Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Portuguese Journal of Nephrology & Hypertension
versión impresa ISSN 0872-0169
Port J Nephrol Hypert vol.27 no.3 Lisboa set. 2013
Diagnosis, pathophysiology and management of pre-eclampsia: a review
Diagnóstico, fisiopatologia e abordagem da pré-eclâmpsia: uma revisão
Susana Machado, Marta Neves, Luis Freitas, Mario Campos
Department of Nephrology, Centro Hospitalar e Universitário Coimbra. Coimbra, Portugal.
ABSTRACT
Pre-eclampsia is a multisystem disease that occurs in 2 to 8% of pregnant women and is a leading cause of maternal and perinatal morbidity and mortality. It is classically defined by new -onset hypertension and proteinuria after 20 weeks of gestation. In recent years, we have witnessed a substantial advance in the understanding of the pathogenesis of this condition. All disease subtypes are characterized by a disruption of vascular remodelling and a systemic antiangiogenic response that leads to hypertension, proteinuria, glomerular endotheliosis, HELLP (haemolysis, elevated liver enzymes, and low platelets) syndrome, and cerebral oedema–the clinical signs of pre -eclampsia and eclampsia. In the clinical practice, there is currently no reliable screening method in the first trimester of pregnancy with sufficient accuracy to identify women at high risk of developing pre-eclampsia, and only two interventions are strongly recommended by the World Health Organization for prevention of pre-eclampsia: calcium supplementation in all women with low dietary calcium intake and low -dose aspirin. Delivery is the only known cure. The treatment of pre–eclampsia and its complications is usually carried out by obstetricians but the role of nephrologists can be crucial, particularly when the condition is complicated by acute kidney injury. Several recent studies have shown an association between early -onset or severe pre -eclampsia and an increased risk of cardiovascular and/or renal disease later in life, suggesting that these women deserve a more careful monitoring programme, including clinical evaluation by nephrologists.
Keywords: Diagnosis; pre-eclampsia; pregnancy; prevention; treatment; vascular endothelial growth factor.
RESUMO
A pré-eclampsia e uma doença multissistémica que ocorre em 2 a 8% das gravidezes e é a principal causa de morbilidade e mortalidade materna e neonatal. Classicamente e definida pelo desenvolvimento de hipertensão e proteinuria apos a 20a semana de gestação. Nos últimos anos, temos assistido a um avanço substancial na compreensão da patogénese deste distúrbio. Todos os tipos de doença caracterizam-se por uma ruptura da remodelação vascular e uma resposta anti -angiogenica sistémica que conduzem a hipertensão, proteinuria, endoteliose glomerular, Sindroma HELLP (hemólise, enzimas hepáticas elevadas e trombocitopenia) e edema cerebral – sinais clínicos de pré-eclampsia e eclampsia. Na prática clínica actual e no primeiro trimestre de gravidez, não existe um método de rastreio fiável e com sensibilidade suficiente para identificar gravidas com elevado risco de desenvolver pré-eclampsia. A Organização Mundial de Saúde apenas recomenda duas accoes preventivas da pré-eclampsia: suplementação oral de cálcio em todas as mulheres com historia de baixa ingestão e cálcio na dieta e aspirina em baixa-dose. O parto e a única cura conhecida. O tratamento da pré-eclampsia e suas complicações e habitualmente conduzido pelos obstetras. No entanto, o papel dos nefrologistas pode ser essencial, sobretudo quando ocorre lesão renal aguda. Diversos estudos recentes, demonstram uma associação entre a pré-eclampsia precoce ou grave com um risco aumentado de doença cardiovascular e renal, anos apos o parto. De acordo com estes dados, estas mulheres deverão ser alvo de um programa de vigilância regular eventualmente com o apoio de nefrologistas.
Palavras-chave: Diagnóstico; factor de crescimento do endotélio vascular; gravidez; pré-eclampsia; prevenção; tratamento.
INTRODUCTION
Pre-eclampsia (PE) is a human pregnancy-specific disease defined by the onset of hypertension and proteinuria after 20 weeks of gestation in a previously normotensive woman. This multisystem disorder complicates 2 -8% of pregnancies in developed countries and is an important cause of maternal/perinatal morbidity and mortality. Worldwide, PE is responsible for approximately 50,000 maternal deaths annually1.
In this review, the authors describe the pathogenesis, epidemiology, diagnosis, prevention and management of PE.
