THE EPIDEMIOLOGICAL BURDEN OF CHRONIC KIDNEY DISEASE
Chronic kidney disease (CKD) is associated with aging. In Portugal, the inversion of the age pyramid is obvious with a growing number of citizens older than 65 years (23.43%) according to data from Censos 2021.1 The improvement of socioeconomic and health care conditions promoted longevity. The growing number of CKD patients is explained by the increase of the average life expectancy in the general population, the increased survival of patients with cardiovascular and neoplastic pathology and the rise in the prevalence of risk factors like diabetes or arterial hypertension. In stage 5 CKD, also called end stage kidney disease (ESKD), the prevalence of patients on kidney replacement therapies (KRT) in our country is the highest of the European countries.2 According to the National Registry of Sociedade Portuguesa de Nefrologia,3 in 2021, 20 731 patients were under KRT in Portugal, which represents a prevalence of 2004 pmp. There is also an increase in the average age of patients who start dialysis aside by a high mortality in older patients. Six‑point seven percent of those deaths occurred within the first 90 days after starting dialysis.4
THE ECONOMIC BURDEN OF CHRONIC KIDNEY DISEASE
In Portugal, the Constitutional Law states that “everyone has the right to health protection and the duty to defend and promote it” and this “right to health protection is carried out through the National Health Service” (NHS).5 Based on this principle, the NHS was created, in 1979, as an “universal, generally and tending to be free” service that enables universal access to health care. Grounded on this assumption, all modalities used to treat ESKD (dialysis or transplantation) are totally insured by the NHS and available to all patients for whom they are feasible.
Facing the growing number of patients depending on KRT and its elevated costs, it is reasonable to conclude that CKD represents a heavy burden for the NHS. It is estimated that CKD is responsible for an expenditure of €140 billion per year, more than the annual health care costs for cancer or diabetes.6
Hemodialysis has been mostly supplied by private providers and it was paid by act for more than 25 years, until 2008.7
THE INDIVIDUAL BURDEN OF CHRONIC KIDNEY DISEASE
It is predicted that CKD might become the 5th leading cause of death worldwide by 2040.6 The expected years of life lost in dialysis depend on age but are around 10 years compared to the general population.8 In other words, the lifetime expectancy of an ESKD patient is inferior to most cancer patients.9 Besides mortality, CKD represents a high burden in disability adjusted life years (DALY). In our country, DALY are between 200 and 299 per 100 000 inhabitants, a value higher than most countries in the Western Europe and Canada.6
It is fair to state that, in general, treatment of ESKD with dialysis is associated with a significant patient survival ad‑ vantage. However, this advantage is dramatically reduced for older people (mostly above 75 years) with major comorbidities (mainly coronary artery disease), or poor functional status and it may be lost if we consider hospital free survival and health related quality of life (QoL).10‑13More than half (58%) ESKD patients living in a nursing home had died within their first year after dialysis initiation, 29% had a decrease in functional status and only 13% maintained it.14 According to another study, patients older than 85 showed a median survival after dialysis initiation below 6 months, with more than a third of that time spent in the hospital receiving the highest intensity of care.15‑20Quality of life and symptoms associated with CKD have also been subject of interest. Several studies have shown that the number and weight of these outcomes are similar in patients undergoing different modalities of KRT (regardless of age and comorbidities) and similar to terminal cancer patients.9 QoL may be difficult to evaluate since it is a very subjective outcome. Anyway, the incorporation of QoL assessment is also important to measure quality‑adjusted life years (QALY)21 and to compare cost effectiveness between different treatment options aiming to support financial sustainability focusing on quality and health gains.
