INTRODUCTION
Ageing is a complex and heterogeneous process. Some elderly patients remain independent and fit while others show significant frailty. Patients with chronic kidney disease (CKD) are at a higher risk of becoming frail. This is associated with worse outcomes.1 Patients with CKD also have a high burden of physical and psychological symptoms (a consequence of high comorbidities and worse functional status) with a negative impact on their quality of life and higher mortality.1,2
In such patients, symptom burden and frailty do not necessarily improve with the initiation of dialysis, nor do quality of life or survival.3 Conservative care offers an alternative focused on quality of life.4
In 2013 the KDIGO conference on Controversies on Supportive Care in Chronic Kidney Disease proposed the main principles and competencies of conservative care:
Conservative care has been recognized in Portugal as an option to CKD patients since 2011. A guideline named “Tratamento Conservador Médico da Insuficiência Renal Crónica Estádio 5 - Norma 017/2011” was published by Direção Geral de Saúde (the Portuguese General Directorate of Health) highlighting the general principles and patients who might benefit from conservative care. Unfortunately, it was not followed by a reimbursement policy or a specific framework on how to implement it.7 It has been 12 years since “Norma 17” was published and, while conservative care is now widely accepted among nephrologists, its delivery varies according to the resources available to each program. In some Nephrology Departments, structured conservative care programs do not exist.8
The Conservative Care Working Group (CC WG) of the Portuguese Society of Nephrology (Sociedade Portuguesa de Nefrologia) set out to identify barriers to the implementation of Conservative Care Programs and to find solutions. To do so, a questionnaire was sent to all Nephrology departments and an open meeting was organized, whose results we report in this paper.
METHODS
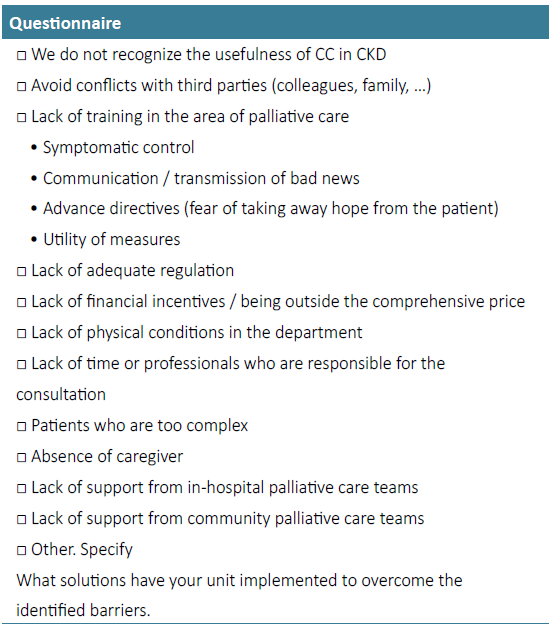
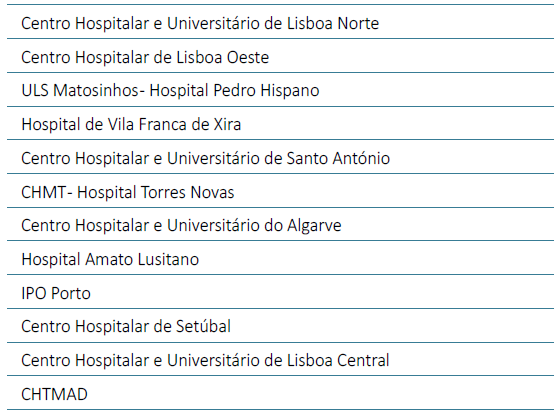
An original, multi select, multiple choice questionnaire (with some open answer items) was designed by the CC WG and sent to all Nephrology departments in Portugal (Table 1). The answers were collected and analyzed by the principal investigator. The results were presented during a virtual meeting, open to all participating departments, (Table 2) where people were invited to share their realities and think of solutions.
