Introduction
Telogen effluvium is a scalp disorder featured by diffuse, non-scarring hair loss1. It may be caused by any disturbance to the hair cycle, resulting in increased and synchronized telogen shedding2. Acute telogen effluvium (ATE) is defined as hair shedding lasting for < 6 months1 and more frequent in the third decade of life3. Chronic telogen effluvium is a condition lasting for more than 6 months with a prolonged unpredictable course and it usually affects middle-aged women1. In general, the cases of ATE are subclinical, and therefore, its true incidence or prevalence is mostly unknown2. An excessive hair shedding without the formation of a glabrous area is a common phenomenon4. Both males and females are affected, but the ratio of females is higher. Nevertheless, it should be regarded that women consider hair-shedding problems more seriously and they probably seek medical help more often1. Despite the subjective complaints of excessive hair loss, objective attributes may completely be absent2. However, the disorder is so frightening that it urges the patient to visit a physician immediately4. Patients usually complain of increased hair loss during washing or brushing. They may even bring in bags of shed hair to prove the quantity of loss. They are often very anxious that they will go bald if this goes on. On examination, in general, there is a normal scalp with an absence of inflammatory signs or follicular miniaturization2. Any evidence of erythema, scaling, inflammation; altered hair density; changes in shaft caliber, length, shape, or fragility may indicate other diagnoses5.
ATE may be related to various offenses that can be physical, chemical, or emotional. In general, hair loss occurs approximately 3 months after the trigger exposure1, however, the observation of increased telogen hair shedding does not always suggest a cause. In addition, the patients usually do not relate these events to the recent insults they faced6, and the cause remains unknown in many cases1. The histopathology of the ATE is non-specific and looks like that of a normal scalp. This may be due to a delayed biopsy, generally performed when the harmful event is no longer active because of the notorious 3-month lag4. Increased physiological stress such as surgical trauma and hemorrhage, high fever, and chronic systemic illness can cause ATE1. Thyroid dysfunction, hyperandrogenism, and hyperprolactinemia are catagen-inducing endocrine disorders2. Thyroid receptors exist in outer root sheath cells and they regulate the frequency of the hair cycle. In general, while hypothyroidism results in decreased frequency of anagen, hyperthyroidism leads to thin hairs. The severity of hair loss is not directly related to the severity of the endocrine abnormality and telogen effluvium can be the only manifestation of subclinical hypothyroidism7. Androgens show an inhibitory effect on the hair follicles of the scalp8. The mechanism of prolactin in regulating hair growth is related to its inhibitory effect on hair shaft elongation and the premature induction of the catagen phase. Prolactin is also recognized as an androgen metabolism modulator, increasing the level of free testosterone and dehydroepiandrosterone sulfate9. Childbirth can also cause excessive hair to enter the telogen phase1. Micronutrients such as vitamins and minerals play an important, but not entirely clear role in normal hair follicle development. The roles of folate and vitamin B12 in nucleic acid production imply that they may have functions in the highly proliferative hair follicle physiology. Furthermore, the association of hair loss and iron deficiency has been debated for many years10. Numerous drugs can cause telogen hair loss and even changes in the dosage of drugs can also lead to excessive shedding. Drugs that can cause telogen effluvium include oral contraceptives, androgens, retinoids, beta-blockers, angiotensin-converting enzyme inhibitors, anticonvulsants, and antidepressants1. Emotional stress is commonly ascribed as a cause of ATE. Stress is probably a negative hair growth modulator in humans, presumably with profound effects2. It is both an inducer of telogen effluvium and a concomitant response secondary to hair loss. Neurohormones, neurotransmitters, and cytokines are secreted during the systemic stress response. The existence of a brain-hair follicle axis is suggested to represent the specific relationship between a stressor and a premature arrest of the hair cycle11.
In this study, it was retrospectively analyzed the 3-month outcome of the female patients who referred to our hospital with ATE without any visible sign.