CURRENT OVERVIEW OF END STAGE KIDNEY DISEASE TREATMENTS IN PORTUGAL
Currently, ESKD can be treated by one of three modalities: dialysis (hemodialysis or peritoneal dialysis) and kidney trans‑ plantation. In 2021, like in the previous years, 96% of patients who started a KRT were under dialysis.3 However, in older and frail patients all of the 3 options to treat ESKD may be more harmful than beneficial, which bumps with the bioethical principles of maleficence and beneficence. Besides that, given the economic burden of these therapies, if no benefit is provided and resources are limited, offering KRT to older and frail patients may impact justice. This brought the need to explore new options to deal with ESKD.
EMERGING OPTIONS TO CHALLENGING PATHOLOGIES ‑ CONSERVATIVE CARE IN CKD
The social, economic and individual impact of CKD has been undervalued in detriment to other chronic diseases, but the information presented above suggested the need to find other options to treat a challenging disease: an innovative and person‑centered solution. Palliative Care (PC) has emerged as an option to avoid futile and costly treatments that might not benefit some patients and focus care on a patient‑centered perspective instead of a disease‑centered one. The World Health Organization (WHO) has clearly stat‑ ed that the provision of PC is a moral responsibility of the health care systems and an ethical duty of health professionals to relieve pain and suffering (physical, psychosocial, or spiritual) regardless of whether the disease or condition can be cured or just handled, like CKD.22 In the last 20 years, evidence on the use of PC in Nephrology has been published to found its use in all CKD patients. Because of the prejudice associated with the term “Palliative Care”, the principles of Palliative Medicine have been denominated as Supportive, Conservative and/or Comprehensive Care when applied to CKD patients. The integration of PC in the management of these patients makes part of a continuum of an integrated care to all phases of the disease.23 It means that whenever the patient status declines, appropriate escalation of supportive/palliative care should be offered. So, it should be considered for all patients approaching ESKD (both the ones who choose not to be submitted to any kind of KRT and or those who have no conditions to proceed to it) as well as those already on KRT.
Offering dialysis to patients who do not benefit from it, like the more than 6% who die in the first 90 days after starting dialysis,3represents a high cost of care but not a patient‑centered one. Many of these patients receive high‑cost, high‑intensity care near the end of life that only contributes to suffering and uncontrolled symptoms. Patients with ESKD receive more intensive treatment than patients with heart failure or cancer but have less access to PC.24,25Most ESKD patients (69%) die as hospital inpatients, where they are repeatedly admitted without having never discussed an advance care plan or the possibility to access a palliative service.26 Unfortunately, most patients and their families have not been involved in the decision process about the kind of care they want to receive at the end of life. It is quite common to hear patients regretting having ever initiated dialysis or doing it to please their doctors or their family.27 There is a wealth of literature demonstrating that patients and/or their families desire to receive accurate prognostic information and to be involved in the planning of their care. Elderly patients on hemodialysis report that their entire day is often taken up traveling to and from the dialysis unit and undergoing the treatment itself. Not offering the option of being cared without dialysis (meaning being cared in a Conservative Care program) is, therefore, a definite downgrading of the quality of care provided by nephrologists with a high cost to the NHS and, sometimes, not aligned with the patient’s preferences and values.
Still, in what PC concerns, ESKD patients can receive hospice care only if:
they have advanced CKD, are expected to die within 1 month and agree to forgo dialysis;
their terminal illness is ESKD and they withdraw from dialysis;
their terminal illness is ESKD and a hospice program agrees to accept them on dialysis care for the caregiver rest; or
they have a terminal illness unrelated to ESKD which allows them to receive concurrent hospice for oncologic uncontrolled symptoms and dialysis care.
This means that ESKD patients only access PC in the final few days of life, a time frame generally considered insufficient to optimize end‑of‑life care.28,29A universal screen for PC needs is, therefore, essential to provide a more qualified care, to satisfy patients and families or caregivers and is also a measure to guarantee the sustainability of the NHS.
