Cystic fibrosis (CF) is an inherited genetic disorder that triggers various clinical manifestations on the respiratory and digestive tracts. A CF diagnosis is usually established in early childhood, especially because of the widespread implementation of newborn screening (Farrell et al., 2017). Persistent chronic cough is the most common respiratory sign. More severe pulmonary complications include an increased predisposition to chronic bacterial infections and acute symptoms such as cough, dyspnoea, fatigue, and the increased production of and change in the colour of the sputum, lasting from days to weeks (Boucher, 2013). The clinical repercussions in the gastrointestinal tract may include nutrient malabsorption and a greater frequency of massive and fetid stools. For this reason, CF children also commonly present malnutrition, growth impairment, and lifelong difficulties in maintaining an adequate weight (Mota et al., 2016).
A variety of medications and procedures are often used in the treatment of CF (Boucher, 2013). The extensive routine of symptoms management, which may include enzyme intake, respiratory physiotherapy, and oxygen therapy, is typically time-consuming and, as such, the symptoms and treatment lead to school absenteeism and restricted contact with peers (Borawska-Kowalczyk et al., 2015; Kostakou et al., 2014). Moreover, children with CF may become more isolated and withdrawn because of their dissatisfaction with their body image. CF children tend to report lower levels of satisfaction with their bodies than healthy children (Pinquart, 2013a), which increases as patients grow because the effects of the disease on physical appearance become more noticeable and may prompt increased reactions from others (Groeneveld et al., 2012). Thus, children with CF may become more isolated and withdrawn due to the implications of the disease on appearance, time-consuming treatment regimens, physical performance, and socialisation constraints.
In addition to the difficulties in peer interactions, mealtime behaviour problems are more commonly reported in the families of CF children than in healthy children or paediatric patients with other chronic diseases, and tend to persist throughout development (Hammons & Fiese, 2010; Sheehan et al., 2012). Such problems usually involve either the refusal of food or of a novel texture, tantrums, crying, or whining behaviour (Driscoll et al., 2015; Ernst et al., 2011). These problems are so frequent that parents report that, although their children may comply with other aspects of care, feeding problems persist throughout development and remain worrisome (Filigno et al., 2012). Finally, daily routines that include respiratory physiotherapy tend to prompt resistance and avoidance in paediatric patients, who can misbehave and have temper tantrums in these situations (Williams et al., 2007). Thus, mealtime problems and resistance to treatment procedures added to school absenteeism, restricted contact with peers, and poor body image may result in a greater risk for developing behavioural and emotional problems (Ernst et al., 2011), for example social withdrawal, anxiety, depression, rule-breaking, and aggressive behaviour. A number of studies have shown increased rates of behavioural and emotional problems in paediatric CF patients compared to children with other chronic illnesses (Pinquart & Shen, 2011) or healthy children (Kostakou et al., 2014).
Emotional and behaviour problems constitute additional challenges for parents raising a CF child, as they need to persuade the child to comply with a demanding treatment regimen, while still going through all other normative development tasks. Strategies used by parents to regulate their children’s behaviour can either effectively contribute to control behaviour, or to intensifying these problems. The relationship between parenting strategies and children’s socio-emotional development has been explored through different theoretical perspectives; most distinguish between coercive or power assertive practices and inductive or non-coercive strategies (Baumrind, 1966; Grusec & Davidov, 2010; Hoffman, 1975, 1994).
The parental control model maintains this distinction by proposing two types of parental practices: psychological control and behavioural control (Barber, 1996; McShane & Hastings, 2009). Psychological control specifies intrusive or coercive strategies that interfere with or invalidate the child’s psychological or emotional experiences and expressions. This type of parental control is divided into two distinctive dimensions: critical control and overprotection. Critical control includes parental behaviours that indicate rejection or criticism, and insult or ridicule both children’s behaviours and their individual characteristics (McShane & Hastings, 2009). For example, when parents say “you’re very stupid, you don’t do anything right” or when they threaten to stop loving the child for misbehaving, they are using critical control. Overprotection, on the other hand, refers to excessive or unnecessary protection that restricts the child’s autonomy and hinders or reduces new socio-emotional experiences (McShane & Hastings, 2009). For instance, when parents do not allow the child to run so as not to fall or when they say something like “do you want to go home and play with Mommy?” in situations where the child shies away from interacting with another child.
Conversely, behavioural control is essentially inductive. This dimension includes the provision of appropriate support, which corresponds to parental behaviours that promote socio-emotional development through the stimulation of autonomy. Thus, it involves the contingent provision of structuring, encouragement, praise, guidance, and nurturance (McShane & Hastings, 2009). For example, when parents explain to their children that they should not eat sweets before lunch, so as not to spoil their appetite, or when they encourage a shy child by saying “why don’t you talk to your new friend?”, they are implementing behavioural control.
