Introduction
Cutaneous leishmaniasis typically presents as one or a few painless ulcers with infiltrated edges in exposed areas of the body1. However, diverse forms have been described in the literature2,3, influenced by the host’s immune response, affected locations, and Leishmania species4,5.
In the state of Rio de Janeiro, leishmania (Vienna) braziliensis is the predominant species, and different genotypes have not been associated with clinical variability6.
Sporotrichoid leishmaniasis (LE) can manifest as an ulcer, lymphangitis, nodules, or ulcerated lesions along its course, resembling the typical presentation of sporotrichosis2,5,7.
Clinical case
A female patient sought dermatological care at Fiocruz, located in the city of Rio de Janeiro, State of Rio de Janeiro, referred by a fellow dermatologist.
The patient reported that, 3 months before the consultation, an erythematous papule appeared on her right hand after a mosquito bite. It soon became ulcerated with a progressive growth that occupied almost the whole dorsum of the right hand within a few weeks. Several small, isolated erythematous nodules appeared along the lymphatic tract of the right forearm. Despite receiving treatment for sporotrichosis with itraconazole at a dosage of 200 mg/day for 1 month, there was no improvement.
Regarding her medical history, she reported a diagnosis of diabetes mellitus under treatment with metformin and denied alcoholism or smoking in her history.
During the physical examination, a painless, large, and relatively superficial ulcer with central crusts measuring approximately 5 cm was observed on the dorsum of the right hand, and it was limited by infiltrated violaceous edges and surrounding erythema (Fig. 1). Along the anterior right forearm, there were multiple painless ascending erythematous papules and nodules (Fig. 2). There was no one palpable lymph node on the right axillae.
From a laboratory perspective, blood count, fasting blood glucose, glycated hemoglobin, hepatogram, VDRL, and anti-HIV were normal, while leishmania serology was reactive. A radiograph of the right hand showed no signs suggestive of a bone injury.
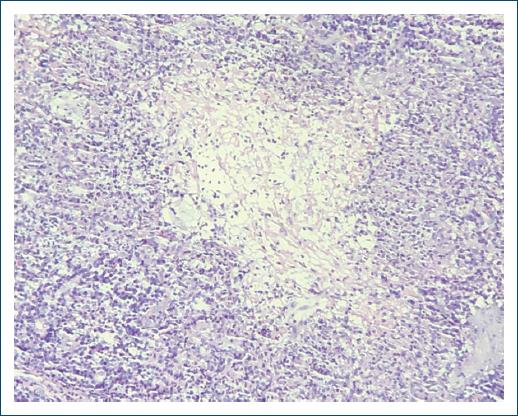
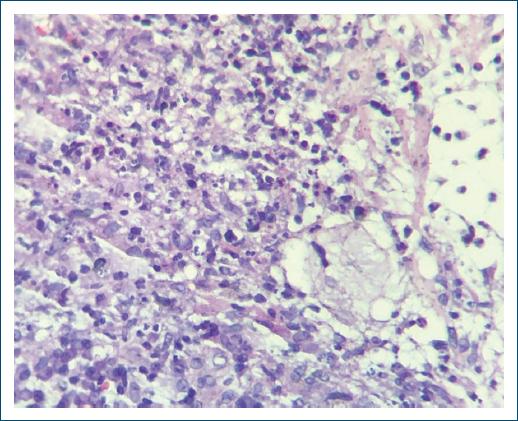
Histopathological examination revealed a cluster of hyperplastic squamous epithelial cells within the deep dermis (pseudoepitheliomatous hyperplasia) at lower magnification (Fig. 3). At higher magnification, a granuloma with central necrosis was observed (Fig. 4), with an intermediate area containing epithelioid cells and an outer zone with plasma cells, lymphocytes, and a few neutrophils and intracellular inclusions suggestive of Leishman bodies by hematoxylin and eosin staining (Figs. 4 and 5). In direct mycological examination revealed motile, flagellated promastigote forms grouped in a “rosette” conformation (Fig. 6).