PATHOGENESIS
There are many theories, and disagreements, about the final event that precipitates PE. It seems that several different initial insults converge into a common pathophysiology pathway (or two common pathophysiologies, if considering early - and late -onset PE). However, it appears clear that all subtypes of disease are characterized by a disruption of vascular remodeling and a systemic antiangiogenic response. The underlying mechanisms contributing to these changes still remain to be elucidated and might overlap.
At the beginning of a successful pregnancy, cytotrophoblast cells of fetal origin migrate through the decidua and part of the myometrium and invade maternal spiral arteries. This invasion is regulated by several factors, including the cytotrophoblast differentiation from an epithelial to endothelial phenotype (pseudovasculogenesis) and the immunological interaction between HLA molecules C, E and G and uterine natural killer cells2. The maternal spiral arteries become larger vessels of low resistance and are responsible for maintaining blood flow to the developing fetus and placenta. In pre -eclamptic women, cytotrophoblast cells do not express specific adhesion molecules of the endothelial phenotype and are unable to penetrate the myometrium. The maternal spiral arteries do not turn into larger vascular channels, leading to a decrease in uteroplacental blood flow and an increase in uterine vascular resistance3.
The mechanical constriction of uterine arteries induces placental hypoperfusion and ischaemia. Poor trophoblast invasion of maternal spiral arteries is an early event in disease progression. However, this phenomenon in not unique to PE, since it also occurs in intrauterine growth restriction in the absence of hypertension, suggesting that it alone is unable to trigger the disease4.
Placentation also requires an extensive angiogenesis to establish an appropriate vascular network to supply fetal needs. The placenta produces a wide variety of pro-angiogenic proteins (vascular endothelial growth factor [VEGF] and placental growth factor [PlGF]), and angiogenesis inhibitors, such as soluble fms -like tyrosine kinase 1 (sFlt -1) and soluble endoglin (sEng), an inhibitor of capillary formation. The balance between these pro and antiangiogenic mediators determines normal placental development4. The reduced uteroplacental perfusion and placental ischaemia causes a release of antiangiogenic factors. Levine et al.5 demonstrated an increase in circulating levels of sFlt -1, and a significant increase in the ratio of sFlt-1 to PlGF in both early - and late onset PE. sFlt-1 binds to VEGF and PlGF, preventing its interaction with endothelial receptors on the cell surface, which reduces phosphorylation of endothelial nitric oxide synthase (eNOS) and promotes endothelial dysfunction6,7. Similarly, studies have found an association between the increased placental expression and circulating levels of sEng and the development of PE. Furthermore, Venkatesha et al.8 showed a positive correlation between increased levels of sEng and disease severity.
Several experimental models have explored the role of oxygen deprivation and hypoxia –reperfusion injury in the pathophysiology of PE. Some in vitro models suggest that hypoxia is not only a consequence of abnormal trophoblast invasion of maternal spiral arteries, but also a cause of it. Hypoxia-inducible factor1 -α (HIF-1α) is a transcription factor that plays a key role in mediating cellular and systemic responses to hypoxia. Different methods of inducing excess HIF-1 α in mice (Tal et al.9 and Kanasaki et al.10) showed incomplete remodeling of maternal spiral arteries, fetal and placental growth restriction, hypertension, and proteinuria. By contrast, HIF -1α suppression reverses these symptoms. Burton and Jauniaux11 showed that pre-eclamptic placentas have multiple markers of oxidative stress, which would not be predicted by hypoxia alone, suggesting a causal role for hypoxia-reperfusion injury in PE pathogenesis. According to this theory, high-resistance maternal spiral arteries create alternating periods of hypoxia and normal oxygenation as the vessels contract and relax. An in vitro model showed that reoxygenation of hypoxic tissue results in the production of pro -inflammatory cytokines and sFlt-1.
Some articles highlight the role of a maternal immune response in the pathogenesis of PE12,13.
Several immune-associated conditions (for example, autoimmune diseases) increase the probability of a woman developing PE. Primiparity and a change of sexual partner are risk factors for PE, suggesting that the response to paternal antigens also plays a role. Some authors consider that PE arises from an exaggerated maternal vascular inflammatory response with a preponderance of Th1 - type (cytotoxic) reaction12.