Previous research with CF children has revealed that appropriate support strategies such as talking to the child, describing their behaviours, valuing the child’s verbalisations, and praising their performance positively contribute to the child’s compliance and adherence to treatment (Butcher & Nasr, 2015). Behavioural control strategies are also related to positive developmental outcomes in chronically ill children, such as more positive affective expressiveness, communication skills, social responsiveness (Tluczek et al., 2015), social competence, and fewer incidences of internalising and externalising problems (Scholten et al., 2013). On the other hand, overprotection and critical control are related to problematic mealtime behaviours (Driscoll et al., 2015), poor psychosocial functioning (Cappelli et al., 1989) and a lower adherence to treatment (Butcher & Nasr, 2015) in CF children. Indeed, parents of children with chronic health problems tend to be more critical and overprotective, and to show less warmth towards their children than the parents of healthy children (Pinquart, 2013b). It is possible that such trends stem from the parents’ understanding of the severity of the diagnosis and from the pressure to comply with the treatment. However, prioritising harsh or coercive interactive patterns may lead to an increased level of internalised problems in children (Smith et al., 2010) and fewer positive outcomes in physical health, as well as in the overall course of their development (Tluczek et al., 2015).
Current study
CF has strong repercussions in both children’s daily routines and their interactions with peers, as well as requires compliance with a rigorous treatment regimen. Parental control strategies can foster or hinder children’s cooperation with routine treatment procedures and their competence for peer interaction. Research has identified the association between psychological control strategies (overprotection and critical control), behaviour problems, and a lower adherence to treatment in chronically ill children (Butcher & Nasr, 2015; Driscoll et al., 2015; Sheehan et al., 2012; Smith et al., 2010). Conversely, behavioural control strategies (appropriate support) are related to positive developmental outcomes and a higher level of adherence in this population (Butcher & Nasr, 2015; Mikesell et al., 2017; Smith et al., 2010). To the best of our knowledge, only a few studies attempted to explore these dimensions of parental control in families with paediatric CF patients (Cappelli et al., 1989; Pinquart, 2013b), but none of them examined these two dimensions of parental control in different living contexts. Since CF has strong repercussions in families’ daily routine as well as in children’s socio-emotional development, it is relevant to describe parental control practices to understand the main socialisation and treatment challenges experienced in this population, as well as the behavioural resources and risks parents may show in these contexts. The aim of the current study is to describe the control strategies reported by parents of CF children in two different contexts of their children’s life. We were guided by the following research question: What control strategies are used by parents with CF children during their daily routine, including treatment and peer interactions?
Method
Participants
The participants involved in this study comprised 14 mothers and 2 fathers of children diagnosed with CF for at least three months. As inclusion criteria, children should have a confirmed CF diagnosis, be under CF outpatient medical treatment, and have a stable clinical condition. The families attended an outpatient clinic of the public health system in Brazil, which mostly assists families from low-income backgrounds. Mothers had an average of 10.60 (DP=4.40) years of education; similarly, fathers had an average of 10.00 (SD=3.56) years. Most mothers did not work outside the home (37.5%), but most fathers did (81.3%), and 62.5% of the parents lived together. The children were 8 boys and 8 girls, with ages ranging from 5 to 12 years (M=7.00; SD=2.25), and they attended elementary or middle school. The average monthly income of the families was approximately twice the Brazilian minimum wage (Table 1). During data collection, all children were medically stable and using treatments including oral medications such as vitamins (100%) and pancreatic enzymes supplementation (87.5%), chest physiotherapy (75%), physical activity (50%), and/or oxygen therapy (12.5%). No child in the sample has had a lung transplant.
Measures
Interview on Childrearing Practices (Piccinini et al., 2007). An adapted version of this interview was used to evaluate parental control in participants’ daily routines. This is a semi-structured interview designed to evaluate parental strategies to regulate children’s behaviour. The original interview includes six common daily situations, involving children’s inappropriate behaviour or disobedience. The original measure was adapted for this study in order to include the most common daily situations for parents and children with CF: (a) food: the child refuses to eat; (b) medicine: the child refuses to take medicines or enzymes; (c) physiotherapy: the child refuses to undergo respiratory physiotherapy or oxygen therapy; (d) sleep situation: the child refuses to sleep at night; (e) tantrum: the child throws a tantrum when something is denied to them; and (f) school: the child refuses to go to school. Parents were asked to consider each situation and think about what they usually did when their children displayed these behaviours or how they would react if the situation occurred. Parents could report as many strategies as they wished. The interviews were audio recorded, transcribed, and coded based on a previously defined coding system, based on the self-report and observational measures presented by Barber (1996) and McShane and Hastings (2009). This system includes 9 distinct and mutually exclusive categories grouped within the broader dimensions of appropriate support, critical control, and overprotection.