RESULTS
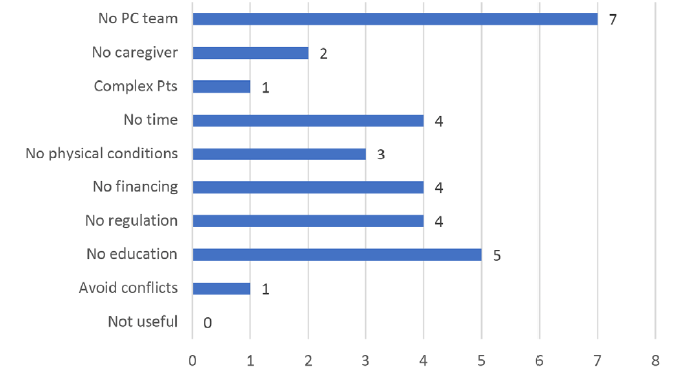
Twenty‑six departments were contacted. From those, 15 (58%) replied (Table 2). Fig. 1 shows the main barriers to the implementation of conservative care programs, namely “lack of palliative care teams” (n=7, 47%) and “lack of knowledge from nephrologists in this field” (n=5, 33%). Also relevant was the “lack of financing” and the “lack of regulation” (both with n=4, 27%). Logistical difficulties were also mentioned, namely lack of time (n=4, 27%) and lack of infrastructures (n=3, 20%). No unit mentioned the lack of importance of CC programs.
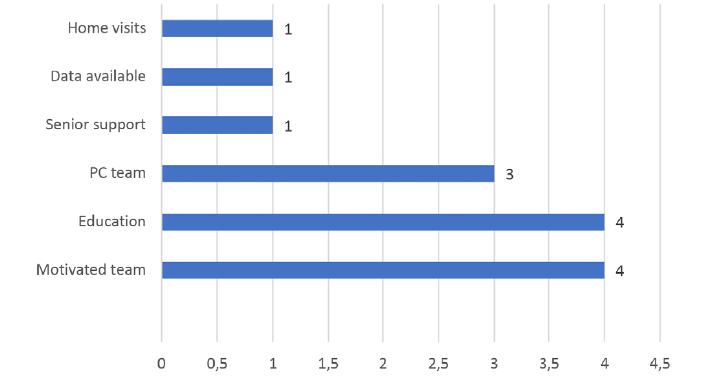
Fig. 2 shows the solutions that were proposed, the most important being having a motivated team (n=4, 27%) and having education in palliative care (n=4, 27%). Having a link to a supporting palliative care team was also mentioned.
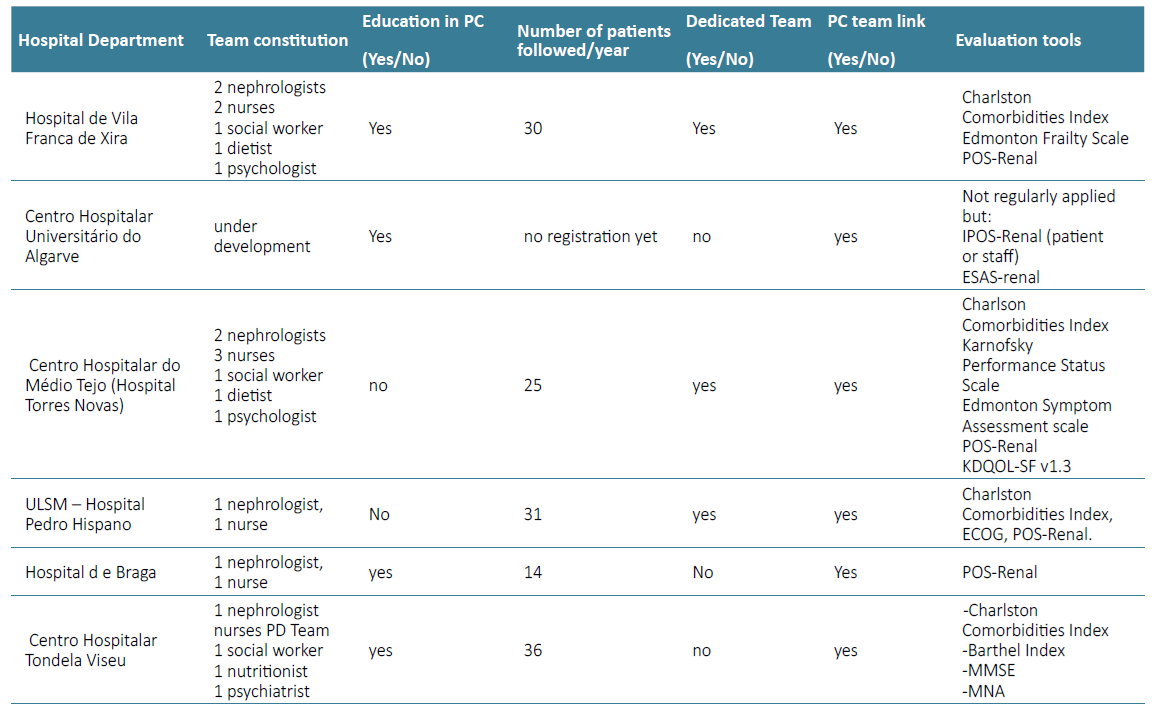
Table 3 contains the main characteristic of the participating programs (n=6). The majority (n=4, 66%) have professionals with intermediate to advanced education in palliative care even if the team is not dedicated mainly to conservative care (n=3, 50%). All programs have simultaneous doctor and nurse patient assessment. How other professionals participate (nutritionist, social worker, psychologist) varies between programs.