This hypothesis is supported by some studies that show an abundance of soluble markers of neutrophil activation in PE and activation of the complement system. The cytokines TNF α and interleukin 6 (IL-6) are elevated in pre -eclamptic women while the placental production of the anti -inflammatory cytokine IL-10 is decreased14. These three cytokines have been used to create animal models that demonstrate the role of inflammation in PE. La Marca et al.15 and Sunderland et al.16 showed that TNFα-infused pregnant rats and baboons exhibit high blood pressure, increased urinary protein and elevated circulating levels of sFLT -1. Orshal and Khalil17 showed that IL-6 administration causes similar increases in blood pressure and proteinuria in pregnant rats, although sFLT-1 levels in these animals were not assessed. Additionally, exposure of an IL-10-knockout mouse to a hypoxic environment during pregnancy resulted in PE symptoms, whereas only fetal growth restriction occurred in wild-type mice exposed to hypoxia (Lai et al.18). Inhibition of IL-10 by passive immunization (i.e., with a monoclonal antibody to IL-10) during early gestation increases blood pressure in baboons.
Autoantibodies to angiotensin II type I (AT1) receptors and phospholipids have been verified in some women with PE and these might increase disease risk (Redman and Sargent19 and Abou-Nassar et al.20). In rats, the injection of anti-AT1-receptor antibodies during pregnancy induces hypertension, proteinuria and defects in vascular remodelling. Moreover, it also increases HIF -1α expression, suggesting a potential pathophysiological link between hypoxic and immune factors (Wenzel et al.21).
The kidney in pre-eclampsia
The VEGF plays a critical role in the maintenance of normal glomerular endothelial integrity and genetic glomerular VEGF deficiency has been shown to result in endotheliosis with loss of fenestrae. The main production of VEGF within the glomerulus arises from the podocytes and, additionally, podocytes express VEGF -Receptor -1 in their membranes. The VEGF acts as an autocrine factor on the podocyte, reducing apoptosis and promoting podocyte survival22. Circulating sFlt1, originating from the placenta, is able to bind and sequester VEGF, resulting in endothelial cell damage. Podocyte changes in PE include decreased expression and altered distribution of important podocyte proteins – synaptopodin, nephrin, GLEPP-1, podoplanin – and podocyte detachment in kidney biopsies and podocyturia. How VEGF-deficient states, such as PE, produce proteinuria is not entirely known. Nephrin is an essential component of the slit diaphragm, but it also signals within the podocyte, regulating the actin cytoskeleton and, thereby, the podocyte shape. VEGF interacts with the cytoplasmic domain of nephrin and through this binding reduces podocyte cell size, regulates the foot process structure and glomerular filter integrity23.
Moreover, animals exposed to high levels of sEng had focal endotheliosis without significant proteinuria, whereas those that were exposed to both sEng and sFlt1 developed massive proteinuria and severe endotheliosis. The effects of sEng may be propagated through the disruption of transforming growth factor beta 1 (TGFβ1) signalling with subsequent impairment of TGFβ1-mediated activation of eNOS24. Since eNOS is of prime importance in regulating vascular tone and also displays angiogenic properties, abrogation of eNOS as a result of elevated sEng levels induces endothelial cell injury and defects in vasodilation24.
DIAGNOSIS AND RISK FACTORS
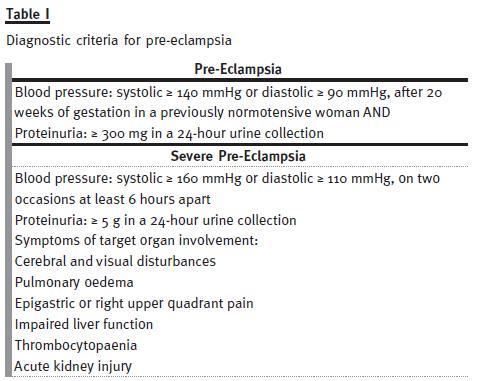
The clinical manifestations of PE are non-specific even in severe disease. The most common symptoms are epigastric or right upper quadrant pain reported in 40-90% of patients. The diagnosis of PE depends on assessing blood pressure and proteinuria, typically by a 24 -hour urine collection. The use of the urine protein to creatinine ratio is a more convenient method for the patient, however its use in pregnancy is controversial, and published studies are discordant25.