The appropriate support dimension includes four categories: (1) Rule-setting, which refers to information about rules and limits set for children’s behaviour: “Saying that she must go, that it is her obligation to go to school, just as I have to go to work, she has to study”; (2) Reasoning, explanations which describe natural consequences of the child’s behaviour to her/himself or others: “I say, ‘this medicine is good for your health, for you to stay strong, fit. Strong to go to school, to study, and to play with your classmates’”; (3) Encouragement and warmth, displays of support and affection, including praise and positive comments in routine situations: “Look at mommy, breathe, relax, it will be all right”; (4) Sensitive Support, regarding the assurance of the necessary care or help when coping is difficult for the child because of a new challenge or extreme situation: “He lies down, I stay with him until he sleeps” (when the child was hospitalised because of a crisis). The critical control dimension includes four other categories: (5) Criticism, regarding hostility, rejection, or humiliation towards the child: “If you don’t study, you’ll look stupid”; (6) Emotional manipulation, attempting to manipulate the child’s behaviour through emotional blackmail such as guilt induction or withdrawing love or attention. It also includes emotional invalidation. For example: “I do everything for you, I buy nothing for myself, just for you, and you keep disobeying me like that”; (7) Physical punishment, physical interventions that cause pain in the child: “If she had a tantrum, I think I’d slap her”; (8) Threat, verbal threats to punish the child either physically or psychologically: “Go to sleep otherwise you will take a beating”. Finally, the overprotection dimension includes only one category: (9) Overprotection, which refers to excessive or unnecessary parental care or assistance: “When he cries so much because he doesn’t want to go to school, then I leave him at home”. The analysis of the interviews was carried out by two independent coders (undergraduate psychology students) who received 60 hours of extensive training. Reliability was established based on 10 interviews and reached 0.75 (Cohen’s Kappa), regarded as excellent (Cicchetti & Sparrow, 1981). After coding all the strategies reported in each interview, the frequencies in the 9 categories were computed.
The New Friends Vignettes (NFV) (McShane & Hastings, 2009) was used to assess parental control in the peer interaction context. This measure assesses parental control when faced with children’s behavioural inhibition and shyness in peer interaction. It presents two hypothetical situations in which parents and children meet other parents and children. The first situation describes a scenario in which the mother goes to her friend’s home with her child. The mother’s friend also has a child who is about the same age as her own child, but both children have never met before. In the second situation, the mother goes to a playground with her child and meets a few other children who are about the same age as her child. Her child already knows just one of the children playing in the playground; all the others are unknown to her. In the current study, the first situation will be referred to as one unknown child situation, and the second as several unknown children situation. For each situation, the parent responds to 18 items using a three-point Likert scale: 0 (no), 1 (maybe), or 2 (yes). The 36 items describe things he/she could say or do which correspond to the three broader dimensions of parental control (appropriate support, critical control, and overprotection). The score in each subscale corresponds to the sum of all answers and can vary between 0 and 24. This scale was adapted to Portuguese (Lins et al., 2012) and showed acceptable internal consistency (Cronbach’s alpha): 0.70 for critical control, 0.69 for overprotection, and 0.72 for appropriate support.
Procedure
This study was registered and approved by the National Commission for Research Ethics (CEP-CONEP/Brazil - process number: 2.553.871). The parents of children diagnosed with CF attending a public outpatient clinic were invited to participate in this study and were evaluated when waiting for a routine medical visit. All the parents who met the inclusion criteria provided informed consent and participated in the study. During a one-on-one interview with the researcher, participants provided socio-demographic and health information about the child and responded to both the Interview on Parental Childrearing Practices and to the NFV.
Data analysis
Absolute frequencies, percentages of specific categories, and broader dimensions of parental control were performed using the Statistical Package for the Social Sciences for Windows version 25.0 (SPSS 25.0). Then, mean (M), standard deviation (SD) and median (Mdn) were calculated, and the magnitude of the differences between parental control strategies for each context separately was examined using non-parametric statistics (Field, 2009).