In Portugal, in 2011, Direção Geral de Saúde (DGS) published “Norma 17”, a clinical guideline that recommended the implementation of “Conservative Medical Treatment” to handle some CKD stage 5 patients (those who choose not to be submitted to any kind of KRT or those who have no conditions to proceed to it).30
“Norma 17” establishes the conditions that must be checked to monitor patients who opt for Conservative Care or those who have no conditions to pursue a KRT. Despite its publication more than 10 years ago, this norm has never been audited and the legislation was not updated in order to frame this option as an effective alternative. Even if it is rated in the same level as all other treatment modalities, a differentiated payment, similarly to what happens in kidney transplantation (with its own legislation) or in dialysis (with a payment model), was not stablished.
There are no official numbers on patients who were treated by Conservative Care because, contrary to what happens in other KRT, there are no records from the Health Ministry to account for these patients. All patients on dialysis are inserted on a platform, called Gestão Integrada da Doença (GID), created to register these patients. For CKD stage 5 patients who do not pursuit an invasive pathway there is no accountability, although they might be a residual number. There are several factors that might explain that. One is the lack of training in PC by nephrologists. It is easier to do the most familiar way of treatment, in this case hemodialysis.31 Another factor for the low number of patients in Conservative Care is refund. It is also more profitable to start a patient on dialysis than to manage the same patient with advanced CKD in an interdisciplinary PC program if refund for Conservative Care is not guaranteed. A European Survey showed that the occurrence of dialysis withdrawal almost doubled when PC was reimbursed, suggesting that clinicians are willing to proceed with dialysis withdrawal when appropriate conservative care is provided.32,33It must be assured an equal access to medical care and reimbursement for patients undergoing dialysis, conservative care or for whom dialysis has been suspended, as suggested by the “International Society of Nephrology that “incorporated Conservative Kidney Management in the Strategic Plan for Integrated Care of Patients with kidney failure for the next 5‑10 years.”34 or by the American Society of Nephrology that stated that “Incorporating Conservative kidney management into routine nephrology practice can assist in overcoming potential barriers for dialysis withdrawal.”10,35
This means that when reimbursement is not granted, implementation is not effective. Therefore, it is urgent to carry out an economic assessment of the implementation of the Conservative Care option in Nephrology Units. That is the only way for this modality to be in similar conditions to be adopted as other current approaches to ESKD.
In other words, national policies can affect the decision‑making process: lack of parity in reimbursement for conservative care programs compared to dialysis care disincentives PC. Additional policy measures that could sup‑ port the provision of PC would be legislation addressing reimbursement for advance care planning, telemedicine for home‑based primary care and PC training.36
MODELS OF CONSERVATIVE CARE IN CHRONIC KIDNEY DISEASE
Conservative Care has been defined as an “Holistic approach, patient‑centered, to treat ESKD patients who choose not to be submitted to any kind of KRT or who have no conditions to proceed to it, aiming to delay further deterioration of renal function, preventing and relieving symptoms and adverse events resulting from irreversible progression of renal disease.”35 Since this integrated care is no longer seen as synonymous of “giving up” or “care for dying patients”, the best PC ideally begins as early as possible in the course of the disease and continues in parallel with renal disease‑focused therapy in a multidisciplinary team.37,38Although the timing has been consensual, there are several proposed models to implement a Conservative Care Program39,40:
Nephrologists with at least intermediate education provide palliative interventions in the Nephrology Unit and refer complex cases to Palliative Care teams;
Patients who benefit from palliative approaches are referred to and followed by to Palliative Care teams (in parallel with the Nephrological Care);
Nephrology Units have Palliative Physicians as part of their team who consult patients who benefit from palliative approaches.
To the best of our knowledge, there are no studies that prove the superiority of a model over another and basically it will depend a lot on each setting and context. In Portugal, where Palliative Medicine is not individualized as an autonomous specialty and where human resources are scarce, the authors defend the first model.41 This model presents several advantages such as:
it promotes the continuum of care (patients maintain the follow up in the same Unit, ideally with the same doctor, where patients have been followed, in some cases, for years);
nephrologists keep managing the CKD complications and the specificities of prescription in patients with renal dysfunction;
In hemodialysis units, patients are already followed 3 times a week by multidisciplinary teams (physicians, nurses, social workers, psychologists, pharmacists and dietitians), improving resources utilization.