The most widely accepted diagnostic criteria for PE are presented in Table I. Beyond proteinuria, the manifestations of renal damage may include acute decrease in effective renal plasma flow and glomerular filtration rate (in 30 to 40% of the patients), and podocyturia. Serum creatinine often remains normal or only slightly increased (1 -1.5 mg/dL), except in severe PE, in which moderate/severe acute kidney injury (AKI) can develop. Renal tubular function is also impaired in PE, with an early dysfunction of uric acid tubular secretion. The urine sediment is usually benign. The histologic lesion associated with PE is glomerular endotheliosis26. The glomeruli are enlarged and solidified as a result of narrowed or occluded capillary lumens due to swollen native endothelial cells and, to a lesser extent, mesangial cells. Glomerular cellularity is not significantly increased and the endothelial changes are limited to the glomerular capillaries; arterioles are typically unaffected. Vascular thrombosis seen on light microscopy is unusual.
In severe PE, particularly with the evolution/resolution of the lesions, mesangial interposition may be seen. Others changes, such as proeminent podocytes with protein reabsorption droplets and endocapillary foam cells, are secondary to proteinuria. Immunofluorescence may reveal the presence of fibrin deposits in glomeruli26. Some authors report low-level glomerular immunoglobulin deposition in severe PE that probably represents non-immunologic insudation23.
Electron microscopy reveals endothelial cells with loss of fenestrations, cytoplasmic swelling owing to fluid and lipid accumulation and capillary occlusion. Mesangial cells may show similar changes.
Podocytes show limited foot process effacement despite significant proteinuria26.
Regarding the diseases severity, PE is divided into 2 groups: mild and severe. Severe PE comprises more substantial blood pressure elevations, a greater degree of proteinuria and symptoms of target organ involvement. PE can also be classified into early-onset and late -onset27 and these subtypes may represent different forms of the disease. Early-onset PE (before the 34th week of gestation) is often associated with abnormal uterine and umbilical artery Doppler ultrasound waveforms, fetal growth restriction and adverse maternal and perinatal outcomes.
Late-onset PE (after the 34th week of gestation) seems to be strongly associated with maternal features (for example, body mass index), normal or slightly increased uterine artery resistance index and minimal fetal involvement27.
Several factors have been proven to increase the risk of PE, such as: age (pregnant women older than 40 years); maternal obstetric factors (nulliparity, multiple gestation pregnancy, previous PE and molar pregnancy); paternal obstetric factors (father born from a pre-eclamptic pregnancy); maternal comorbid conditions (chronic hypertension, renal disease, pre-gestational diabetes mellitus, obesity and rheumatic disease); maternal genetic factors (antiphospholipid antibody, factor V Leiden mutation and PE in a first-degree relative´s pregnancy)28.
PREDICTIVE MODELS AND PREVENTIVE INTERVENTIONS
Screening for PE attempts to identify high-risk pregnancies in an effort to modify antenatal care and institute preventive measures in order to reduce maternal and fetal complications. In the clinical practice, there is currently no reliable screening method in the first trimester of pregnancy with sufficient accuracy to identify women at a high risk of developing PE. Guidelines from the National Institute for Health and Clinical Excellence (NICE)29 recommend routine screening for specific risk factors for PE (nulliparity, older age, high body mass index, family history of PE, underlying renal disease or chronic hypertension, multiple pregnancy, more than 10 years between pregnancies, and a personal history of PE). The expected rate of PE when any one of these risk factors is present ranges from 3% to more than 30% and, in prospective studies of general obstetric populations, the reported performance of a limited number of clinical risk factors to predict PE is modest30. A prospective and multicentre cohort of healthy nulliparous women, the SCOPE (Screening for Pregnancy Endpoints) study, developed a multivariable predictive model for PE based on clinical risk factors present in early pregnancy in combination with ultrasound estimates of uteroplacental perfusion and fetal measurements at 19-21 weeks gestation. The proposed algorithm performed better than the NICE guidelines, predicting 34% of cases of PE and 53% of cases of preterm PE30. Poon et al.31 recently published a prediction algorithm at 11-13 weeks of gestation that combine maternal characteristics, uterine artery pulsatility index, mean arterial blood pressure, median serum pregnancy-associated plasma protein-A and PlGF values. The detection rates of early-PE and late-PE were 95.3% and 45.6%, respectively. A systematic review studied the current literature on the predictive potential of first-trimester serum markers (ADAM12, fβ -hCG, Inhibin A, Activin A, PP13, PlGF, and PAPP -A) and of uterine artery Doppler velocity waveform assessment. Low levels of PP13, PlGF, and PAPP-A and elevated level of Inhibin A were found to be significantly associated with the development of PE later in pregnancy32. The detection rates of single markers in the prediction of early-onset PE were relatively low, and ranged from 22% to 83%. Detection rates for combinations of multiple markers varied between 38% and 100% and show promise in identifying patients at high risk for PE development. Large scale prospective studies are, however, required to evaluate the power of this integrated approach in the clinical practice.
