A 51-year-old man, with skin type V according to the Fitzpatrick scale, with human immunodeficiency virus (HIV) infection currently receiving highly active antiretroviral therapy, and with an undetectable viral load, presented with a 3-week history of asymptomatic lesions on his back and arms. Clinical examination revealed multiple pin-point, round, white-colored, flat-topped papules, some clustered, and others arranged linearly (Fig. 1A). Dermoscopic examination uncovered several white, well-circumscribed, circular areas measuring 0.5-1 mm in diameter, characterized by a smooth surface with a central brown shadow (Fig. 1B and C). Histopathological analysis of a biopsy specimen revealed epidermal hyperplasia encompassing a central area of atrophy and erosion. This was accompanied by a focal dense lymphohistiocytic infiltrate in the upper dermis, with surrounding hyperplastic rete ridges forming a distinctive “ball and claw” configuration (Fig. 1D). These findings were consistent with a diagnosis of lichen nitidus (LN).
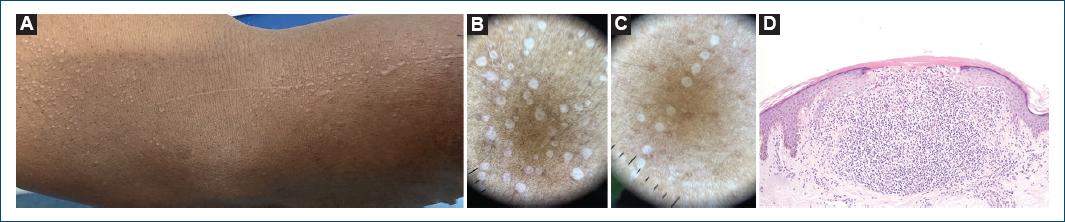
Figure 1 Lichen nitidus. A: numerous pinhead-sized white papules on the flexural aspect of the arm, some clustered and some in a linear distribution. B and C: dermoscopy of multiple white, well-circumscribed, circular areas measuring 0.5-1 mm in diameter, characterized by a smooth surface with a central brown shadow – clustered (B) and linearly (C) (DermLite DL4; polarized, ×10). D: histopathologic picture revealing epidermal hyperplasia surrounding a central zone of atrophy and erosion; focal dense lymphohistiocytic infiltrate in the upper dermis, with surrounding hyperplastic rete ridges in a “ball and claw” configuration (H&E, ×40).
LN is an uncommon idiopathic chronic eruption with an unknown etiology and pathogenesis. Predominantly, LN cases manifest in pediatric and young adult populations1. It presents with multiple small, uniform, shiny, and asymptomatic papules, typically localized in the flexor aspects of the upper extremities, abdomen, and genitalia1,2. The Koebner phenomenon serves as a hallmark of LN3. Dermoscopy proves to be a valuable tool, revealing well-demarcated, smooth, white circles with a discernible brownish shadow within4. A definite diagnosis, as described in the reported case, relies on histopathological evaluation2,3. Given its typically asymptomatic nature and tendency to spontaneous resolution within months to a year, treatment primarily targets symptomatic or generalized cases of LN. Therapeutic options include topical corticosteroids, topical calcineurin inhibitors, oral antihistamines, and phototherapy1. It is imperative to provide patients with reassurance regarding the benign yet chronic course of this condition. This case underscores the importance of considering LN in HIV-positive patients and highlights the utility of dermoscopy in its diagnosis. Clinicians encountering similar presentations should consider LN in their differential diagnosis.