Methods
Two hundred and sixty-six caucasian female patients between 13 and 58 years old, who referred to our hospital dermatology outpatient clinic with hair loss complaints, which began in the last 6 months, in the years 2017-2019 (that is, before the COVID-19 pandemic, which is known to cause telogen effluvium frequently) were retrospectively recruited. All of the procedures were performed in rapport with the ethical principles established for medical research (Helsinki Declaration of World Medical Association 1975, and amendments as revised in 1983). The mean age (MA) ± standard deviation (SD) of the patients was 28 ± 10. They declared excessive shedding which was noticed by themselves or other households. The patients were not using any topical or systemic medications at least for 3 months, they had no scalp or hair disease and none of them were pregnant or in the lactation period. On examination of each patient, there was an essentially normal scalp with an absence of inflammatory signs or follicular miniaturization, and hairs had normal thickness. There were no signs or symptoms of hyperandrogenism. The patients did not declare a solid physical or mental stress in 3 months before the initiation of the complaints. All patients were analyzed for the same parameters in the biochemistry blood laboratory. The searched parameters and their lowest and highest normal values were iron: 40-150 μg/dL, iron-binding capacity (IBC): 200-400 μg/dL, vitamin B12: 134-590 pg/μL, folate: 2.4-12.6 ng/mL, thyroid-stimulating hormone (TSH): 0.27-4.2 μU/mL, and prolactin: 3.34-26.72 ng/mL. The patients were analyzed in five different age groups, each corresponding to a decade. The age groups, MA ± SD, and patient numbers in each group are depicted in figure 1.
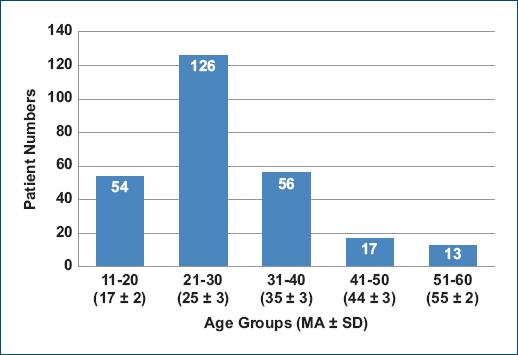
Figure 1 The distribution of patients in each decade and their mean age ± standard deviation values. MA ± SD: mean age ± standard deviation.
For treatment, all patients were prescribed 400 IU vitamin E (α-tocopherol) and 50 mg zinc supplements daily, whether they had all normal or some outside normal laboratory values. In addition to standard supplements, the medications prescribed to the patients with abnormal values were; for iron deficient patients 80 mg Fe+2/day PO, for vitamin B12 deficient patients 1 mg cyanocobalamin/day PO both for 3 months; and for the patients with hyperpolactinemia 0.250 mg cabergoline once in every 3 days PO, 1 mg total. All the patients were requested to use the prescribed supplements and medications according to the instructions and invited to a second visit 3 months later.
Results
The mean value ± SD of each parameter according to age groups and each mean value’s percentile score (PS) are shown in table 1. All of the mean values for all parameters were in normal ranges in all age groups. PS denotes the place of any normal mean value in the whole normal range of relevant parameters and is calculated as: Current Mean Value-Lowest Limit of Normal Range (LLNR)/Highest Limit of Normal Range (HLNR)-LLNR. In general, it should be emphasized that, although in normal ranges, iron PSs in all age groups were closer to the lowest limit, when compared with the PSs of other parameters.
Table 1 The mean value ± standard deviation of each parameter according to age groups and each mean value’s percentile score
| Age group | Iron | IBC | Vitamin B12 | Folate | TSH | Prolactin |
|---|---|---|---|---|---|---|
| 11-20 | ||||||
| MV ± SD | 82 ± 22 | 292 ± 54 | 341 ± 135 | 7.9 ± 1.6 | 2 ± 0.8 | 16 ± 7 |
| PS | 38.1 | 46 | 45.3 | 53.9 | 44 | 54.1 |
| 21-30 | ||||||
| MV ± SD | 79 ± 24 | 302 ± 55 | 328 ± 114 | 7.7 ± 1.4 | 1.9 ± 1 | 17 ± 10 |
| PS | 35.4 | 51 | 42.5 | 51.9 | 41.4 | 58.4 |
| 31-40 | ||||||
| MV ± SD | 72 ± 22 | 316 ± 68 | 336 ± 134 | 7.6 ± 1.6 | 2.2 ± 1.8 | 12 ± 5 |
| PS | 29 | 58 | 44.2 | 50.9 | 49.1 | 37 |
| 41-50 | ||||||
| MV ± SD | 71 ± 24 | 313 ± 44 | 334 ± 140 | 8.2 ± 1 | 1.7 ± 0.9 | 14 ± 6 |
| PS | 28.1 | 56.5 | 43.8 | 56.8 | 36.3 | 45.5 |
| 51-60 | ||||||
| MV ± SD | 70 ± 17 | 298 ± 42 | 362 ± 101 | 8.5 ± 1 | 1.9 ± 1.6 | 8 ± 4 |
| PS | 27.2 | 49 | 50 | 59.8 | 41.4 | 19.9 |
| Total | ||||||
| MV ± SD | 77 ± 23 | 303 ± 57 | 334 ± 124 | 7.8 ± 1.5 | 2 ± 1.2 | 16 ± 14 |
| PS | 33.6 | 51.5 | 43.8 | 52.9 | 44 | 54.1 |
MV ± SD: mean value ± standard deviation; PS: percentile score.
