Introduction
We report the first two cases in the literature of patients who developed both erythema nodosum (EN) and Sweet syndrome (SS), following simultaneous vaccination against COVID-19 with the Comirnaty Bivalent BA. 1 vaccine (Pfizer) and influenza with the trivalent vaccine provided by the Brazilian Unified Health System.
Case report
Case 1: a 49-year-old healthy female presented with petechiae over an erythematous plaque on the digital pulps, a single painful erythematousedematous papule with a vesicle-like appearance on the left arm –at the site of one of the vaccines, an aphthous lesion on the jugal mucosa of the lower lip, and painful erythematous-violaceous nodules on the lower limbs (Fig. 1), which appeared simultaneously 2 weeks after COVID-19 and influenza vaccination. The condition was associated with a maximum fever of 38.3 °C. Laboratory studies showed no alterations; serologies for hepatitis and sexually transmitted infections were negative. Incisional biopsies were performed on the arm and the left leg, and the histopathology report confirmed SS and EN.
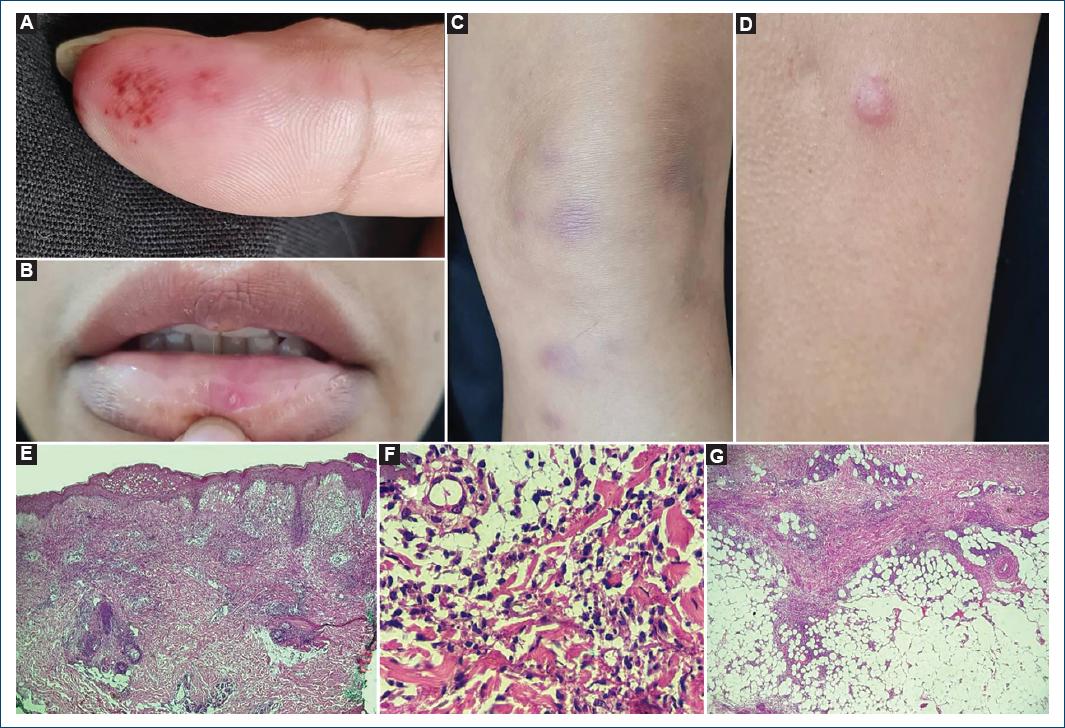
Figure 1 Patient 1 – petechiae over an erythematous plaque on the digital pulp of the first right finger (A), single aphthous lesion on the lower lip (B), erythematous-violaceous nodules on the lower limbs (C), and erythematous papules with hypochromic center and central pseudovesiculation located on the left arm (D). Histopathology from the arm with papillary dermal edema, perivascular and interstitial dermal infiltrate (H&E, 4×) (E), predominantly with neutrophils and leukocytoclasis (H&E, 40×) (F), and from the leg with septal panniculitis (H&E, 4×) (G).
Case 2: a 41-year-old healthy female presented with painful erythematous-edematous papules and plaques with a vesicle-like appearance on the upper limbs, as well as painful erythematous-violaceous nodules on the lower limbs (Fig. 2) that appeared 1 week after COVID-19 and influenza vaccination, associated with fever (max 38.3 °C) and arthralgia. The patient had no alterations in serologies and other blood tests, except an elevated ESR (38 mm/h) and protein electrophoresis with asymmetrical distribution of the γ fraction. Histopathology of one of the lesions on the forearm confirmed the hypothesis of SS. Lower limb lesions were clinically diagnosed as EN.
