Introduction
Alopecia areata (AA) and trichotillomania (TTM) are two common forms of non-scarring hair loss encountered in clinical practice. TTM is a compulsive disorder characterized by the irresistible urge to pull out hair leading to bizarre-shaped patches of hair loss1. AA is an autoimmune disorder that typically presents with sharply demarcated patches of hair loss. Since the treatment strategies and prognosis of these disorders are different, it is important to differentiate them using non-invasive methods such as dermatoscopy since scalp biopsy is not frequently accepted by the patients. Concerning the dermatoscopic features, not much work has been done on TTM compared to AA.
Methods
The present cross-sectional and observational study was conducted in the outpatient department of Dermatology, Venereology, and Leprosy in Sri Guru Ramdas Institute of Medical Sciences and Research, Sri Amritsar, between January 2019 and September 2020.
Only patients with the clinical diagnosis of AA or TTM were included. Any other scalp disease, such as androgenetic alopecia, seborrheic dermatitis, and tinea capitis, were excluded from our study. The diseased area of the scalp was examined, and the diagnosis of AA and TTM was made clinically. Well-demarcated patches of hair loss with hair broken at equal lengths favored the diagnosis of AA, whereas irregular patches of hair loss with hair broken at varying lengths favored the TTM diagnosis. TTM patients had a history of relief of stress with picking of hair, unlike AA patients. This macroscopic examination was followed by the dermatoscopic examination of the scalp with Dermlite DL4 dermatoscope to see the various hair follicle structures and hair shaft patterns. Informed consent was taken from each patient. Approval from the Institutional Ethics Committee was taken.
Results were tabulated and analyzed statistically using SPSS Software 19.0 version. Percentages and mean values were calculated wherever applicable. For establishing relation between AA and TTM, correlation coefficient (r) was calculated. Results were considered significant if value of probability ‘p’ < 0.05 and highly significant if ‘p’ < 0.01.
