INTRODUCTION
Patients with end‑stage renal disease (ESRD) have a high morbidity and mortality when compared to age‑matched individuals in the general population, and even with patients with other chronic diseases such as cancer and cardiovascular disease.1-3The treatment for ESRD may involve kidney replacement therapies (KRT) such as chronic dialysis (peritoneal dialysis or hemodialysis) or kidney transplant. Nevertheless, older patients with ESRD who frequently have other chronic health issues may not experience improved functional status or extended life expectancy with renal replacement therapies.4 Some of these patients are not candidates for kidney transplantation and others may face technical difficulties, as well as a high burden of symptoms when starting dialysis. Therefore, the decision to start dialysis or not can cause psychologic distress to the patient and family members. Individuals undergoing dialysis tend to receive more in‑ tensive medical care towards the end of their lives, which often includes hospital admissions, treatment in intensive care units, and invasive life‑support measures.2 It is important to note that patients already on dialysis have a threefold greater risk of experience cognitive impairment compared to age‑matched individuals,5 which can compromise their decisions when faced with the need to make choices about their health. However, despite these facts, numerous individuals fail to engage in discussions with their loved ones or healthcare providers regarding end‑of‑life matters such as their preferences concerning involvement with palliative care services, intensive care admission, discontinuation of renal replacement therapy, resuscitation measures, or their preferred place for passing.6 In a situation where the patient is incapacitated, this type of decision often has to be made by the surrogate, which is a difficult and stressful situation, especially when the patient’s wishes were not discussed. Thus, advance care planning (ACP) emerges as a valuable strategy to encourage collaborative decision‑making about the management of future healthcare conditions involving patients, their families, and healthcare providers, through conversations that aim to identify the patient’s values, preferences, and goals.7 Patients can record their preferences for future healthcare in advance directives (ADs), which are legal documents that can be consulted by healthcare professionals.
This article intends to review the topic of ACP in patients with ESRD worldwide and report the current situation in Portugal.
ADVANCE CARE PLANNING IN PATIENTS WITH ESRD
ACP is recommended for patients with ESRD,8 and the planning must be done before initiation of dialysis and adjusted as clinical circumstances change. Pre‑dialysis programs, where different KRT are explained to the patients with chronic kidney disease (CKD) stages 4 or 5, are appropriate moments for discussion about ACP.9 However, it is important to note that the most appropriate moment may need to be adapted to the patient and socio‑economic context that we are dealing with.
Patients undergoing dialysis therapy should include details about their dialysis treatment preferences in their ADs, ensuring clear guidance on how they wish their dialysis to be managed towards the end‑of‑life. This will enable to honor the patients’ values, as well as reduce the challenges associated with decision‑making by their surrogates.7 In the general population, ACP seems to be associated with significant advantages, such as enhanced quality of life, decreased stress and depression in family members, fewer hospital admissions, higher utilization of hospice and palliative care services, and healthcare aligned with patient preferences.10 Regarding dialysis population, ACP has been shown to improve surrogate grief11 and increase admission to palliative care.12 However, it is estimated that only 6%‑49% of the population with CKD has performed ACP worldwide.7,13-16
Feely MA and co‑authors in a retrospective study involving 808 ESRD patients on maintenance hemodialysis on dialysis units at Mayo Clinic in Rochester, found that 49% of patients had ADs in their electronic clinical records, but only 3% of their ADs addressed how they would like to manage dialysis at the end‑of‑life.7 It is noteworthy that patients articulate their preferences concerning other forms of organ support but often fail to specify their wishes regarding the ongoing organ support measures they are already receiving chronically. In the same study,7 the investigators also found that patients who had ADs tended to be older (74.5 vs 65.4 years old, p<0.001), more likely to be of white ethnicity (93.1% vs 80.1%, p<0.001), and more likely to be deceased (64.4% vs 46.6%, p<0.001) compared to those without ADs. Furthermore, patients with ADs also tended to have more comorbidities, such as dementia, coronary artery disease, congestive heart failure, and stroke. Additionally, a higher proportion of patients with ADs received palliative care consultations compared to those without ADs (20.2% vs 13.3%). The findings of the study carried out by this group of researchers seem to demonstrate that older patients with more comorbidities appear to have a greater awareness of their fragility, poor prognosis and limited longevity. On the other hand, the authors point out as a complementary justification for these results that these patients may simply have had more contact with healthcare and been more encouraged to undergo ACP.