Results
Parental control in daily routine
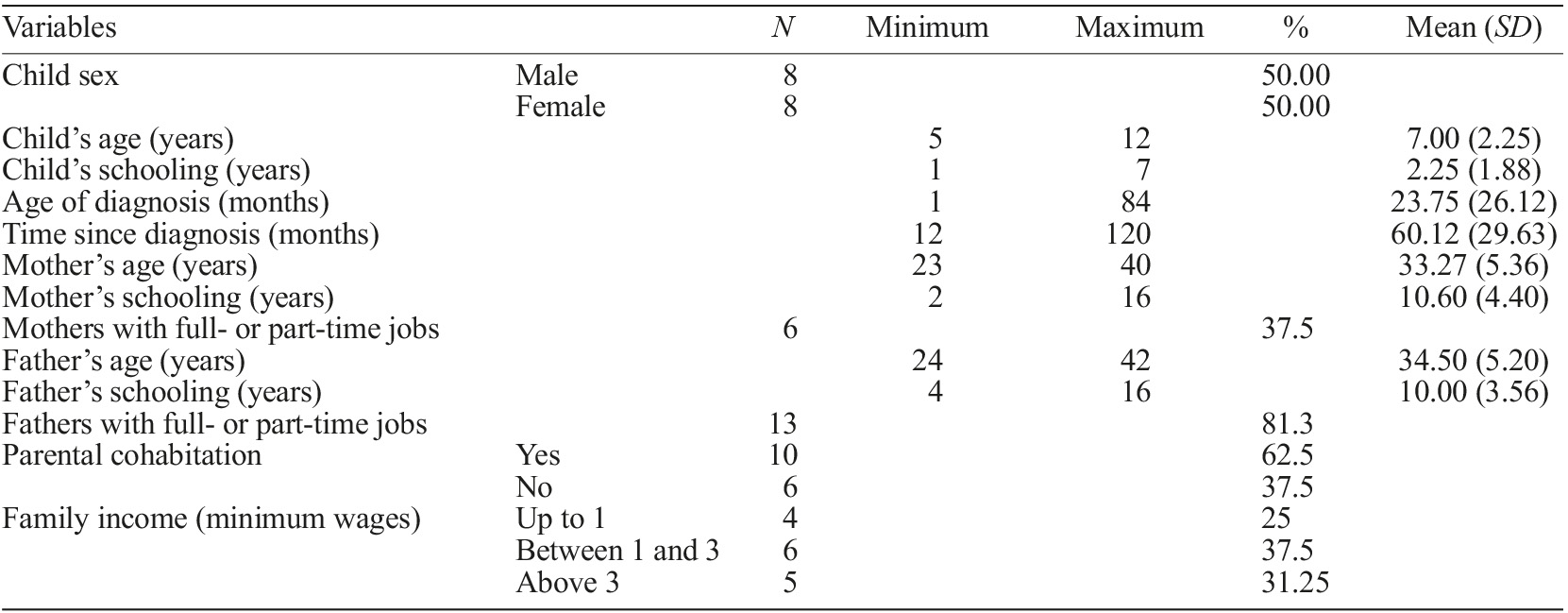
The total number of analytical units under consideration was 236. The frequencies and percentages of parental control strategies in each of the six situations of daily routine are presented in Figure 1. Appropriate support was the most frequently reported dimension in all six situations, with the food situation portraying the highest frequency. Critical control was described only a few times, particularly in the sleep situation. Overprotection was reported only by one mother in the school situation.
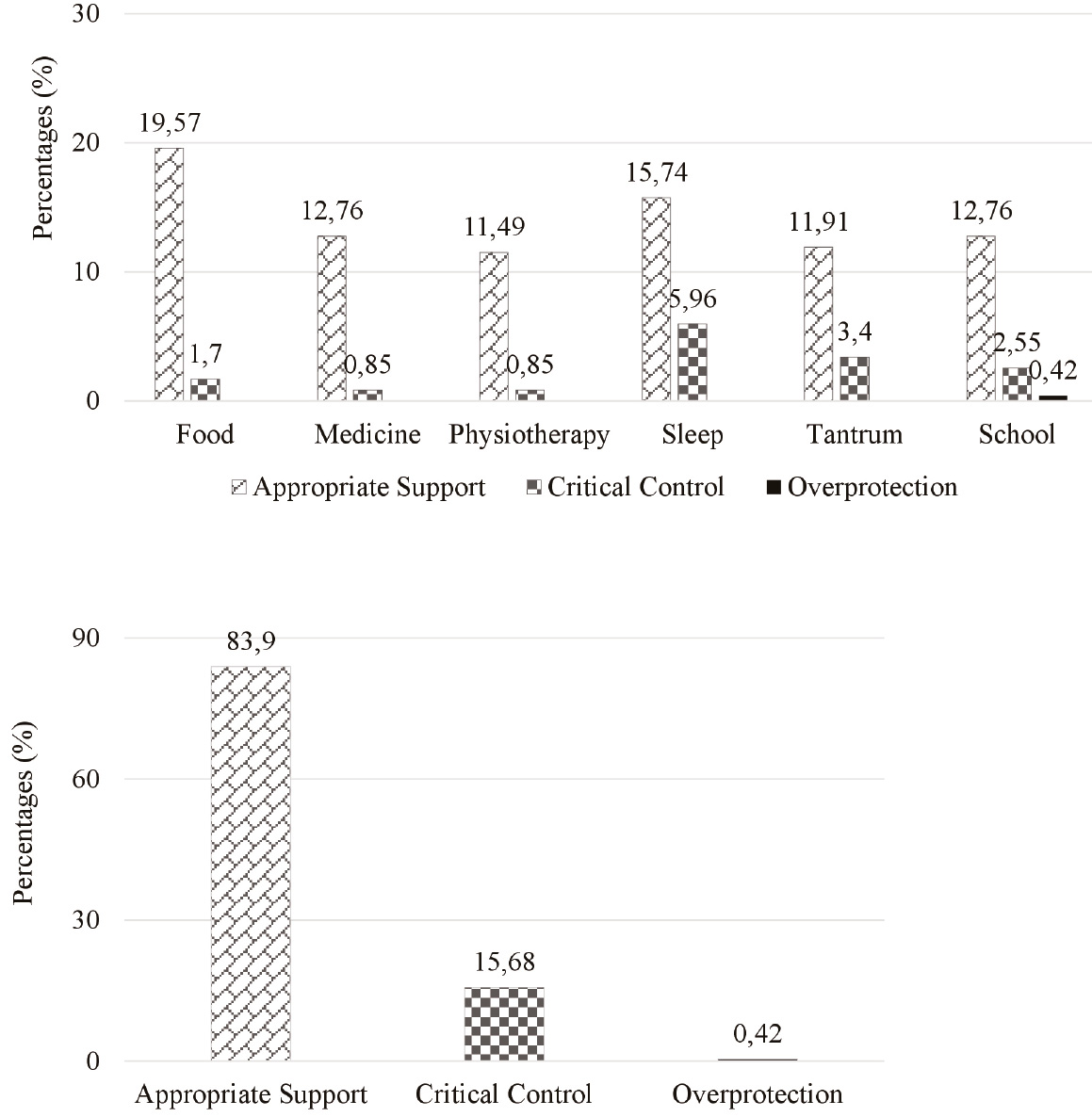
Figure 1 Percentages of broader dimensions of parental control in the six daily routine situations, separately (a) and together (b) (N=16)