The general term prevention can have three different connotations: primary, secondary, or tertiary.
Primary prevention of PE involves avoiding pregnancy in women at high risk, lifestyle modification or improving nutrient intake in the entire population. Secondary prevention, in the context of PE, implies breaking off the disease process before clinically recognizable disease emerges. Tertiary prevention relies on the use of treatment to avoid PE complications.
A number of trials, reviews, and protocols evaluating strategies for the prevention of PE are available in the scientific literature. Despite the variety of possible prophylactic interventions described, studies have produced disappointing results. Interventions such as rest, exercise, reduced salt intake, garlic, marine oil, daily supplementation with magnesium, vitamin C, D or E, diuretics, progesterone and nitric oxide showed insufficient evidence to modify the outcomes of PE33,34,35. Two interventions are strongly recommended by the World Health Organization (WHO) for prevention of PE36: (1) Calcium supplementation at doses of 1.5 – 2.0 g of elemental calcium/day in all women, but especially those at high risk of developing PE, if dietary calcium intake is low (< 600 mg/day); (2) Low -dose aspirin (75 mg/day) in women at high risk of developing this condition.
TREATMENT
The treatment of PE depends essentially on illness severity, gestational age and fetal wellbeing. Delivery is the best treatment for PE, but an expectant approach is also recognized in specific situations.
Worsening maternal condition (such as AKI), eclampsia or signs of fetal compromise, are considered indications for prompt delivery regardless of gestational age. Figure 1 represents a proposed algorithm for PE management28.
The role of the nephrologist is crucial in the treatment of AKI related to PE. Administration of intravenous fluids should be started as soon as possible, not only to restore or maintain renal perfusion, but also to prevent hypovolemia and ensure an adequate uteroplacental perfusion and fetal wellbeing. However, fluid balance should be monitored closely to avoid overload, since women with severe disease are at risk of pulmonary oedema and significant third-spacing. Maintenance fluids at a perfusion rate of 80 mL/hour are often adequate.
Antihypertensive drugs should be used for emergency treatment of severe hypertension (systolic blood pressure (SBP) > 160 mmHg and/or diastolic blood pressure (DBP) > 110 mmHg). The goal of antihypertensive treatment is to maintain SBP between 140 mmHg and 155 mmHg, and DBP between 90 and 105 mmHg37. Some of the antihypertensive drugs commonly used in the general population (angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists) are contraindicated in pregnancy. Diuretics are not recommended because of the high risk for volume depletion and are only indicated for treatment of pulmonary oedema. There are some controversies regarding the best drug for the treatment of hypertension during pregnancy. The most commonly used drugs are methyldopa, s -blockers and dihydropyridine calcium channel blockers (such as nifedipine).
Methyldopa is regarded as a first-line drug for the maintenance treatment of hypertension in pregnancy, because it is safe, effective and the subject of many studies28,37. It is an α-agonist agent that decreases central vascular resistance without decreasing cardiac output. Dosing is started at 750 mg/day, with a maximum dose of 3 g/day. Intravenous hydralazine and labetalol are recommended for the treatment of hypertensive emergencies. However, some authors associate the use of hydralazine with a higher risk of persistent hypertension, hypotension, caesarean delivery, oliguria, abruptio placentae, abnormal fetal heart rate, and low Apgar scores38. These authors consider that the results are not robust enough to guide clinical practice but do not support the use of hydralazine as a first -line drug for the treatment of hypertensive crises in pregnancy.
Other complications of AKI can arise in PE, particularly hyperkalemia, metabolic acidosis and anaemia.
The administration of insulin, glucose and ion exchange resin are recommended for the treatment of hyperkalemia. There are no published data regarding the use of resin in pregnant women, but this drug has a local action within the gastrointestinal tract, therefore, there is no reason for a fetal deleterious effect. In the healthy pregnant woman, a 4 mEq/L decrease in bicarbonate concentration is common.
This fact has to be taken into account when correcting metabolic acidosis with sodium bicarbonate.
Regarding anaemia associated with AKI, blood transfusion is recommended in acute therapy. The erythropoiesis-stimulating agents are safe in pregnancy, but higher doses are usually required to obtain the desired therapeutic effect28.