The patients whose values were outside the normal ranges were also analyzed (Table 2). Without regarding the age groups, all of the patients with abnormal values were included in this analysis, grouping them as; those who have mean values lower than the LLNR, mean values higher than the HLNR, and sum of the first two items as outside the limits of normal range (OLNR). Furthermore, the ratios of mean values to LLNR and HLNR for all parameters were calculated to assess the divergences of abnormal values from the normal ranges. As it is seen in table 2, the highest divergence of low values is −27% (that is, iron: 0.73-1/1) and of high values is +43% (that is, TSH: 1.43-1/1) from LLNR and HLNR, respectively. It should also be stated that in addition to relatively low divergence ratios, the ratios of patients having abnormal values in the whole patient population for any single parameter are also quite low (that is, OLNR%, between 4.5% and 6.4%). It is mentionable that the patients who had iron values lower than LLNR and the patients who had IBC values higher than HLNR were the same individuals. Folate levels were quite consistent and neither low nor high levels were found in all patient population. All patients who had either low or high TSH values were further analyzed for their free T3 and T4 values, and all were found in normal ranges. Therefore, these TSH values were considered normal and no medication was prescribed for them. Furthermore, the patients who had solitarily higher vitamin B12 levels than HLNR were not prescribed any medication. Because some patients had more than one abnormal value needing medication, they were given more than one medication. Totally, 25 (9.4%) patients had one or more medications.
Table 2 The analyses of the patients whose values were outside the normal ranges
| Parameters | Lower than LLNR | Higher than HLNR | Total OLNR | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | MV ± SD | MV/LLNR | n | % | MV ± SD | MV/HLNR | n | % | |
| Iron | 12 | 4.5 | 29 ± 5 | 0.73 | NA | NA | NA | NA | 12 | 4.5 |
| IBC | NA | NA | NA | NA | 12 | 4.5 | 453 ± 28 | 1.13 | 12 | 4.5 |
| Vitamin B12 | 5 | 1.9 | 114 ± 12 | 0.85 | 12 | 4.5 | 725 ± 98 | 1.23 | 17 | 6.4 |
| Folate | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| TSH | 4 | 1.5 | 0.2 ± 0.1 | 0.74 | 9 | 3.4 | 6 ± 2.2 | 1.43 | 13 | 4.9 |
| Prolactin | NA | NA | NA | NA | 14 | 5.3 | 38 ± 12 | 1.42 | 14 | 5.3 |
MV ± SD: mean value ± standard deviation; LLNR: lowest limit of the normal range; HLNR: highest limit of the normal range; OLNR: outside the limits of the normal range; NA: non-applicable.
Two hundred and nine patients came to the second visit after the 3-month treatment period. Of these patients, 19 (9.1%) stated that hair shedding ceased totally, 156 (74.6%) diminished to some extent, and 34 (16.3%) continued as before. The number of patients who had medication(s), namely who had abnormal value(s), in these groups, was 2, 19, and 4; and their ratios to the patients in each group were 10.5%, 12.2%, and 11.8%, respectively.
Discussion
Previously, it was declared that the tendency to ATE was highest in the third decade, probably due to more frequent health changes, such as pregnancy and deliveries, tubal ligations, starting and stopping oral contraception, menorrhagia associated with fibroids, and extreme weight fluctuations due to pregnancies3. In the current analysis also, among the age groups, the highest patient number belonged to the 21-30 group, that is, the third decade of life (Fig. 1).
Considering the mean values, all parameters in our study were found in normal ranges for both the entire patient population and age groups (Table 1). Furthermore, it should be emphasized that the PSs of all parameters were around 50%, suggesting a normal distribution, except for iron. The relatively low values of iron PSs might be due to the ethnic tendency of Turkish women toward lower serum iron values12,13. However, due to normal mean values, it should be considered that none of the analyzed parameters can directly be accused as the cause of the hair sheddings. On the other hand, in addition to the relatively low numbers of patients whose one or more values were outside the normal ranges, it was found that divergence ratios of their values from LLNR and HLNR were also quite low (Table 2). Therefore, it might be suggested that even for the individual patients whose values were outside the normal ranges, it was quite probable that their complaints were not related to these mild abnormal values. The comparable ratios of the patients who had medications (that is, the patients with abnormal values) in all three groups, as 10.5%, 12.2%, and 11.8%, whether declared the shedding had stopped, diminished, and continued, respectively; might also suggest that the abnormal values had no role in their complaints.
