Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.30 no.1 Lisboa mar. 2016
CASE REPORT
Pulmonary cement embolism in haemodialysis
Vladimir Petkov Stoyanov1, Maria Jose Gutierrez Sanchez1, Arelys Yauner Loza2, Juan Antonio Martin Navarro1
1 Department of Nephrology and Dialysis, Hospital Universitario del Tajo
2 Department of Radiology, Hospital Universitario del Tajo, Madrid, Spain
ABSTRACT
Chronic care in haemodialysis patients usually requires a multi-system approach. Metabolic bone disorders in chronic kidney disease often cause physical disabilities and require new therapeutic strategies to maintain a good quality of life. Percutaneous cement vertebroplasty and balloon kyphoplasty are widely used to treat compressive vertebral fractures but higher rate of comorbidities in renal patients often cause some complications. We present an unusual case of late pulmonary cement embolism in an elderly haemodialysis patient. Curiously, in spite of a large number of vertebral augmentation procedures performed in the world, this is the first report of pulmonary cement embolism in a dialysis patient.
Key-Words: Haemodialysis; balloon kyphoplasty; pulmonary cement embolism; vertebral augmentation procedures; vertebral compressive fractures
BACKGROUND
Chronic care for haemodialysis (HD) patients requires a multi-system approach managing wide range of pathologies frequently unrelated to the kidneys or cardiovascular system. Metabolic bone disorders (MBD) usually present in chronic kidney disease (CKD) and a growing life expectancy in the population under renal replacement therapy (RRT) often cause physical disabilities requiring new strategies to maintain a good quality of life. The combination of multiple diseases and aggressive treatments in this population also increases the complications frequency that can be found. We present an unusual case of pulmonary cement embolism (PCE) diagnosed in an elderly HD patient.
CASE PRESENTATION
A 76-year-old man undergoing HD was admitted to hospital because of biliary origin sepsis. His summarized medical history includes:
Orthotopic heart transplantation due to severe coronary heart disease at age 56, complicated with deep vein thrombosis and pulmonary thromboembolism 50 days after surgery. His usual long-term immunosuppressive treatment includes Prednisone, Cyclosporine and Sirolimus.
Currently he has cardiac graft dysfunction with NYHA class III chronic heart failure (CHF).
End stage renal disease (ESRD) due to Cyclosporine toxicity, having begun HD at age 69. Kidney transplantation performed at 70 with early graft loss due to chronic allograft nephropathy, rebooting HD at age 71.
Superior vena cava thrombosis due to repeated central dialysis line insertion for HD, diagnosed 18 months before the current admission, resulting in continued treatment with acenocoumarol.
His vascular access history includes 1 arteriovenous fistula, 2 PTFE grafts and at least 6 longterm central vein catheters (CVC) in jugular and subclavian veins.
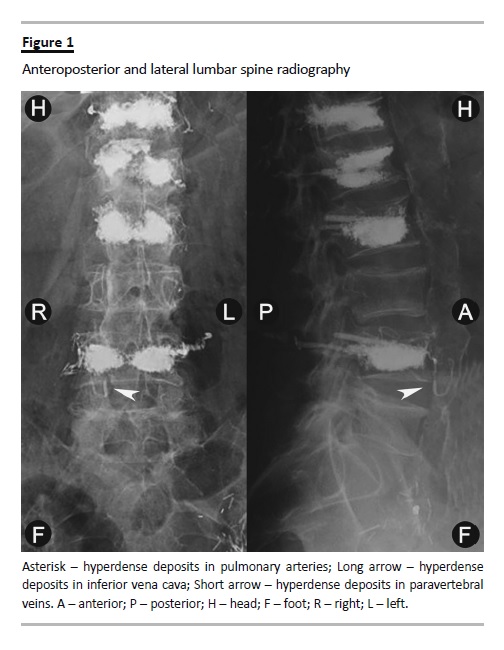
MBD linked to ESRD and steroid-induced osteoporosis with symptomatic vertebral compression fractures (VCFs) in D12-L4 section. To treat the chronic back pain, two-stage percutaneous balloon kyphoplasty (BKP) was performed. First, L1 and L2 cementation, 8 months before the current admission, and second, D12 and L4 vertebroplasty 7 months before current admission as fractures had extended to adjacent vertebrae (Fig. 1).
Other medical antecedents are: high blood pressure, gastrointestinal bleeding due to antral gastritis and oligosymptomatic biliary lithiasis. Diagnosis of cholecystitis and biliary sepsis was based on typical clinical and radiological findings.
Blood cultures performed by CVC dismiss the possibility of its infection. Empiric piperacillin-tazobactam antibiotic treatment was started at admission with consequent improvement in few days.