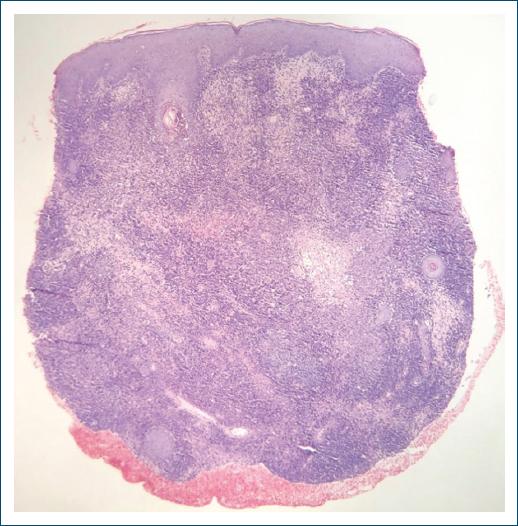
Figure 3 Lower magnification section stained with hematoxylin and eosin showing pseudoepitheliomatous squamous hyperplasia and a dense granulomatous dermal infiltrate up to the deep dermis (×H&E 40).
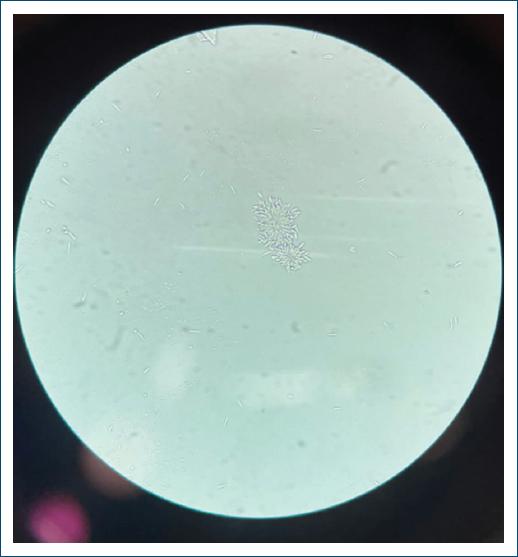
Figure 6 Motile, flagellated promastigote forms grouped in a “rosette” conformation (optical microscope ×100).
An electrocardiogram showed a QTc interval of 0.435 s (normal), an observation by otorhinolaryngology that did not detect a mucosal lesion.
For treatment, pentavalent antimony was administered intravenously in a low-dose regimen of 5 mg/kg/day for 30 days. The patient returned after 45 days, reporting significant improvement in the lesions, remaining only a residual scar (Fig. 7).
Discussion
Cutaneous leishmaniasis is considered a public health problem in around 88 countries, with approximately 1.5 million cases reported annually. It is considered by the World Health Organization (WHO) as one of the six most important infectious diseases due to its high detection rate and capacity to produce deformities1.
In Brazil, American cutaneous leishmaniasis (ACL) is one of the dermatological diseases that deserve more attention due to its magnitude as well as its potential to generate deformities. It has a wide distribution with reported cases throughout the national territory1.
Sporotrichosis is a subacute and chronic fungal infection caused by species of the Sporothrix spp. genus. Notably, S. brasiliensis is responsible for an epidemic in Rio de Janeiro linked to feline zoonotic transmission3. Compulsory reporting in Rio de Janeiro since 2013 revealed predominance in women (61%) and a higher incidence in individuals aged 40-598. The infection commonly results from traumatic inoculation, often through contact with contaminated soil or through scratches and bites from infected cats9,10. Eventually, report the typical sporotrichoid presentation, as occurred in our case.
The typical ulcer of cutaneous leishmaniasis (CL) is painless and usually located in exposed areas of the skin. It has a rounded shape, measuring from a few millimeters to a few centimeters, erythematous, infiltrated, and firm consistency, well-defined and elevated borders, and a reddish base with coarse granulations. An associated bacterial infection may cause local pain and produce seropurulent exudate that, when dried into crusts, covers the ulcer’s base partially or completely.