The total percentages of the three broader dimensions of parental control were assessed, regardless of the situation. Appropriate support was by far the most commonly reported type of parental control in daily routine situations. The percentage of critical control was approximately five times lower when compared to appropriate support, while overprotection was reported only once by one participant.
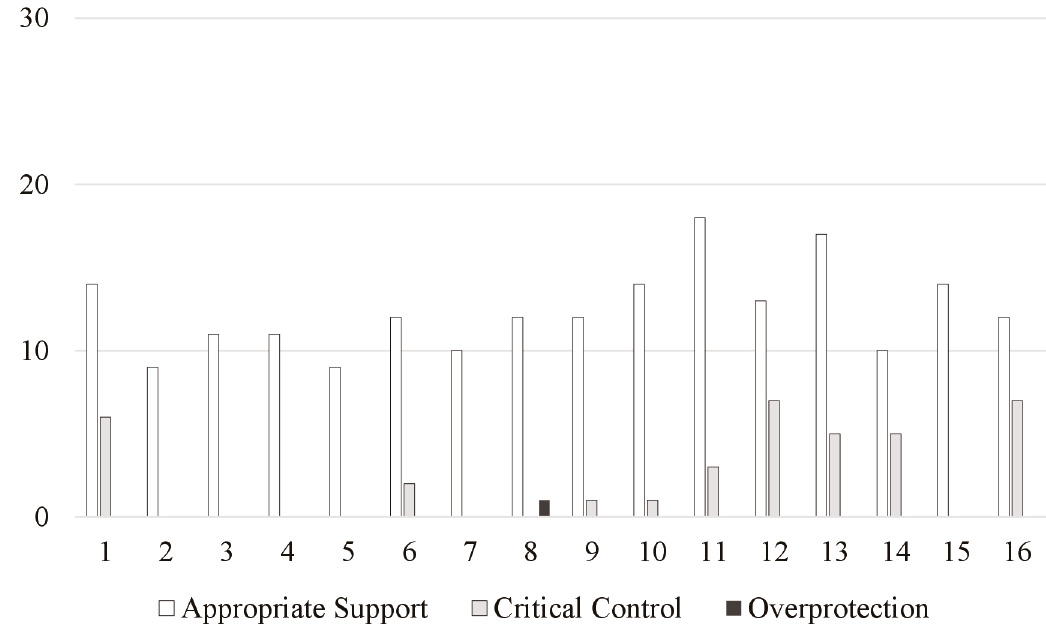
Figure 2 presents the absolute frequencies of the three broader dimensions of parental control reported by each participant. All participants reported higher frequencies of appropriate support strategies in daily routine situations, whilst six participants reported only appropriate support strategies (P2, P3, P4, P5, P7, and P15). The remainder reported predominantly appropriate support strategies, although critical control strategies appeared in low frequencies.