In what concerns to settings where Conservative Care should be provided (private versus public), there are no economic studies to evaluate it. It depends on the reality of each national health system politics (based on public or private providers). In our opinion, in Portugal, patients who have never been on dialysis (patients who opt for conservative care or who have no conditions to KRT) should continue to be followed in the hospital where their nephrology care in being provided. Patients who are attending private dialysis clinics would ideally be followed in these institutions by professionals with PC education, in parallel with their attending nephrologists. That would be a way of the patients not to feel abandoned in their last days of life and not having to meet a knew team to whom they are unknown. Anyway, and once more, private units will only offer services for which they are paid for, which is not the case. That is one other example of the importance of establishing an economic evaluation of the several options and implementing a reimbursement strategy for this kind of care.
REQUIREMENTS FOR A CONSERVATIVE CARE PROGRAM IMPLEMENTATION
Unlike dialysis or kidney transplantation, a Conservative Care Program requires very few resources.
Human Resources
The cornerstone of a Conservative Care Program is a Nephrologist with intermediate or advanced education on PC. This subject is not yet a requirement of the Portuguese nephrology curriculum, but in the last years many nephrologists and residents have undertaken education in PC at their own expenses. Furthermore, in 2021, the Portuguese Parliament approved a resolution (131/2021, April 29, 2021) recommending formal training at an intermediate level in PC for nephrologists (among other specialties). Nephrologists should take the lead of the multidisciplinary team. They should coordinate care with other doctors, including the primary care physician, the palliative care doctor and other colleagues who also follow the patient.
The multidisciplinary team should include other professionals with at least basic education in PC: nurses, nutritionists, psychologists, and social workers. These members may be shared with other units within the nephrology department (dialysis, transplantation), so it does not require any new acquisition. The time spent by these human resources in the Conservative Care Program will depend on the number of patients followed, but it will always be much less than the needs from other KRT, particularly hemodialysis.
In what concerts to articulation protocols, it is important to settle short cuts to the hospital and community (when available) PC teams. Anyway, the referral criteria are no different from any other sources, including to apply to hospice beds (out of the scope of this article).
Logistical Resources
For logistics, all that is required is a consultation office which is significantly different (and cheaper) than any other KRT.
The pathway until a patient has indication to be followed in this appointment is the same as in other KRT: after informed decision‑making regarding ESKD treatment modalities, the patient follows the way as defined in Norma 17.
Anyway, there are several rights that are assured to all KRT patients that are not provided to Conservative Care patients:
Access to medication. There are several drugs that are freely supplied patients on KRT that should also be guaranteed to palliative patients. Additionally, some drugs specific to PC, like opioids for pain or dyspnea, should be provided in the same way that immunosuppressors are assured to transplanted patients;
Transports. As for any other ESKD patient (artigo 4º da Portaria n. º 142‑B/2012), the NHS has to ensure the costs of transportation, for all acts related to the conservative care consultation. Transports are also totally free of charge for patients in PC consultations.
Exemption from user fees and inability certification. These patients must have the same rights as the declaration of a > 60% inability certification to effects of exemption, independently of their socio‑economic status.36 Also in this point, PC consultations are exempted from user fees.
BROAD ANALYSIS OF END STAGE KIDNEY DISEASE TREATMENTS PAYMENT AND REIMBURSEMENT
Health care policies in ESKD treatments have evolved over time to reach two goals:
restraining spending growth;
providing the best care through meeting innovation and quality standards.