Results
We included 86 patients in the study, 76 patients with AA and 10 patients with TTM. Out of total patients, there were 40 males and 46 females. The mean age of presentation in the study was 30.6 years with a standard deviation of 14.52 years.
Trichoscopic features of AA
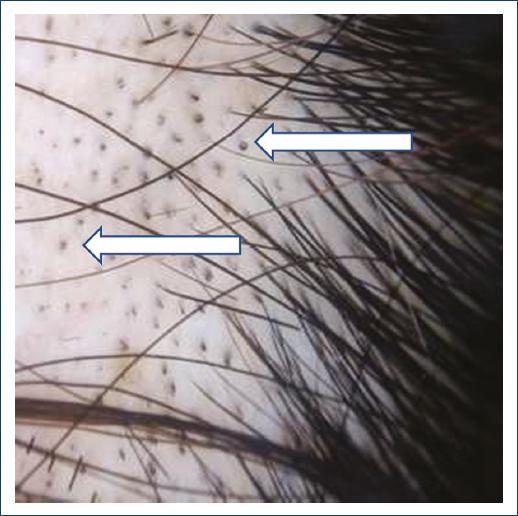
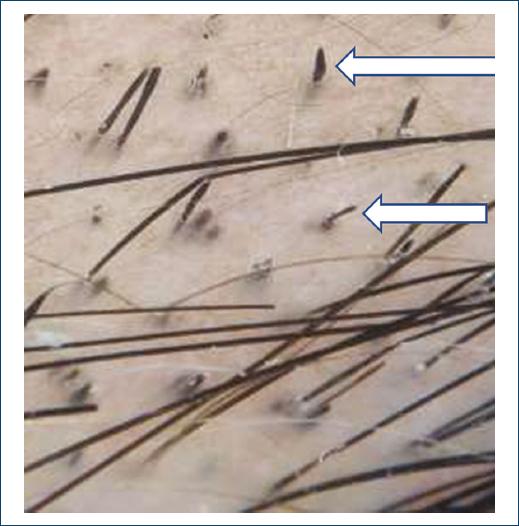
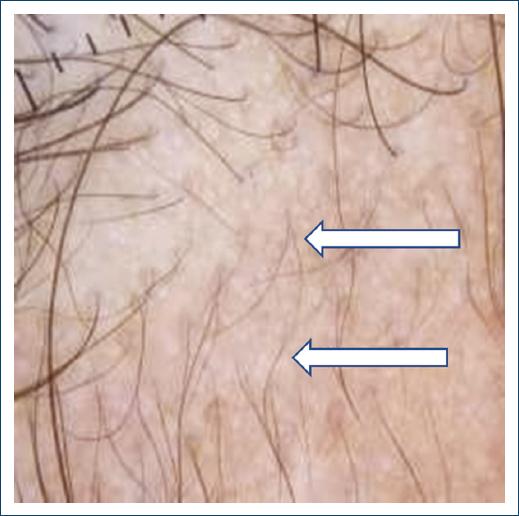
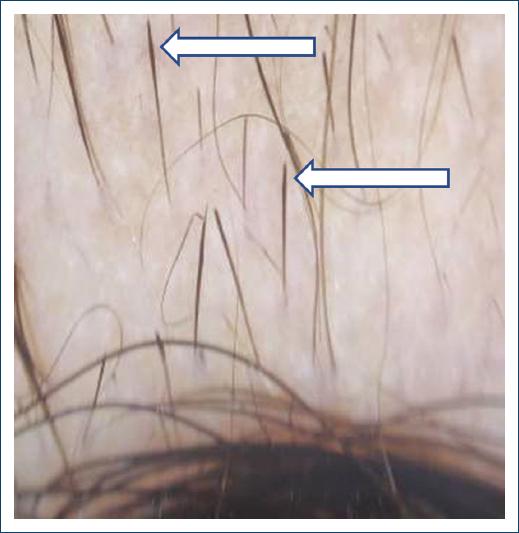
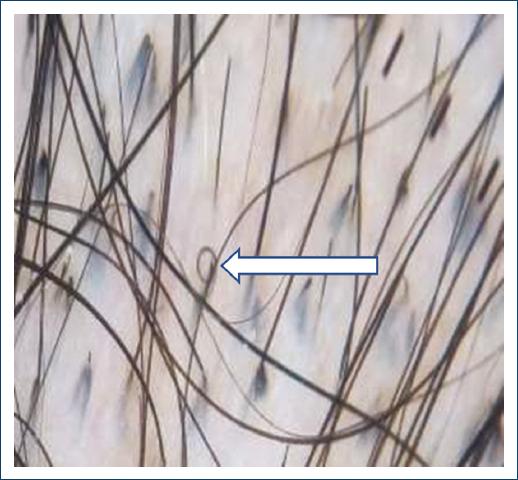
Among the 76 patients diagnosed with AA, the most common trichoscopic finding was black dots (Fig. 1) seen in 51 patients (67.1%), broken hair (Fig. 2) seen in 50 patients (65.7%), short vellus hair (Fig. 3) seen in 36 patients (47.3%), tapering hair (Fig. 4) in 27 patients (35.5%), yellow dots (Fig. 5) in 23 patients (30.2%), pigtail hair in 18 patients (23.6%), coudability hair (Fig. 6) in 16 patients (21.05%), tulip hair (Fig. 7) in 8 patients (10.5%), upright regrowing hair in 6 (7.89%) patients, and split ends (Fig. 8) in 4 (5.26%) patients (Table 1).
Table 1 Trichoscopic features of alopecia areata (n = 76)
| Trichoscopic features | No. | % |
|---|---|---|
| Black dots | 51 | 67.11 |
| Yellow dots | 23 | 30.26 |
| Tapering hair | 27 | 35.53 |
| Broken hair | 50 | 65.79 |
| Short vellus hair | 36 | 47.37 |
| Pigtail hair | 18 | 23.68 |
| Coudability hair | 16 | 21.05 |
| Tulip hair | 8 | 10.52 |
| Upright regrowing hair | 6 | 7.89 |
| Split ends | 4 | 5.26 |
Trichoscopic features of TTM
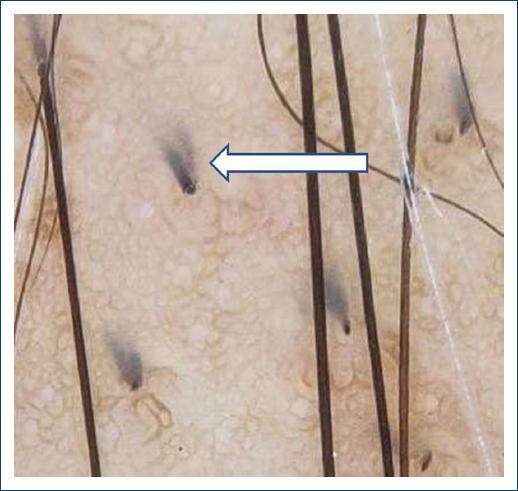
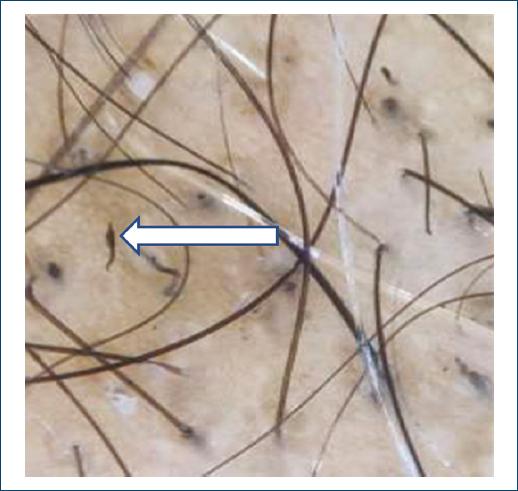
Out of 10 patients in the TTM group, the most common trichoscopic features were broken hair at varying lengths (Fig. 9) seen in 10 patients (100%), black dots in 9 (90%) patients, upright regrowing hair, split ends, and coiled hair (Fig. 10) were seen in 7 (70%) patients each, V sign (Fig. 11) and flame hair (Fig. 12) in 4 (40%) patients each, tulip hair in 3 (30%) patients, and tapering hair in 1 (10%) patient (Table 2).