In a prospective cohort study, involving 2575 kidney transplant (KT) candidates and 1233 KT recipients, Fisher MC et al,17 described that 21.4% of KT candidates and 34.9% of recipients engaged in ACP. The percentage of patients engaging ACP in this study is lower compared to other research involving dialysis patients.7,16 The authors explained this discrepancy by noting that their study included recipients and individuals eligible for KT, who might have better health status compared to participants in prior studies. However, it is important to recognize that numerous KT candidates and recipients endure lengthy periods undergoing dialysis, alongside significant comorbidities and frailty. Frequently, both patients and healthcare providers prioritize treatment goals and targets, overlooking the crucial discussion regarding ACP and patient preferences in situations of end‑of‑life and irreversible health conditions. In a retrospective cohort study Wang YH et al,18 found that ESRD patients were less likely to have ADs, compared to patients who had cancer. These findings seem to corroborate the idea that patients with ESKD often do not recognize their shorter life expectancy compared do general population.
Some studies in the United States7,17,19have reported racial disparities in relation to the likelihood of engage ACP. The probability of having ADs appears to be more frequent in white ethnicity. These disparities can be attributed to educational, cultural and religious differences. All of these issues are important to take into account when approaching the patient to discuss ACP.
To understand the concept of ACP it is essential not only for patients but also for healthcare professionals as they must be prepared to initiate and engage in discussions about it. Gomes BMM et al20 carried out a study in Minas Gerais, Brazil, in which they questioned medical students, doctors teaching at medical schools and companions of geriatric patients evaluated in an outpatient clinic. The researchers found that 77% of the doctors interviewed admitted they were unfamiliar with ADs. This underscores the importance of not only governmental efforts but also the inclusion of ACP discussions in medical conferences and medical schools’ programs.
In a systematic review, O’Halloran P et al21 pointed out as barriers to ACP the lack of training of the professionals, administrative complexities, pressures of routine care and lack of time, patients overestimating life expectancy, and when patients, family, and/or clinical staff are reluctant to initiate discussions.
Another crucial aspect to consider when discussing ACP with patients is to assure them that their decisions and preferences are not fixed and can be altered at any point.
In a study led by Cogo SB et al,22 it was found that while some patients expressed a desire to create ADs, they also harbored concerns about their effectiveness, fearing that their wishes might not be honored or could change when confronted with the realities of a terminal illness. Additionally, they expressed worries about being abandoned by healthcare professionals and uncertainty regarding the accuracy of diagnoses and prognoses. It is critical to tackle and clarify these concerns, and healthcare professionals need to undergo communication training to effectively accomplish this.
LIVING WILL - THE PORTUGUESE REALITY
In Portugal, in 2012, was approved a law which established the ADs regime, in the form of a living will (LW) and created the “Registo Nacional de Testamentos Vitais” (RENTEV): “Lei n.º 25/2012, de 16 de julho”.23 According to this law, the LW is a document that is unilateral and can be freely changed by the individual at any time. It can be created by a legally competent adult who is in a situation of mental lucidity and total decision ‑making autonomy. In the LW, the individuals express their informed and conscious preferences regarding the healthcare that they desire or refuse to receive in the event of they are unable to communicate their wishes personally and independently for any reason. This concept assumes that the patient has the right to refuse treatments that do not cure or alleviate symptoms, but only prolong life and suffering.24 In the Portuguese LW model (available in https://spms.minsaude.pt/wp‑content/uploads/2016/05/Rentev_form_v0.5.pdf), some of the treatments that are listed are cardiopulmonary resuscitation, invasive methods of artificial support of vital functions, artificial diet, medications, intravenous fluids, among others. The document, once validated, is effective for 5 years. In addition to the LW, a legal representative called a healthcare proxy can be nominated. It is worth noting that a LW does not have to be registered with RENTEV to be considered valid, a document authenticated by a notary also has legal validity.
Until this date, there is no national study in Portugal that evaluates the prevalence of ADs in patients with ESRD. However, Farinha A et al, in a cohort study that included 1265 patients from 6 hemodialysis units in Portugal, found that among the 158 patients who died during the year of follow‑up, only 2 patients had ADs.25 In the same cohort study, the authors verified that among the patients who died, only 10.8% had palliative care intervention (most commonly due to oncologic disease) and for more than a half of patients, nephrologists would not be surprised if they died in the next 6 months.25These findings indicate a low prevalence of ACP and ADs among ESKD patients in Portugal, even though medical professionals recognize their frailty and high risk of death. In the previously mentioned study,25 Farinha A et al report the causes of death of these ESKD patients undergoing hemodialysis. In one case, the cause of death was cachexia, which led to a reflection on the importance of ACP.