In ATE, fear and stress usually arise from the inability to comprehend that a completely healthy person can still have hair loss2. In general, patients with this complaint often believe that there is a terrible disease sneaking internally, causing hair loss despite repeated normal laboratory results and no other symptoms of any kind3. The characteristic wording in such cases is: “I always had a full head of hairs and now I am losing them by the handful.” Actually, the typical patient is a lady who still has a “full head of hairs”4. Patient education is important in disease management. Treatment for ATE is primarily reassurance and counseling. An assurance that ATE will not lead to baldness is quite helpful3. In our experiences, it also works well to comfort the patient by emphasizing that shedding itself is not important if there is no rarefaction or thinning of the hairs, as the body compensates for the shedding. Enthusiastic management and observation are usually appropriate as shedding is expected to cease within three to 6 months2. Compatible with these reports, at the end of 3rd month, 83.7% of our patients declared their shedding had ceased or diminished to some extent.
There is no sufficient evidence to indicate micronutrients and vitamin prescription for telogen effluvium. An old tradition incriminates the deficiency of iron for hair loss4, but its role during the hair cycle has not been well studied and there are contradicting reports on the efficacy of the replacement of iron on the outcome of telogen effluvium. Indeed, large double-blind placebo-controlled trials are required to determine the effect of specific micronutrient supplementation on hair growth in those with both micronutrient deficiency and non-scarring alopecia to establish any association between them10. However, in our opinion, although there is insufficient data for any kind of supplementation for this condition, the expectations of the patients from the physicians are so great that it will be wise to prescribe some supplements, at least for their placebo effects. Otherwise, the feeling of dissatisfaction may urge the patients to seek other advices. Therefore besides prescribing the medications for the parameters that we found deficient in biochemical analysis, we additionally prescribed zinc and vitamin E supplements to all patients whether they had any deficiency for the searched parameters or not. Zinc and vitamin E were selected because of their anti-oxidant effects14,15. Vitamin E consists of fat-soluble compounds known as tocopherols and tocotrienols which function by scavenging peroxyl radicals16. Eight months of supplementation with 50 mg of mixed tocotrienols and 23 IU of α-tocopherol resulted in a 34.5% increased hair count in 38 patients with hair loss, compared to a 0.1% decrease with placebo17. Zinc has an essential role in both the structure and function of a range of proteins, transcription factors, enzymes, and hormone receptor sites18. However, there are conflicting data from the studies, while some of them concluded that zinc level was significantly lower in telogen effluvium patients19,20, some others declared no statistical difference between patients and controls21,22. In the current study, of course, we do not have any evidence of whether they had any effect on the patients and if affected, whether that was due to their anti-oxidant and other relevant features, placebo effects, or both.
Scalp hair is an important accessory of humans and the apprehension of shedding may have deep impacts on the patients’ emotions. It generally incites more intensive distress than its objective severity and for some patients, the emotional burden of hair shedding may be comparable to a life-threatening disease. Therefore, even if the patient has no visible signs but anxiety, the physician should not underestimate the complaints of these patients. Otherwise, it is quite probable that they will attempt to find a new physician or carry out the advices of laypeople. Initially, when the patient first referred with hair shedding complaint that commenced recently, after an incomprehensive biochemical blood test regarding the likely responsible hormones and vitamins/minerals, the reassurance of the patient by stating the benign prognose that the shedding would cease up to 6 months, will soothe the patient. Even if no abnormality is found in the test results, it is strongly recommended to prescribe some supplements due to the emotional dissatisfaction and vulnerability of these patients. Although they are extremely frustrated, if these patients are helped in an understanding and expectant way, often they are quite grateful.
Conclusions
Considering the normal mean values, low divergence ratios, and low ratios of abnormal values in the whole patient population; none of the analyzed parameters in the current study can directly be accused as the cause of the hair sheddings. In ATE the cause remains unknown in many cases and the patients generally refer without any objective sign, but with deep frustration. Treatment for ATE is primarily reassurance and counseling. Although there is insufficient data for any kind of supplementation for this disorder, the expectations of the patients from the physicians are so great that it will be prudent to provide some supplements, at least for their placebo effects. An enthusiastic management and observation are usually appropriate, as shedding is expected to cease within three to 6 months.