To examine the magnitude of the differences between parental control strategies in the daily routine, we used the Wilcoxon’s test which confirmed that appropriate support (M=14.25; SD=2.72; Mdn=14) was significantly more reported than critical control (M=2.38; SD=2.82; Mdn=1) (Z=-3.524; p<0.001). Overprotection strategies were not included in this analysis because of their low frequency.
Parental control in peer interaction
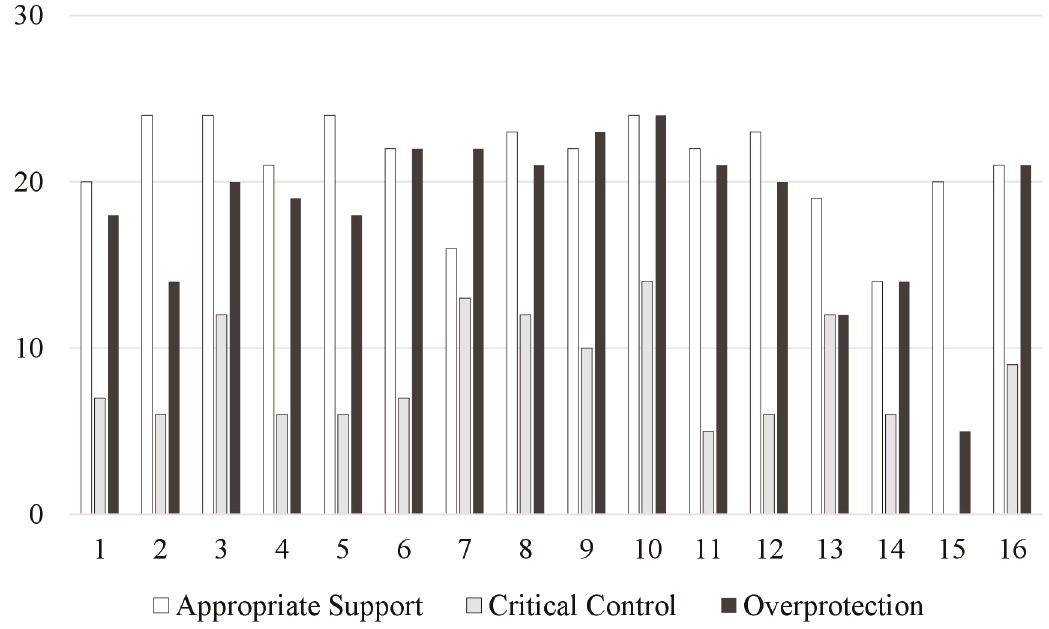
Figure 3 presents the percentages of each broader parental control dimensions in the two peer interaction situations. The percentages in the three dimensions were highly similar in the two situations, indicating that parents would adopt the same strategies regardless of the presence of one or several unknown children. Appropriate support was again the most frequently observed dimension. However, in both peer situations under consideration, critical control was the least frequently reported dimension while overprotection was mentioned with frequencies that were almost as high as the ones observed for appropriate support.
The percentages of all the strategies used in the three dimensions together were assessed, taking into account the two situations. The percentage of appropriate support was slightly higher than the percentage of overprotection, while critical control showed the lowest relative frequency.
Figure 4 illustrates the results of the analysis of the absolute frequency of the three broader dimensions of parental control reported by each participant in peer interaction. Only one participant did not report the use of critical control (P15). For 10 of the participants, appropriate support was the most common dimension. However, 2 participants reported a higher frequency of overprotection than appropriate support (P7 and P9). The remaining 4 participants reported the same frequency of appropriate support and overprotection (P6, P10, P14, and P16).