Table 2 Trichoscopic features of trichotillomania (n = 10)
| Trichoscopic features | No. | % |
|---|---|---|
| Black dots | 9 | 90.00 |
| Tapering hair | 1 | 10.00 |
| Broken hair | 10 | 100.00 |
| Upright regrowing hair | 7 | 70.00 |
| Hair of varying lengths | 10 | 100.00 |
| Split ends | 7 | 70.00 |
| Coiled hair | 7 | 70.00 |
| Tulip hair | 3 | 30.00 |
| V sign | 4 | 40.00 |
| Flame hair | 4 | 40.00 |
Comparing trichoscopic features in AA and TTM
Black dots were seen in 51 (67.1%) patients of AA and 9 (90%) patients of TTM. Broken hair was seen in 50 (65.7%) patients of AA and 10 (100%) patients of TTM. Tapering hair was seen in 27 (35.5%) patients of AA and 1 (10%) patient of TTM. Tulip hair was seen in 8 (10.5%) patients of AA and 3 (30%) patients of TTM. Split ends were seen in 4 (5.26%) patients of AA and 7 (70%) patients of TTM. Upright regrowing hair was seen in 6 (7.89%) patients of AA and 7 (70%) patients of TTM.
The difference between AA and TTM in the percentage of black dots, broken hair, tapering hair, tulip hair, split ends, and upright-growing hair was statistically significant (Table 3).
Table 3 Trichoscopic features of alopecia areata and trichotillomania
| Trichoscopic features | Alopecia areata (n = 76) | Trichotillomania (n = 10) | r | p-value | ||
|---|---|---|---|---|---|---|
| No. | % age | No. | % age | |||
| Black dots | 51 | 67.11 | 9 | 90 | 0.48 | 0.046* |
| Broken hair | 50 | 65.9 | 10 | 100 | 0.37 | 0.044* |
| Tapering hair | 27 | 35.53 | 1 | 10 | 0.43 | 0.034* |
| Tulip hair | 8 | 10.52 | 3 | 30 | 0.42 | 0.035* |
| Split ends | 4 | 5.26 | 7 | 70 | 1.00 | 0.000 |
| Upright regrowing hair | 6 | 7.89 | 7 | 70 | 1.00 | 0.000 |
*Significant at 0.05 level of significance.
Discussion
AA is one of the most common forms of hair loss seen by dermatologists and accounts for 25% of all cases of alopecia2. In the general population, the prevalence was estimated at 0.1-0.2%, with a lifetime risk of 1.7%3. It is characterized as a non-scarring form of hair loss involving the scalp and/or body without any clinical inflammatory signs. AA typically presents with well-defined, regular, circumscribed patches of hair loss with hair broken at equal length4.
TTM is another form of non-scarring alopecia resembling AA. The disorder most commonly affects children between the age group of 9-13 years with female preponderance1. The scalp is the most common site, but it can also involve eyebrows, eyelashes, facial hair, axillary and pubic hair5. Clinically, patients present with irregular localized patches of hair loss with broken hairs of varying lengths, mainly in the frontoparietal area and the vertex6.
