INTRODUCTION
Meat allergy is becoming an increasingly recognized condition and a higher prevalence is seen in pediatric age compared to adults. In some case series meat allergy seems to represent 3-15% of all pediatric cases of food allergy1,2. The real prevalence of meat allergy in children with cow’s milk protein allergy (CMPA) is difficult to estimate. Few studies address this question, generally small and with different study methods, possibly leading to overestimations on its true epidemiology3. Only two studies reported prevalence of meat allergy in CMPA based on oral food challenges (OFC), with study samples of 15 and 25 patients, and they found that the estimated prevalence of meat allergy is between 13%4 and 20%5, respectively. When meat allergy is diagnosed during early childhood, the prognosis is usually good with clinical resolution during the first years of life1,3.
CASE REPORT
Three-year-old female child with episodes of recurrent vomiting since the first days of life under exclusive breastfeeding, and failure to thrive during the first months of life. The past history was unremarkable during pregnancy.
The endocrine metabolic disease screening was negative at the 7th day of life. She had been under exclusive breastfeeding until one month and a half and started na infant formula at that time. The investigation workup conducted by general pediatrician included: blood count, biochemistry, abdominal ultrasound, thyroid function tests, urinary culture, search for viruses in stools, which were all unremarkable.
Anti-reflux measures and a diet without CMP were proposed, with only limited adherence and a partial improvement in symptoms was noticed. At the age of 11 months an allergy study was carried out that revealed: IgE specific (sIgE) to milk 23.8 kUA/L; nBos d 4 α-lactalbumin 5.52 kUA/L; nBos d 5 β-lactoglobulin 2.82 kUA/L and nBos d 8 casein 7.59 kUA/L. An open OFC with milk was carried out, with peri-oral erythema 20 minutes after 1ml of milk intake, confirming the diagnosis of CMPA.
A diet without CMP was reinforced with improvement in weight and height and resolution of recurrent vomiting. After the OFC that confirmed the diagnosis of CMPA, several inadvertent ingestions of milk and products containing milk occurred, despite the counseling given on avoidance measures. The introduction of beef occurred around the 6th month of age, with 2-3 ingestions per week.
At the age of 7 months, minutes after ingestion of a soup with beef, the mother noticed appearance of facial erythema, palpebral and lip angioedema and irritability and, at the age of 2 years an episode of syncope minutes after the ingestion of beef was reported. A few more episodes of less severity occurred and, in those, mother couldn’t exclude any contact with milk or products containing milk and did not administer any medication or searched for medical care. Possible allergic reactions in relation to beef were not suspected by the family, since the episodes did not occur with most beef ingestions and some of them occurred with possible, but uncertain milk contamination.
She had never ingested pork. Skin prick tests (commercial extracts, Leti®, Madrid, Spain) were positive for milk extract and milk proteins (nBos d 4 α-lactalbumin, nBos d 5 β-lactoblobulin, nBos d 8 casein) and negative for chicken and pork (clinical criteria for positivity >3mm comparing to negative control; commercial extracts for beef were not available).
Specific IgEs were positive to milk, nBos d 4 α-lactalbumin, nBos d 5 β-lactoblobulin, nBos d 8 casein, cow’s, pork (Table 1) and nBos d 6 (Table 2).
Table 1 Values of specific IgE along the course of the disease
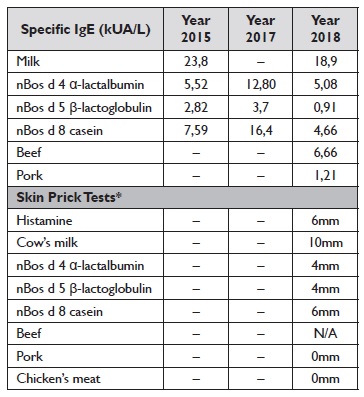
* Commercial extracts, Leti®, Madrid, Spain; N/A, Not available.