The indications for dialysis are the same as for the general population with severe AKI: uraemic symptoms (encephalopathy, pericarditis or neuropathy), volume overload, hyperkalemia and/or metabolic acidosis unresponsive to initial medical treatment.
Notwithstanding, many authors recommend starting dialysis earlier, when GFR falls to below 20 ml/min per 1.73 m239. Despite the absence of randomized trials showing benefits of a specific dialysis modality, in most cases the choice falls on intermittent haemodialysis. Some aspects must be considered when prescribing dialysis in pregnant women.
Increasing the dialysis dose leads to an increase in fetal survival and decrease in prematurity. A daily dialysis program (more than 20 hours/week) should thus be established40,41 in order to: (a) improve the uraemic environment, a high risk factor for prematurity and polyhydramnios, and (b) minimize haemodynamic fluctuations during haemodialysis that adversely affect uteroplacental perfusion and increase the risk of placental oxidative stress. When establishing a dry weight, it is important not to forget the normal weight gain (0.3 -0.5 kg/week) in the second and third trimesters. Some dialysate parameters should be tailored in pregnant women, such as bicarbonate to 25 mEq/L and sodium to 135 mEq/L28.
Heparin and low-molecular-weight heparin are safe in pregnancy since they do not cross the placental barrier. Both can be used during haemodialysis treatment40.
MATERNAL AND PERINATAL OUTCOMES
The maternal and perinatal outcomes in PE depend on gestational age at onset, disease severity, maternal comorbid conditions and type of care provided to the pregnant woman. In mild PE, the prognosis is usually favourable, whereas severe PE is associated with maternal and neonatal complications1,2.
The major fetal complication is growth restriction, reported in 10 to 25% of cases of severe PE. Hypoxaemic neurologic damage (< 1%) or perinatal death (1.2%)28 can seldomly occur.
Severe PE may trigger early and late complications in pregnant women. The most frequent immediate maternal complications are disseminated coagulopathy/haemolysis, elevated liver enzymes and low platelet count (HELLP) syndrome (10%-20%), pulmonary oedema (2%-5%), AKI (1%-5%) and abruptio placentae (1%-4%)28. After delivery, the hypertension and proteinuria of PE disappears within a few days to weeks.
Exceptionally, proteinuria may still be detected until 6 months after delivery. A renal biopsy should be performed if proteinuria persists for more than 6 months and whenever it is accompanied by an active urine sediment and/or rapidly deteriorating renal function.
Long-term epidemiologic studies point to an increased risk of cardiovascular diseases (chronic hypertension, ischaemic heart disease, stroke and venous thromboembolism) in women who developed PE, especially those with early -onset or recurrent PE1,27. In two large studies conducted by Mongraw-Chaffin et al.42 and Fraser et al.43, these women had an eight- to nine-fold increased risk of death from cardiovascular events compared with women without history of PE. Several studies have shown that women with a history of early-onset/severe PE exhibit impaired endothelial function, vasodilation, higher levels of fasting glucose, insulin and dyslipidaemia many years after pregnancy27,42,43. This late cardiovascular morbidity may reflect an underlying predisposition in the women for both disorders and/or permanent arterial damage caused by mechanisms behind PE. Some authors advocate that increases insulin resistance, sympathetic and pro -inflammatory overactivity, endothelial dysfunction, and the abnormal lipid profile in PE constitute an early manifestation of the metabolic syndrome, thereby putting affected women at an increased risk for cardiovascular disease44.
Pre-eclamptic women may be at increased risk of developing end-stage renal disease (ESRD) later in life45. This data is supported by a Norwegian study that demonstrated a four-fold increase in risk of ESRD compared with women without PE46.
In conclusion, despite being known as a pregnancy-specific disease, recent data show that pre–eclampsia can determine the prognosis of these women, increasing the risk of cardiovascular disease and end-stage renal disease. Consequently, pre-eclamptic women deserve a monitoring programme beyond 6 months after childbirth, which may benefit from the collaboration of nephrologists.