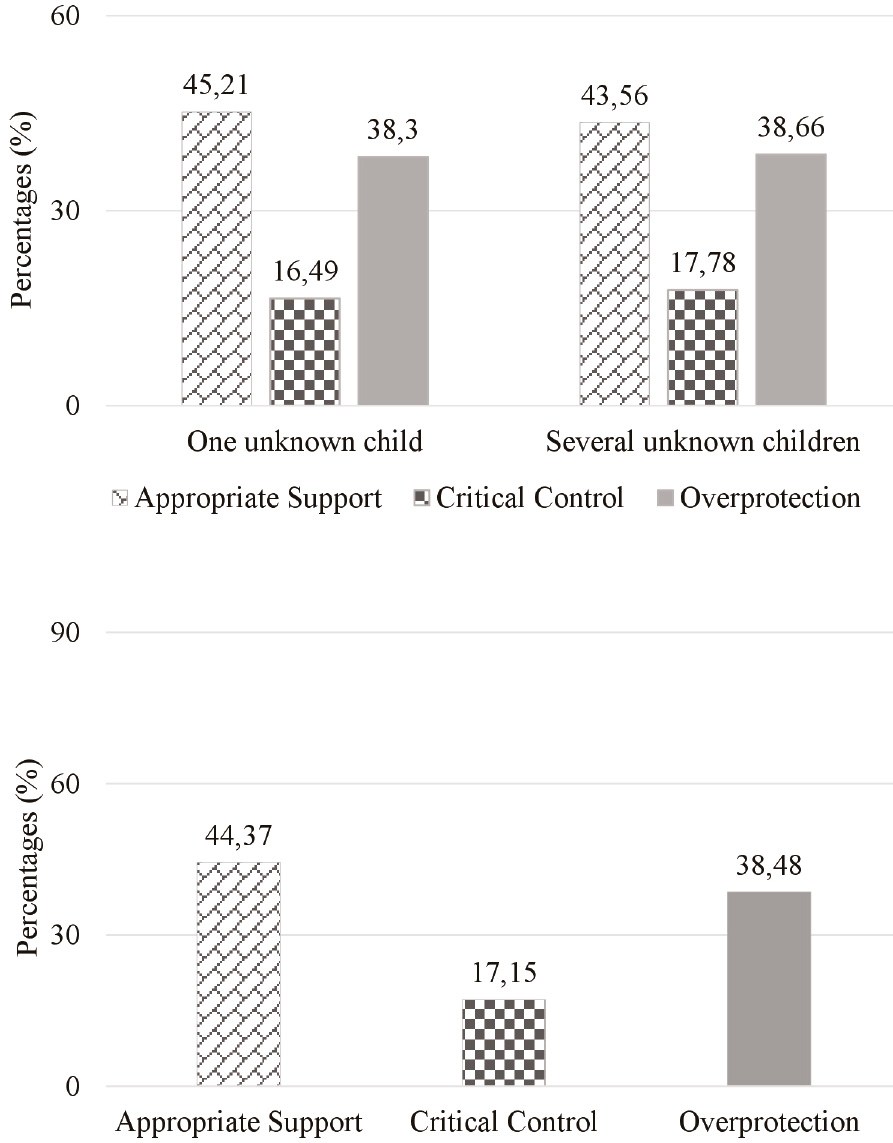
Figure 3 The broader dimensions of the percentages of parental control in the two peer interaction situations, separately (a) and together (b) (N=16)
To address the magnitude of the differences between parental control strategies in peer interactions we used Friedman’s test, which showed that parental control strategies significantly differed [χ 2 (2)=26.881; p<0.001]. In the second step of the analysis, post hoc tests were used to confirm the significant difference found and multiple pairwise comparisons were performed. A Bonferroni correction was applied and all effects were tested with a significance level of 0.0167. The multiple comparison tests showed that critical control (M=8.19; SD=3.73; Mdn=7) differed from the appropriate support (M=21.19; SD=2.91; Mdn=22) (Z=-4.861; p<0.001) and overprotection (M=18.38; SD=4.93; Mdn=20) (Z=-3.359; p=0.002).
Discussion
This study aimed to describe the parental control strategies utilised by mothers and fathers of children with CF in daily routine and peer interaction contexts. Two measures were used, a semi-structured interview for the daily routine context and a scale for the peer interaction context. The results indicated that appropriate support strategies are prominent in daily routine situations, while critical control is used in some situations; conversely, overprotection does not seem to be an important control strategy. In the peer interaction context, caregivers reported appropriate support and overprotection with similar frequencies, while the use of critical control was described at lower frequencies.
The high frequency of appropriate support in the daily routine context was a trend also identified in similar studies with physically healthy children (Alvarenga & Piccinini, 2003; Piccinini et al., 2007). On the other hand, a meta-analysis revealed that parents of children with chronic physical illnesses demonstrated less parental responsiveness and were more likely to use critical control and overprotection than parents of healthy children. However, these differences were slight (Pinquart, 2013b). In paediatric CF cases, mothers may perform the treatment and other daily routine activities using lower levels of coercion, because they understand that the child already experiences much suffering due to a painful treatment routine and the limitations imposed by the disease.