To accomplish these goals, the Portuguese NHS changed its payment policy and renewed the delivery models. The high costs associated with dialysis treatments and the dependency of the NHS on the private providers led to a change in the financial management of these health care services. In 2008, an integrated management model for ESKD was developed. This initiative restructured the delivery of dialysis services, the monitoring of outcomes and the funding of dialysis. This model integrated various dialysis services and products, which were reimbursed at a fixed rate/patient/week called preço compreensivo (“comprehensive price”). This value‑based purchasing model consists of a prospective bundled payment to dialysis facilities for outpatient dialysis services and a set of pay‑for‑indicators initiatives. Included in this bundled price are the provision of dialysis, the billable medication, laboratory tests, some imaging and cardiology exams and the vascular access management. The payment amount is now (year 2023) established in €450.68 (€64.383/patient/ day) to providers who choose not to include vascular accesses and €470.09 (€67.156/patient/day) to those who do (Despacho nº 10569/2011). This model seemed to represent a win‑win strategy for payers, providers and patients. However, the real‑world data exposed some limitations of this model, namely:
The access to innovation is expensive and might be refused because it is not supported by the accorded budget;
The contracted indicators / outcomes (number of dialysis sessions, laboratory results…) do not attend individual patient needs. The blind pursuit for a “high value care” that means applying uniform standards of care to all patients irrespective of their specificities may harm more than guarantee the good legis artis. For example, a 4‑hour dialysis plan to reach good dialysis adequacy in a young man with 100 kg must be necessarily different from the needs of an 85 years‑old woman with 47 kg. The same is true when we analyze hemoglobin or phosphorus levels, or any other parameters that compose the standard that has been stated.
That is why PC in Nephrology is an innovative and quality‑driven approach that benefits both patients and the NHS, contributing towards the rationalization of service provision and the efficient use of resources.
CONSERVATIVE CARE COST‑EFFECTIVENESS ANALYSIS AND LIMITATIONS OF THE USUAL MODELS
Cost ‑effectiveness analysis is a method of comparing costs and effects of two or more alternatives in health or social care interventions to an outcome. Conceptual models of cost‑effectiveness analysis evaluate outcomes compared to costs (Fig. 1). Cost‑saving interventions are only beneficial if they bring the same outcome.
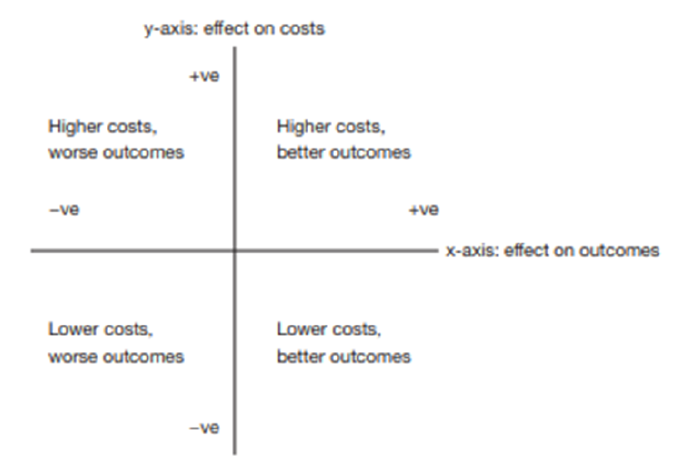
Adapted from: May P, et al. Economic outcomes in palliative and end‑of‑life care: Current state of affairs. Ann Cardiothorac Surg. 2018;7:S244-8.42
Figure 1. Conceptual Illustration of cost‑effectiveness analysis
The way costs and outcomes are measured are, therefore, crucial. Quality‑adjusted life‑years (QALYs) is a popular measure of outcome to evaluate cost‑effectiveness in health care. It provides a metric for valuing a healthcare intervention on survival (quantity) and health‑related QoL. That is the first difficulty in using this indicator: if we are dealing with old and frail patients, survival is compromised by all the conditions presented (ESKD, comorbidities, age and frailty). Secondly QoL is difficult to measure since it is subjective. There are validated tools (e.g. EQ‑5D) that allow its evaluation and comparison between interventions, but its application in Nephrology is recent and data comparing QoL in KRT and Conservative Care is limited. Furthermore, studies rely on observation since it would be unethical to perform randomized control trials to compare outcomes or costs on both pathways (KRT versus Conservative Care). On the other hand, only recently have patient‑reported outcomes (PRO) started to be used to evaluate interventions, so they are still not used in economic theory. Another limitation is the fact that patients who are feasible to Conservative Care may be too old, too frail or too ill to express QoL, which would make QALYs not adequate to evaluate these patients. Finally, end of life is unique and personal. The experience of a “good death” is not measurable.