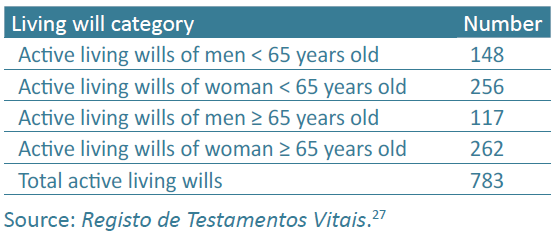
Although data on patients with ESKD are scarce, there are data from the general population in Portugal. According to the National Statistics Institute of Portugal, in 2022 10 467 366 people were living in Portugal26 and it is astonishing to note that in December of that same year, only 783 Portuguese had active LW, as can be seen in Table 1. In other words, in December 2022, less than 1% of the Portuguese population had ADs registered on the RENTEV platform.
In February 2024, there was not much change in these numbers, with only 798 active LW registered.27 These numbers are significantly lower compared to those found in the United States of America,28 where the majority of the studies mentioned in this article about ACP were conducted. Educational, religious and cultural differences probably justify these results. In Portugal, the physician is often perceived as a paternalistic figure, particularly among individuals with lower levels of health literacy.
In their study conducted in Portugal, Barreto ALF and Capelas MLV surveyed 503 healthcare professionals, including nurses, doctors, psychologists, and social service professionals, using a questionnaire. The results indicated that most healthcare professionals view ADs as a crucial tool for safeguarding patient autonomy. However, only approximately 40% feel adequately informed about the process of implementing ADs, highlighting the pivotal role of training in this aspect.29 In the same study, around 20% of health professionals reported having already consulted or proposed consulting RENTEV in a given context. Lack of time or the thought that they are not in their role are justifications proposed by the authors for this result.
In another analysis involving the same group of healthcare professionals, Barreto ALF and Capelas MLV discovered that about 85% of participants believe that health professionals provide information about ADs to their patients. However, only around 30% of healthcare professionals feel adequately prepared to provide this information, and approximately 40% inquire whether patients have ADs.30 The Portuguese data highlight that merely enacting laws is insufficient; there is a need for broad dissemination of information to both the general population and health professionals. The general population must know that they can have a word about the care that they want or not to receive in an end‑of‑life situation, if they are unable to express themselves consciously. This is extremely important for patients with ESRD, as previously mentioned, so that they can express their wishes regarding dialysis management in a terminal context.
In Portugal in 2011, was approved for the Direção Geral de Saúde a guideline31 that regulates the treatment of chronic kidney disease stage 5. This guideline establishes that all patients must be informed about their clinical condition and possible treatment modalities so that they can make an informed and shared decision. Nevertheless, nothing is mentioned in this guideline about ACP or ADs.
On the other hand, although ACP and ADs are recognized as crucial for patients with ESKD, the nephrology residency program in Portugal currently lacks any component aimed at training professionals on how to effectively discuss ACP. Healthcare professionals should understand the principles of ACP and LW, and they should be capable of initiating discussions with patients about their willingness to establish ADs. Training in this field is important and must be included in medical training plans. Also, considering the importance and intricacy of this responsibility, professionals require support from their organizations in various forms. This includes endorsement of policies, assurance of quality, establishment of administrative systems, provision of training that addresses concerns, enhances skills, and clarifies procedures, as well as staffing levels that permit adequate time for thorough implementation.21
CONCLUSION
Patients with ESRD on dialysis have many contacts with healthcare professionals, whether on dialysis sessions or in other medical appointments, and these patients should be encouraged to discuss their wishes and preferences in relation to their future in terms of healthcare, creating ADs. In this specific group of dialysis patients, it is important to know their preferences regarding the management of dialysis at the end‑of‑life, and not just their preferences regarding cardiopulmonary resuscitation or mechanical ventilation. Clarifying their wishes is crucial for the patient, as it ensures their autonomy is honored. It’s also vital for family members, alleviating stress and guilt when making decisions. Additionally, it benefits healthcare professionals, enabling them to respect the patient’s preferences. However, it is important that healthcare providers have training in this area so that they can feel more capable of approaching their patients about ACP. The physician does not have to be paternalistic, he just needs to possess the tools and skills to guide his patients towards the most appropriate choices for their clinical situation, accordingly to their personal wishes.