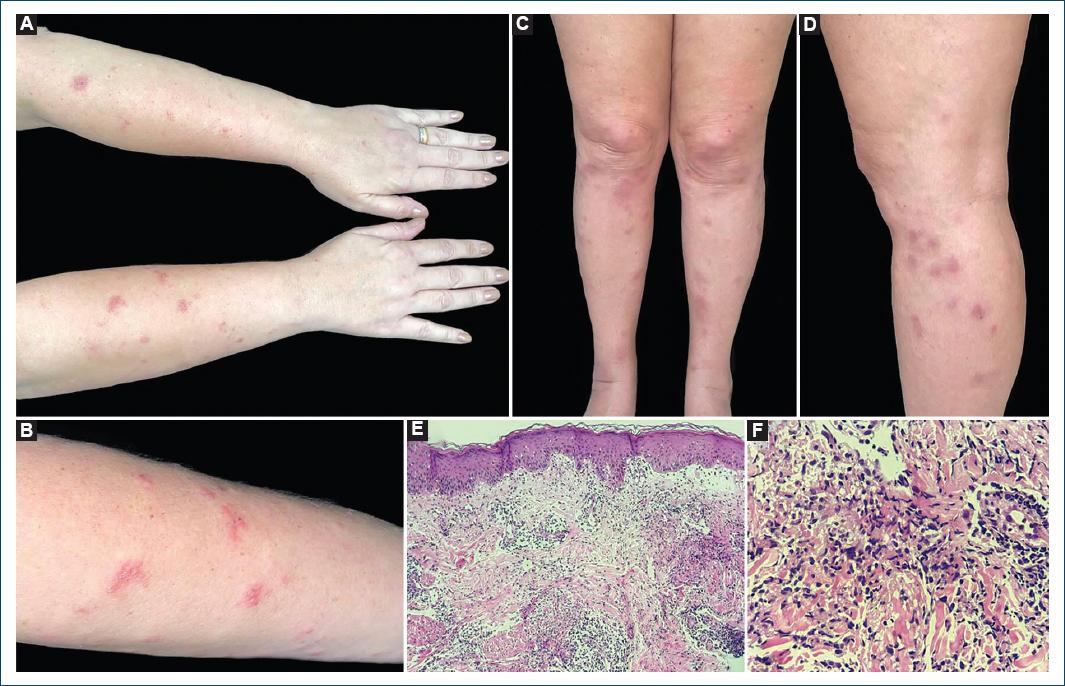
Figure 2 Patient 2 – erythematous papules and plaques with pseudovesiculation on the forearms (A), and left forearm (B), and erythematous-violaceous nodules on the lower limbs (C), and left leg (D). Histopathology from a lesion on the forearm showing focal papillary dermal edema and dermal infiltrate (H&E, 10×) (E) predominantly composed of neutrophils (H&E, 40×) (F).
Treatment with oral prednisone –at a dose of 40 mg/day for 7 days followed by gradual weaning until completing 21 days of treatment – was initiated in both cases, with complete resolution in 14 days and no recurrence.
Discussion
SS occurs predominantly in middle-aged women following an infectious condition. Vaccinations can also trigger the syndrome1, which can still be associated with inflammatory conditions such as EN1,2. Elevated erythematous plaques with vesicle-like appearance preferentially affect the face, neck, and extremities and may be accompanied by fever, general malaise, involvement of the eyes, joints, and oral mucosa1. It is associated with the pathergy phenomenon, with few reports in the literature, which may justify the appearance of a single lesion at the vaccine application site as shown in case 13.
The diagnosis includes the presence of two major criteria (abrupt onset of lesions and compatible histopathology –diffuse dermal and perivascular neutrophilic infiltrate, with leukocytoclasia and dermal edema) and at least two minor criteria (fever, constitutional symptoms, leukocytosis, good response to systemic corticotherapy, and presence of triggering factors such as medication, vaccination, neoplasm, pregnancy, and infectious/inflammatory diseases)1. Some authors also propose specific diagnostic criteria for the drug-induced form, requiring the presence of five criteria: abrupt appearance of typical cutaneous lesions, histopathology compatible with SS, presence of fever and constitutional signs and symptoms, temporal relationship between the onset of the medication and clinical manifestation or relapse after therapeutic testing with the drug, and temporal relationship between withdrawal of the medication or use of systemic corticosteroids and resolution of the condition4.
SS responds quickly to systemic corticotherapy, which is the first line of treatment1 –the therapeutic option adopted in the two cases reported. Laboratory tests can reveal leukocytosis with neutrophilia, elevated ESR, and transient IgA monoclonal gammopathy, which has also been described in the literature after Janssen’s Ad26.COV2.S vaccine3.
EN is characterized by the presence of symmetrical, painful erythematous nodules located mainly in the pretibial region5. Like SS, it is more common in adult women and has the same triggering factors, such as vaccinations5. The histopathology shows septal panniculitis with neutrophilic infiltrate in the acute phase and later an infiltrate with lymphocytes, histiocytes, and giant cells. Diagnosis is eminently clinical and treatment includes anti-inflammatory and symptomatic drugs5.
Postvaccination cutaneous reactions are rare and can occur in association with the vaccine or the adjuvant6. With the COVID-19 pandemic, recent articles have discussed the association between either SS or EN and vaccination against SARS-CoV23,6; however, the association of these disorders with vaccination is rare, with few case reports in the literature6–10. Until now, we found no case reporting the concomitance of both dermatoses after vaccination. Nevertheless, in the second case reported, we believe that two diseases, SS and EN, represent different manifestations of the same hypersensitivity reaction to the vaccine at two different body sites. However, in contrast to the first case, a biopsy of the cutaneous leg lesions was not performed and we cannot completely rule out the possibility of SS mimicking EM. Actually, some authors have described that SS can present on the legs with lesions that clinically resemble EN11,12.
We cannot infer whether the cases were due to the influenza vaccination, the COVID-19 vaccination, or a combination of both vaccines. However, as these are concomitant cases of the two dermatoses after simultaneous vaccination, something not yet reported in the literature, the communication of these cases is relevant in the current global health situation. However, it is important to note that nonserious adverse events from vaccination, such as these two, should not discourage people from getting vaccinated.