In regards to cost evaluation there are also limitations. Costs of care are mostly elevated at the end of life,42 but the way they are calculated is debatable. Cost evaluation comes mainly from studies in hospitals and/or is obtained by healthcare utilization in context of rapidly progressing diseases such as cancer. This is not extrapolable to ESKD that has a different disease trajectory, especially if patients are under KRT or if they present other comorbidities like increasing frailty over many months or years.
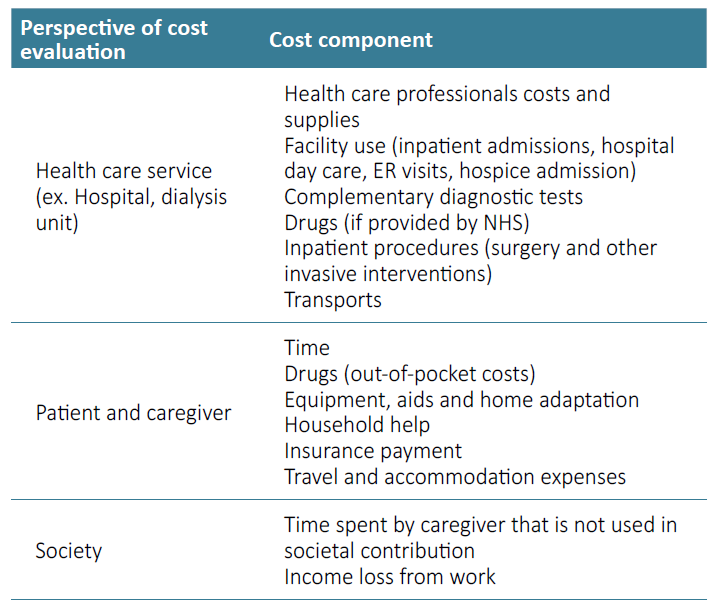
The way we evaluate costs might have different points of view. It may be analyzed from the provider’s angle. In this case, costs are mainly synonyms of what it is charged, which is different from what it really costs. It does not take into account indirect costs such as caregiver or out‑of‑pocket ones or gains in QoL. These costs are the ones that come from the patient’s point of view, but which are rarely evaluated in economic studies. Finally, there is a societal point of view to handle (Table 1). Most of these patients are old and ill, so they do not work but they require a care‑giver that, most of the time, has to abandon his job to take care of the sick one. Furthermore, PC might be a service that is offered to patients in need besides disease specific therapy (chemotherapy, dialysis, …). This might increase costs but also improve QoL.
