A 65-year-old man with a history of alcohol abuse presented with cicatricial alopecia and whitish sclerotic plaques in the upper chest, distributed mainly on the V area of the lower neck and lower sternum (Fig. 1). In addition, physical examination revealed a hyperpigmented area of hypertrichosis on the interparietal and left parietal region (Fig. 2).

Figure 1 White-yellow atrophic plaques in the “V” area of the upper chest with a hyperpigmented border.
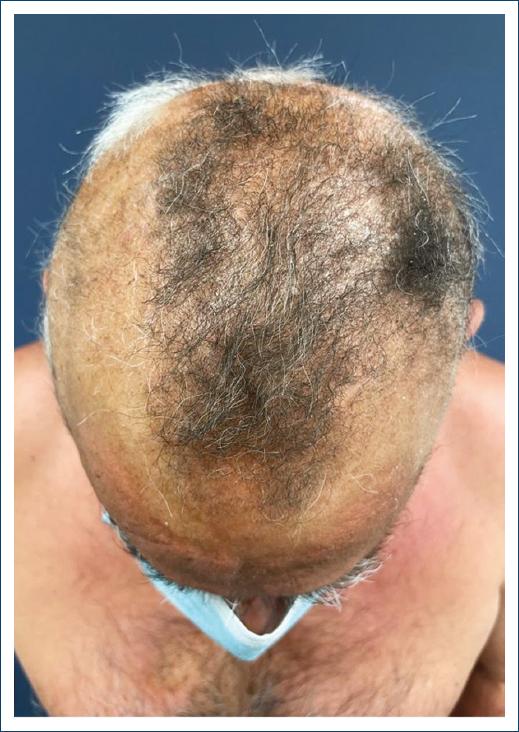
Figure 2 Alopecic patches on the scalp and hyperpigmented area of hypertrichosis on the interparietal and left parietal region.
Laboratory evaluation showed iron overload and elevated transaminases. Antinuclear antibodies and infectious serologies, including borrelia, were negative. A cutaneous biopsy of the scalp and neck was compatible with morphea, and thus, narrow band ultraviolet B phototherapy was initiated.
One month later, the patient reported blistering and crusting of the forearms. Urine analysis revealed increased uroporphyrins establishing the diagnosis of porphyria cutanea tarda (PCT). The patient was started on bimonthly phlebotomies, and photoprotection and alcohol withdrawal were recommended.
Sclerodermiform changes have been reported in 2% of PCT patients1,2. Clinically, lesions may resemble morphea, presenting with hyperpigmentation rather than a peripheral lilac ring3,4. Scalp lesions may present as scarring alopecia, also called alopecia porphyrinica3. Isolated sclerodermiform changes, without the typical clinical picture of PCT, pose a diagnostic challenge. Histopathology cannot reliably distinguish morphea from sclerodermiform PCT4. Given the clinical and pathological resemblance, one must consider this alternative diagnosis, especially when facing therapy failure.