Diagnosis and treatment of these groups of disorders can be challenging. Even with careful clinical evaluation and proper history taking, the diagnosis can be missed. The diagnosis cannot be based per se on hair evaluation methods because of the variations in sensitivity and invasiveness of procedures, such as scalp biopsy, which are not frequently accepted by the patients7. So besides basic evaluation, it is important to have easy-to-use and non-invasive office tools such as dermatoscope that aid in performing the diagnosis and help to interpret the overlapping features of these hair disorders.
The diagnosis of AA cannot be made based on a single dermatoscopic feature but needs the combination of various dermatoscopic features. In our study, the combination of black dots, tapering hair, and broken hair was specific and diagnostic for AA. A similar trichoscopic picture can also be seen in TTM with different characteristics of broken hair and black dots. Furthermore, we reported that the V sign, coiled hair, and flame hair are exclusively seen in TTM.
Tapering hair (aka exclamation mark hair) is considered to be pathognomonic of AA and a marker of the disease activity8. In our study, tapering hair was more frequently observed in not only in AA patients but also in TTM with a statistically significant difference. Rakowska et al. also observed a higher number of patients with exclamation mark hair in AA (81%) as compared to TTM (16%)6. Rakowska et al. also demonstrated the comparison of tapering hair seen in AA and TTM. The tapering hair in TTM has a flat distal end with a pigmented proximal end, whereas the tapering hair in AA has a frayed and uneven distal end with a hypopigmented proximal end6.
We observed a statistically significant difference in the occurrence of black dots in patients of AA and TTM, with a higher number of black dots in AA patients, in agreement with the findings of Chiramel et al.9, Rakowska et al. observed that black dots in AA are of uniform size and shape whereas in TTM, they are of variable diameter and shape6.
Broken hair is formed due to the breakage of hair shafts at a different distance from the scalp surface. Ankad et al. in a study with 10 TTM patients observed broken hairs of varying lengths in 100% of patients10, similar to our findings and to the study of Chiramel et al.9. Broken hair occurs both in AA and TTM, but in TTM, broken hairs typically have varying lengths10.
In our study, we observed that patients with split ends, tulip hair, and upright regrowing hair were higher in TTM as compared to AA. This difference was statistically significant and similar to the findings of Rakowska et al.6.
Upright regrowing hair is short hair with a tapered distal end and thickened proximal end11. We observed upright regrowing hair in 70% of patients of TTM, comparable to the study of Ankad et al. where upright regrowing hair was observed in 80% of patients10.
Trichoptilosis refers to irregular hair with split ends. TTM is characterized by trichoptilosis affecting short hair12. Split ends were seen in 70% of TTM patients in our study, which was consistent with the findings of Chiramel et al.9.
Flame hair, coiled hair, and V-sign were only seen in TTM in our study and thus were considered to be the specific features of TTM. Similar observations have been reported by Ankad et al.10.
Flame hair refers to semi-transparent, wavy cone-shaped hair residues formed due to repetitive mechanical pulling of hair11. We reported flame hair in 40% of TTM patients, findings comparable to Ankad et al. where flame hair was seen in 30% of patients10. Rakowska et al. and Govindarajaulu SM reported flame hair in a lower percentage, respectively, 25% and 20% of patients6,8.
Coiled hair is formed as a result of hair shaft fracture and curling of the proximal part which remains attached to the scalp13. We observed coiled hair in 70% of patients of TTM which was comparable to the study of Ankad et al.10.
V sign is formed when two or more hair emerges from a single follicular opening breaking at the same length above the scalp surface11. In our study, the V sign was seen in 40% of TTM patients, a percentage similar to Ankad et al. (30%)10. Nevertheless, other studies reported a higher incidence of V sign, namely Govindarajaulu et al. (100% of pati) and Chiramel et al. observed V sign in 80% of patients8,9.
Trichoscopy has proved to be a reliable tool in the diagnosis of TTM by demonstrating distinctive dermatoscopic patterns and thus allows us to differentiate TTM from patchy AA14. Since TTM as a disease carries its social implications, early diagnosis and treatment are necessary. Dermatoscopy thus plays a vital role in the diagnosis of the disease and precludes the need for a scalp biopsy.
Conclusion
The early diagnosis using a dermatoscope helps in the timely management of non-scarring hair disorder and prevents the progression to cicatricial hair loss. Thus, the use of dermatoscopy in the clinical evaluation of these non-cicatricial alopecias enhances the diagnostic potential beyond the simple clinical examination. The combination of black dots, tapering hair, and broken hair is specific and diagnostic for AA. Broken hair at varying lengths, the V sign, coiled hair, and flame hair favors the diagnosis of TTM.