Finally, costs are not extrapolable from other realities since they depend on several conditions. First, the national setting (different national health systems and societal values) in which the clinical interventions and outcomes are defined and measured. Second, the time to evaluate the disease trajectory is incredibly different from one patient to the other. Third, the heterogeneity of interventions and way of delivery is so distinct (different populations with different ages, diagnosis and prognosis) and the approaches that fall under the “palliative care” label are so diversified that it is really difficult to build a model that fits all conditions. Whenever a care or intervention is a patient centered one instead of a standardized one (like what happens in dialysis with its performance parameters that are the same for all patients) it will always be difficult to evaluate. Anyway, current evidence on the economic outcomes from PC interventions are generally cost saving43 and that is certainly the belief of the authors from their experience in the field. Recently, an article has been published that performs a cost‑utility analysis comparing hemodialysis and conservative care using two instruments to assess healthcare interventions in CKD patients. They conclude that conservative care “proves a preferable and more cost‑effective treatment option than HD for CKD patients aged 65 and above, regardless of the quality‑of‑life measure used for QALY calculations”.44
OUTCOMES THAT MIGHT BE USED TO AUDIT CONSERVATIVE CARE
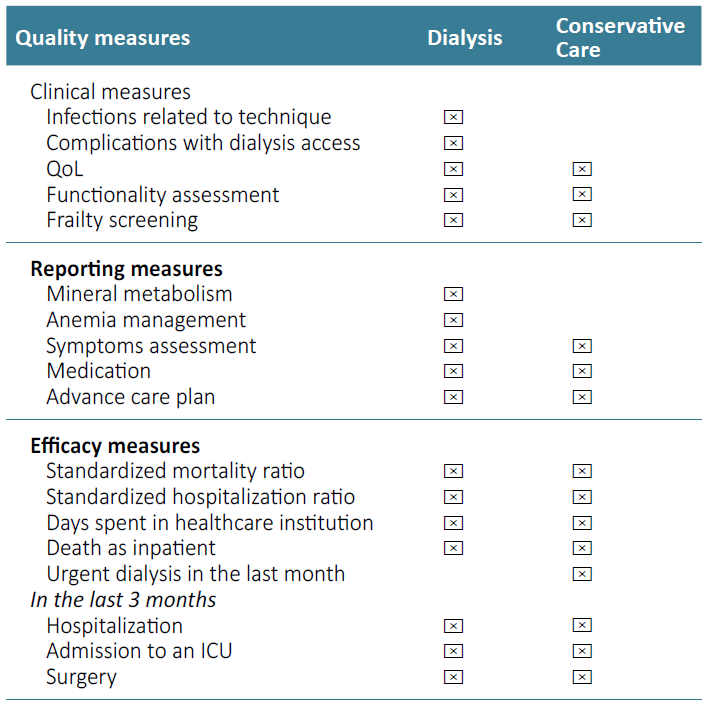
Even when measurement is challenging, policy makers still need evidence to make decisions. In a patient centered care instead of a disease centered one, outcomes suggested to audit value‑based services would be, naturally, different. Dialysis indicators are focused on tangible measures like adequacy of dialysis, anemia or mineral metabolism management. In conservative care, reimbursement must focus on patient‑reported outcomes, such as symptoms and QoL, as well as detailed communication around prognosis, shared decision making, advance care planning, and ensuring that treatments remain aligned with patient preferences and prognosis. Anyway, some indicators and outcomes should be shared in all KRT, such as hospital admission, days spent at home and symptom control. Advance care plans should also be an indicator of value for money. That would include the percentage of patients who have a stated living will (with suitable invasive interventions and Do Not Resuscitate order) and indication of place of death.
The scarce literature on indicators of cost‑effectiveness to evaluate Conservative Care reflect the novelty (namely in Portugal) of this CKD approach and the real‑world challenges in the measurement of abstract outcomes such as satisfaction with care among an old and frail population. Nevertheless, it is time to identify relevant components to truly evaluate the individual, clinical and economic impact of this modality (Table 2).
CONCLUSION
The objectives of health policies should be to guarantee access to the health care, with quality, effectiveness, efficiency, and safety in the provision of services in a universal coverage, but at the same time to assure financial sustain‑ ability and patients’ satisfaction. The continuum of care in CKD seems to respond to all of these objectives. For nephrologists it does not persist any doubt that Conservative Care should be part of ESKD care and the choice for this pathway is based on its clinical benefit for the patient. Nevertheless, healthcare decision makers should also reflect about Conservative Care and have a plan to support this modality based on its value for the money. To turn this option in a reality, a cost‑effectiveness evaluation must be implemented.