Table 2 ImmunoCAP® and ImmunoCAP inhibition
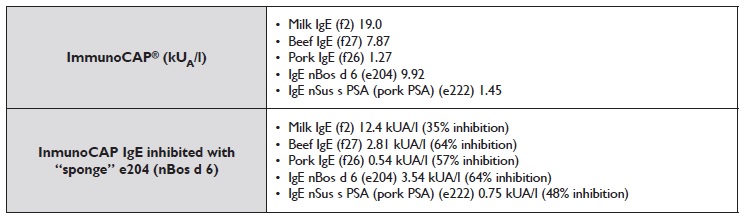
Bos d 4 - α-lactoalbumin; Bos d 5 - β-lactoglobulin; nBos d 6 - Bovine serum albumin; Bos d 8 - Casein
An OFC with well-cooked beef (steamed for 20 minutes at 100ºC) was performed and was negative until a total of 30 gr. An OFC with medium rare beef (fried 4 minutes at 45ºC) was performed and was positive within 10 minutes after ingestion of approximately 5 gr, with appearance of lip edema, peri-labial erythema and local pruritus. In order to determine if Bos d 6 could be the relevant allergen we performed an inhibition assay, briefly 150 µl of patient serum was incubated overnight with one sponge of ImmunoCAP e204 (nBos d 6), the next day we recovered the serum inhibited and performed ImmunoCAP with the patient serum and the patient serum inhibited. Percentages of inhibition were calculated with the formula (1- (sIgE inhibited/sIgE control) *100) (Table 2).
Some of the described episodes were considered as probable anaphylaxis, according to clinical criteria and a self-injector of epinephrine (150 mcg) was prescribed, along with avoidance of the implicated foods, dietary advice, anti-histamine and oral corticosteroid for mild reactions.
DISCUSSION
Immunological mechanisms associated with meat allergy can be IgE or non-IgE mediated. Clinically, three main forms of IgE-mediated meat allergy are now recognized: primary meat allergy, pork-cat syndrome and alphagal syndrome6,7.
The list of allergens associated with meat allergy includes proteins and some carbohydrates. Serum proteins and immunoglobulins seem to be the primary allergens of beef and meat from other mammals6,7. Serum albumin has been described as implicated in cow, pork, rabbit, lamb and chicken’s meat allergy7,8. Three major allergens (Bos d 6, Bos d 7, α-gal) are already identified as main causative agents implicated in bovine meat allergy7.
The existence of cross-reactivity between beef and cow’s milk has been attributed to serum albumin and gamma-immunoglobulins. The low reported prevalence of meat allergy may be partially explained by the termal lability of serum albumin and the fact that most of the meat is ingested in the cooked form5.
In our case, sensitization to Bos d 6 explains meat allergy, which can be showed by the inhibition that Bos d 6 achieves in beef and pork IgE in ImmunoCAP. The clinical presentation of a beef allergy in children is challenging as the symptoms in the first years of life can be unspecific; the presence of other food allergies, such as CMPA, may be a confounding variable and the presence of symptoms is dependent on the cooking and processing status. Since Bos d 6 is a heat labile protein, the process of cooking beef may be, in some cases, insufficient to have an effect on the complex matrix of meat and the associated serum albumins. The performance of two OFC, with well-cooked and medium-rare meat, is of great interest given that the results can be absolutely different, as the effect of cooking in meat allergy is already known. The authors consider that this strategy is of utmost importance since that a tolerance to well-cooked meat may assure a meat intake in a child with diet deficiencies, and OFC with rare meat allows to discard meat allergy. Considering tolerance to other mammalian meat, such as pork or lamb, there has been little research into whether children allergic to beef can tolerate it or not, however, considering the high degree of homology between mammalian albumins it is suggested that there is significant risk of IgE cross-reactivity between these species8.
Considering the early diagnosis, the resolution of the symptoms within the first years of life is expected. Since meat is an important source of protein, challenging in order to evaluate development of tolerance is advisable. After exposing to parents all our concerns regarding diet deficiencies, risk of reactions and expectations on development of tolerance, parents preferred waiting to introduce meat until tolerance to medium-rare meat was achieved and proved with OFC.