References
1. Carty DM, Delles C, Dominiczak AF. Preeclampsia and future maternal health. J Hypertens 2010;28(7):1349-1355 [ Links ]
2. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet 2010;376(9741):631-644 [ Links ]
3. Yagel S. Angiogenesis in gestational vascular complications. Thromb Res 2011;127(Suppl 3):S64 -S66 [ Links ]
4. Silasi M, Cohen B, Karumanchi SA, Rana S. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin North Am 2010;37(2):239-253 [ Links ]
5. Levine RJ, Maynard SE, Qian C, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 2004;350(7):672-683 [ Links ]
6. De Vivo A, Baviera G, Giordano D, Todarello G, Corrado F, Danna R. Endoglin, PlGF and sFlt-1 as markers for predicting pre -eclampsia. Acta Obstet Gynecol Scand. 2008;87(8):837-42 [ Links ]
7. Foidart JM, Schaaps JP, Chantraine F, Munaut C, Lorquet S. Dysregulation of anti-angiogenic agents (sFlt -1, PLGF, and sEndoglin) in preeclampsia: a step forward but not the he definitive answer. J Reprod Immunol 2009;82(2):106-111 [ Links ]
8. Venkatesha S, Toporsian M, Lam C, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 2006;12(6):642-649 [ Links ]
9. Tal R, Shaish A, Barshack I, et al. Effects of hypoxia -inducible factor -1alpha overexpression in pregnant mice: possible implications for preeclampsia and intrauterine growth restriction. Am J Pathol 2010;177(6):2950-62 [ Links ]
10. Kanasaki K, Palmsten K, Sugimoto H, et al. Deficiency in catechol -O –methyltransferase and 2-mehoxyoestradiol is associated with pre -eclampsia. Nature 2008;453(7198):1117-1121 [ Links ]
11. Burton GJ, Jauniaux E. Oxidative stress. Best Pract Res Clin Obstet Gynaecol 2011;25(3):287-299 [ Links ]
12. Matthiesen L, Berg G, Ernerudh J, Ekerfelt C, Jonsson Y, Sharma S. Immunology of preeclampsia. Chem Immunol Allergy 2005;89:49-61 [ Links ]
13. Eiland E, Nzerue C, Faulkner M. Preeclampsia 2012. J Pregnancy 2012;2012:586578 [ Links ]
14. Pinheiro MB, Martins -Filho OA, Mota AP, et al. Severe preeclampsia goes along with a cytokine network disturbance towards a systemic inflammatory state. Cytokine 2013;62(1):165-173 [ Links ]
15. LaMarca BB, Bennett WA, Alexander BT, Cockrell K, Granger JP. Hypertension produced by reductions in uterine perfusion in the pregnant rat: role of tumor necrosis factor-alpha. Hypertension 2005;46(4):1022-1025 [ Links ]
16. Sunderland NS, Thomson SE, Heffernan SJ, et al. Tumor necrosis factor alpha induces a model of preeclampsia in pregnant baboons (Papio hamadryas). Cytokine 2011;56(2):192-199 [ Links ]
17. Orshal JM and Khalil RA. Interleukin -6 impairs endothelium -dependent NO -cGMP-mediated relaxation and enhances contraction in systemic vessels of pregnant rats. Am J Physiol Regul Integr Comp Physiol 2004;286(6):R1013-R1023 [ Links ]
18. Lai Z, Kalkunte S, Sharma S. A critical role of interleukin-10 in modulating hypoxia-induced preeclampsia -like disease in mice. Hypertension 2011;57(3):505 -514. [ Links ]
19. Redman CW and Sargent IL. Immunology of pre -eclampsia. Am J Reprod Immunol 2010;63(6):534-543 [ Links ]
20. Abou-Nassar K, Carrier M, Ramsay T, Rodger MA. The association between antiphospholipid antibodies and placenta mediated complications: a systematic review and meta-analysis. Thromb Res 2011;128:77-85 [ Links ]
21. Wenzel K, Rajakumar A, Haase H, et al. Angiotensin II type 1 receptor antibodies and increased angiotensin II sensitivity in pregnant rats. Hypertension 2011;58(1):77 -84 [ Links ]
22. Foster RR. The importance of cellular VEGF bioactivity in the development of glomerular disease. Nephron Exp Nephrol 2009;113(1):e8-e15 [ Links ]
23. Wagner SJ, Craici IM, Grande JP, Garovic VD. From placenta to podocyte: vascular and podocyte pathophysiology in preeclampsia. Clin Nephrol 2012;78(3):241 -249 [ Links ]