All teams are linked to either a hospital or community palliative care support team. The mean number of patients per program was approximately 30 patients. All units used symptom assessment scales (iPOS‑R or ESAs). Most units used a comorbidity scale (Charlson Comorbidities Index) and a functional scale (Karnofski, Barthel or ECOG). Some units use Quality of life scales, frailty scales or cognitive assessment.
DISCUSSION
We identified insufficient education in palliative care as the main obstacle to the implementation of conservative care programs. This is most likely because palliative care is not part of the Nephrology Residency program. This is in line with the barriers identified in other countries, even in countries with a longer tradition in palliative care, such as the United Kingdom and the Netherlands.9‑12Difficulty accessing a supporting Palliative Care team can worsen this problem.13 The solution to the first barrier involves the Colégio de Nefrologia da Ordem dos Médicos updating the residency program to include palliative care, which we have proposed.14 The second issue involves the Health Ministry accelerating the development of the Palliative Care Network, but this will take time. In the meantime, we encourage more flexibility and direct communication between the conservative care team and health care providers in primary care, nursing homes, home care facilities, etc.
The second most cited barrier is “lack of regulation and/ or reimbursement”. “Norma 17” set the general principles of conservative care but reimbursement was never established. Hemodialysis and peritoneal dialysis are funded through a system of bundled payments which has been important for the allocation of resources and standardization of care.15 No such system was ever established for conservative care in Portugal. This a barrier in other countries as well.16 The solution to this involves the continuing appeals of groups such as Comissão Nacional de Acompanhamento dos Doentes em Diálise (CNAD) or Sociedade Portuguesa de Nefrologia for the Health Ministry to create a reimbursement policy. Recently, a national plan for CKD care was published (Despacho nº12635/2023 de 11 de dezembro) which includes references to the need to implement a conservative care circuit for patients, and integrated dialysis/CC programs, but no specifics on how to do it are given.
Some units mentioned having limited resources. Conservative care is the modality of stage 5 CKD management that requires fewer resources: we estimate that a nephrologist is not expected to spend more than 10 hours per week in a program with 30 patients and about the same for a nurse.16 Human and physical resources may be shared with other sections of the Nephrology department.
Other issues such as the complexity of patients or the absence of a caregiver are shared with other kidney replacement therapies and should not dissuade the implementation of a program. A diligent multidisciplinary team can predict these problems and often find solutions.
Finally, the importance of avoiding conflicts with families and colleagues was mentioned. Again, training in communication, which is a fundamental part of palliative care, can be helpful here. The importance of having the support of the Head of the Nephrology department is, likewise, critical. Although not a single unit answered that conservative care was not useful, we can not discard a possible representation bias. Our study has some limitations. It is based on an original unvalidated questionnaire. Some barriers and solutions may not have been considered. It was sent by email. A significant number of departments did not reply. Some departments did not disclose the characteristics of their programs. Nonetheless, this is the first and only study to address the state of the art of conservative care in Portugal.
CONCLUSION
Although some important barriers have been identified by all Nephrology departments, some units have found ways to overcome them, and are offering patient‑centered conservative care to elderly or frail CKD patients who so chose. We hope this paper can inform and inspire all departments to overcome their barriers to the implementation of their own conservative care programs.