In general, parents of children with chronic conditions suffer intensely because the disease often implies irreversible changes in health and, in some cases, a threat to the child’s life (Barros, 2003). Moreover, by individually considering the results of each of the six daily routine situations, we were able to observe that parents of this sample seem to behave even more flexibly and responsively to their children’s demands in treatment-related situations compared to other non-disease-related situations. The CF diagnosis poses a threat to the child’s life and development, and its treatment is highly burdensome (Borawska-Kowalczyk et al., 2015; Douglas et al., 2016). Our results can support this trend in parental behaviour, showing that critical control frequencies were lower for daily routine treatment situations (food, medication, or physiotherapy) than in the other three situations (sleeping at night, going to school, or throwing a tantrum). The differential use of critical control might be justified by the treatment burden, which causes greater physical and emotional exhaustion in the caregivers (Barker & Quittner, 2016; Barros, 2003; Vardar-Yagli et al., 2017). Parents may be more comprehensive about the child’s negative reactions to treatment routines or be more persistent when faced with this kind of challenge than in the other common everyday situations.
Nevertheless, previous studies have noted that in families of children with a chronic disease, including CF, parents tend to use overprotective strategies more often (Pinquart, 2013b), a trend that was not observed in our results. On the other hand, parents reported a relatively high frequency of critical control and overprotection in the context of peer interaction. This overall pattern of parental interaction remained the same in situations with either one or more than one unknown child. Caregivers might be overprotective of the child when interacting with peers for fear that they will be less accepted on account of the disease (Ernst et al., 2011; Paixão & Alvarenga, 2019). As they develop, CF patients often present growth delay (Yen et al., 2013), low body mass indexes (Borawska-Kowalczyk et al., 2015), and late-onset puberty (Ernst et al., 2011), thus affecting their physical appearance and subsequent social acceptance by peers. In addition, the socio-emotional development of school-aged children involves social comparison with their peers (Ernst et al., 2011), which may further emphasise the physical differences related to the disease. Consequently, CF children may tend to be neglected by their peers and show more withdrawn behaviour due to their physical appearance, thus leading parents to implement overprotective strategies more frequently.
The results of this study must be considered in light of its limitations. CF is an uncommon disease, especially in Brazil, where the population is primarily mixed-race. All the families that met the inclusion criteria followed in the public outpatient clinic in which the study was carried out participated in this study. However, the small number of participants in our sample made robust statistical analysis impossible. The unbalanced number of mothers and fathers in the sample did not allow comparisons of different strategies used according to parents’ gender. However, a meta-analysis based on 325 studies about the parent-child relationship and parenting behaviours have shown that mothers and fathers of chronically ill children showed similar parental functioning (Pinquart, 2013a,b). Some studies report differences on the use of strategies between mothers and fathers, but these differences may be related more to family characteristics than to gender of the caregiver per se (Malm-Buatsi et al., 2015).
A second limitation refers to the measures used for the evaluation of parental control in the two evaluated contexts. A semi-structured interview was used to evaluate the daily routine context, while a scale was used to evaluate the context of peer interaction. Both measures presented situations in which children displayed difficult behaviours and required that parents described what they would do if these situations occurred. The difference between these two measures is that while in the semi-structured interview the parents openly talked about the strategies they usually adopted, in the scale they indicated how frequently they used a set of different control strategies which were described to them. The latter measure was perhaps more sensitive to specifically assess overprotection. Overprotection may be subtler and infrequent than appropriate support and critical control, when evoked by open-ended questions such as the ones included in the semi-structured interview. It is also vital to consider that participants can be influenced by social desirability and report an increased use of appropriate support control because they are aware these strategies are considered the most suitable responses. This type of bias is more likely in a less structured measure such as an interview. On the other hand, these data may also suggest that these caregivers are aware of how to best interact with their children and as such report its use more often.
The results of this descriptive study showed preliminary findings regarding parental control strategies in families of children with CF. Despite the treatment burden, parents of CF children seem to be more flexible and responsive to the child’s demands in treatment settings than when facing everyday conflicts related to feeding, sleeping, and behavioural issues or difficulties in their children’s interaction with peers. The latter context seemed to evoke overprotection in relatively high frequencies, which may be associated with parents’ fears and worries about peer acceptance. These initial findings need further scrutiny, but point to the relevance of interventions to increase parents’ awareness about their overprotective strategies, their reasons to regulate their children’s behaviour with these types of practice, and, most importantly, the risk that overprotection could result in reduced opportunities for their children to develop socio-emotional skills while interacting with peers.