Typical presentations of cutaneous leishmaniasis include a sporotrichoid form, clinically described as a primary ulcer associated with lymphangitis and nodules, with or without ulcerated lesions along its course. In a city like Rio de Janeiro, where both leishmaniasis and sporotrichosis can coexist, this represents a major challenge for dermatologists.
Other types of less common cutaneous lesions may be encountered. Initial lesions often appear as nodules, located deep in the hypodermis, or small papules resembling insect bites, which evolve by increasing in size and depth (papulotuberosal lesions) and ulcerating at the apex. Vegetating lesions are characterized by a papillomatous, moist appearance and a soft consistency. Verrucous lesions are characterized by a dry, rough surface with the presence of small crusts and scaling. These two types of lesions can be primary or evolve from ulcers. Around the main lesion, subcutaneous induration and satellite papules may appear, which can coalesce to form plaques. New lesions of LC may arise in traumatized areas.
The main differential diagnoses include other infectious diseases such as syphilis, leprosy, tuberculosis, atypical mycobacterioses, paracoccidioidomycosis, histoplasmosis, lobomycosis, sporotrichosis, and chromoblastomycosis. Tumorous conditions such as keratoacanthoma, basal cell carcinoma, squamous cell carcinoma, histiocytoma, and cutaneous lymphoma are also considered. In addition, other conditions such as sarcoidosis, discoid lupus erythematosus, psoriasis, Jessner’s lymphocytic infiltration, and vasculitis should be considered.
The first-line drugs for the treatment of leishmaniasis are pentavalent antimonials (Sb+5). To standardize the treatment regimen, the World Health Organization (WHO) recommends that the dose of this antimonial should be calculated in mg Sb+5/kg/day. There are two types of pentavalent antimonials that can be used: meglumine antimoniate and sodium stibogluconate, the latter of which is not commercially available in Brazil.
In localized and disseminated cutaneous forms, the recommended dose varies between 10 and 20 mg Sb+5/kg/day, suggesting 15 mg Sb+5/kg/day for both adults and children for 20 consecutive days1.
Several side effects have been reported in the literature, such as arthralgia, myalgia, anorexia, nausea, vomiting, epigastric pain, abdominal pain, pancreatitis, weakness, headache, dizziness, palpitations, insomnia, and acute renal failure (ARF). These complaints are generally mild and rarely require treatment suspension. However, at a dose of 20 mg Sb+5/kg/day, the antimonial can reach its toxicity threshold, leading to cardiac, pancreatic, or renal alterations that may necessitate treatment discontinuation11.
One of the main adverse effect of Sb+5 is due to its action on the cardiovascular system. This effect is dose- and time-dependent, manifesting as a repolarization disturbance (inverted and flattened T wave and increased QT interval). Weekly electrocardiograms and careful daily cardiac auscultation should be performed until the end of medication, always before each infusion, to detect arrhythmias. If this occurs, the patient should be thoroughly evaluated, and if necessary, the medication should be discontinued and a second-line drug should be prescribed. For this reason, we opted to use the low-dose regimen of pentavalent antimonials.
According to the study, the standard treatment (10-20 mg Sb5+/kg/day for 20 days), the low-dose regimen (5 mg Sb5+/kg/day for 20 days), and intralesional infiltration demonstrated effectiveness of 95.3%, 84.3%, and 75.9%, respectively11.
At present, there are few cases of sporotrichoid Leishmaniasis described in the literature9.
In most cases, the correct diagnosis is delayed, especially in regions where both diseases coexist, which can become a challenge. Therefore, its recognition is essential for the early and correct implementation of therapy to avoid harm both to the patient and the health-care system.
Ultimately, histopathology (a granuloma with central necrosis, epithelioid cells, and an outer zone with plasma cells, lymphocytes, and intracellular inclusions suggestive of Leishman bodies) and access to appropriate laboratory tests enabled an accurate diagnosis and effective treatment, aiming to reduce morbidity and prevent the formation of scars.