24. Muller -Deile J, Schiffer M. Renal involvement in preeclampsia: similarities to VEGF ablation therapy. J Pregnancy 2011;2011:176973 [ Links ]
25. Morris RK, Riley RD, Doug M, Deeks JJ, Kilby MD. Diagnostic accuracy of spot urinary protein and albumin to creatinine ratios for detection of significant proteinuria or adverse pregnancy outcome in patients with suspected pre-eclampsia: systematic review and meta-analysis. BMJ 2012;345:e4342 [ Links ]
26. Stillman IE, Karumanchi SA. The glomerular injury of preeclampsia. J Am Soc Nephrol 2007;18(8):2281-2284 [ Links ]
27. Paruk F, Moodley J. Maternal and neonatal outcome in early - and late-onset pre-eclampsia. Semin Neonatol 2000; 5(3):197-207 [ Links ]
28. Machado S, Figueiredo N, Borges A, et al. Acute kidney injury in pregnancy: a clinical challenge. J Nephrol 2012;25(1):19-30 [ Links ]
29. National Institute for Health and Clinical Excellence. NICE clinical guideline 62. Antenatal care: routine care for the healthy pregnant woman. NICE, 2010 [ Links ]
30. North RA, McCowan LM, Dekker GA, et al. Clinical risk prediction for pre-eclampsia in nulliparous women: development of model in international prospective cohort. BMJ 2011;342:d1875 [ Links ]
31. Poon LC, Kametas NA, Pandeva I, Valencia C, Nicolaides KH. Mean arterial pressure at 11(+0) to 13(+6) weeks in the prediction of preeclampsia. Hypertension 2008;51(4):1027-1033 [ Links ]
32. Anderson UD, Olsson MG, Kristensen KH, Akerstrom B, Hansson SR. Review: Biochemical markers to predict preeclampsia. Placenta 2012;33 Suppl:S42-47 [ Links ]
33. Costa FS, Murthi P, Keogh R, Woodrow N. Early screening for preeclampsia. Rev Bras Ginecol Obstet 2011;33(11):367-375 [ Links ]
34. Bezerra Maia E, Holanda Moura S, Marques Lopes L, Murthi P, da Silva Costa F. Prevention of preeclampsia. J Pregnancy 2012;2012:435090 [ Links ]
35. Salles AM, Galvao TF, Silva MT, Motta LC, Pereira MG. Antioxidants for preventing preeclampsia: a systematic review. ScientificWorldJournal 2012; 2012:243476 [ Links ]
36. WHO Recommendations for Prevention and Treatment of Pre -eclampsia and Eclampsia. Geneva: World Health Organization; 2011 [ Links ]
37. Noronha Neto C, de Souza AS, Amorim MM. Pre-eclampsia treatment according to scientific evidence. Rev Bras Ginecol Obstet 2010; 32(9):459-468 [ Links ]
38. Vest AR, Cho LS. Hypertension in pregnancy. Cardiol Clin 2012;30(3):407 - 423 [ Links ]
39. Krane NK, Hamrahian M. Pregnancy: kidney diseases and hypertension. Am J Kidney Dis 2007;49(2):336-345 [ Links ]
40. Gammill HS, Jeyabalan A. Acute renal failure in pregnancy. Crit Care Med 2005;33(10 Suppl):S372 -S384 [ Links ]
41. Anantharaman P, Schimdt R, Holley J. Pregnancy & renal diseases. In: Nissenson A,Berns J, Lerma E, eds. Current diagnosis and treatment: nephrology and hypertension, McGraw-Hill; International Edition. 2009:497 -498 [ Links ]
42. Mongraw-Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension 2010;56(1):166-171 [ Links ]
43. Fraser A, Nelson SM, Macdonald-Wallis C, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age. Circulation 2012;125(11):1367-1380 [ Links ]
44. Stekkinger E, Zandstra M, Peeters LL, Spaanderman ME. Early-onset preeclampsia and the prevalence of postpartum metabolic syndrome. Obstet Gynecol. 2009;114(5):1076-1084 [ Links ]
45. Facca TA, Kirsztajn GM, Sass N. Preeclampsia (marker of chronic kidney disease): from genesis to future risks. J Bras Nefrol 2012;34(1):87-93 [ Links ]
46. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end -stage renal disease. N Engl J Med. 2008;359(8):800-809 [ Links ]
Dra. Susana Machado
Department of Nephrology, Centro Hospitalar e Universitario Coimbra
Praceta Professor Mota Pinto,
3000 -075 Coimbra
Portugal
E-mail: susana_machado_@hotmail.com
Conflict of interest statement. None declared.
Received for publication: 31/07/2013
Accepted: 18/08/2013














