidence suggests that treatment of nodulocystic acne with isotretinoin is safe and does not increase the risk of depression6. Nevertheless, Che et al. recommend close surveillance of patients with greater susceptibility4,6.
The strengths of our review are the comprehensive research in several databases, recent studies (published in the last 5 years), and moderate to high quality (with evidence levels 1 and 2).
On the other hand, there are some limitations: no randomized clinical trials were included; some of the studies have a small sample size and present methodological heterogeneity, namely, depression assessment scales, dosage, duration of treatment with isotretinoin, and history of psychiatric illness. Randomized clinical trials would allow for a stronger EL however not treating patients with severe acne with isotretinoin would raise ethical questions. Prospective studies aimed at patients with a psychiatric history may also be of interest.
This evidence-based review demonstrated that treatment of acne patients with isotretinoin does not appear to be related to the development of depression, with a strength of recommendation of A3,4,6-8. We further conclude that treatment of acne, regardless of chosen drug, seems to improve depressive symptoms3,6,7. More studies, such as randomized clinical trials or other prospective studies with larger sample sizes, are needed to confirm these findings.
What does the study add?
Depression may be related to the use of isotretinoin, however, this association is not yet clarified. In this sense, reviewing the existing scientific evidence on the association between isotretinoin and the risk of depression in patients with acne was relevant. This systematic review demonstrated that treatment of acne patients with isotretinoin does not appear to be related to the development of depression. We further conclude that treatment of acne, regardless of chosen drug, seems to improve depressive symptoms. More studies, such as randomized clinical trials or other prospective studies with larger sample sizes, are needed to confirm these findings.