During the 2 weeks were detected peripheral oedema, pleural effusion, asthenia and minimal effort dyspnoea related to stage III CHF. NYHA functional class had not changed compared with previous weeks.
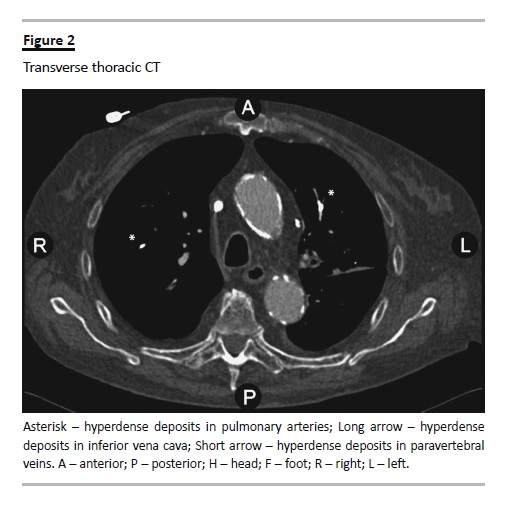
The thoraco-abdominal computed tomography (CT) performed for diagnosis revealed an unexpected presence of high-density deposits diffusely distributed in the pulmonary arteries (Fig. 2).
Despite the initial confusion due to the suspected relation between these radiological findings and preexisting low-grade respiratory insufficiency, other finds did unlikely the embolism as leading cause of dyspnoea. Arterial blood gas analysis showed low pH (7.32), low PaO2 (64 mmHg), high PaCO2 (52 mmHg), and normal HCO3 levels (26 mEq/L) diagnostic for hypoxemia with combined chronic respiratory and metabolic acidosis partially corrected by bicarbonate supply in dialysis. Progressive dry weight decrease led to better respiratory status at discharge without any other therapeutic actions. Presence of the same high-dense material in the paravertebral veins put in evidence the pathway of polymethyl methacrylate (PMMA) cement leakage to the pulmonary arteries (Fig. 3).
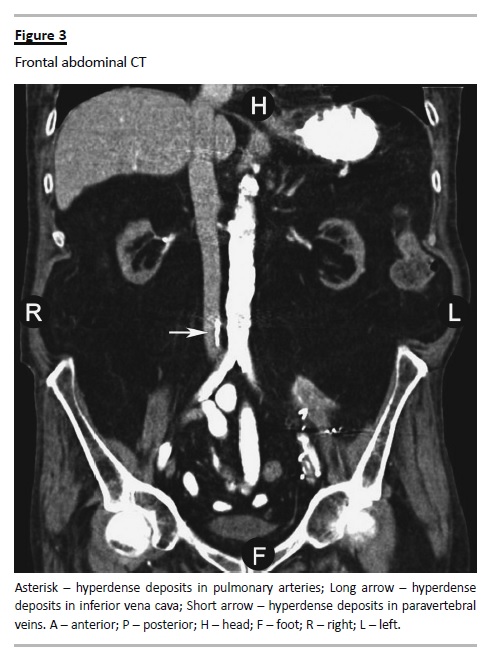
Diagnosis of late oligo-symptomatic PCE secondary to BKP was added.
Curiously, in spite of a large number of vertebral augmentation procedures (VAPs) annually performed in the world, this is the first report of PCE in a dialysis patient.
DISCUSSION
Vertebral fractures are an important health policy problem because they provoke kyphosis, chronic pain, impaired physical function, reduced quality of life, higher in-hospital attention rate and greater mortality risk1,2,3,4 Two large European studies describe about 12% incidence of VCFs in the general population5,6.
Furthermore, this prevalence is higher in some groups with metabolic illness, bone specific disorders or extended neoplasms. There is little evidence about their epidemiology in ESRD and only one publication of BKP in dialysis7. The recent Italian study EVERCRAFT appreciates a higher prevalence of VCFs in HD (55.3%) compared to the osteoporotic control group (51%), being in both, much greater than in the general population8.
This chronic degenerative disorder usually associates progressive, poorly controlled invalidating pain, which encourages an increased use of surgical interventions as vertebral cementation. Percutaneous vertebroplasty (PVP) using PMMA was first performed by Galibert et al., in 1984, to treat a painful, giant haemangioma9. Percutaneous BKP, applied since 1998, implies introduction of inflatable balloon into the fractured vertebral body for elevation of the endplates prior to bone cement fixation, thus allowing a lowest pressure injection of greater viscosity cement, with better results and potential decrease of postprocedure complications10,11. A recent small, randomized, controlled trial (RCT) compares a new selfexpanding implant cement directed kyphoplasty (CDK) to conventional PVP with promising reduction of extravertebral cement leak12.
The VAPs effectiveness has been strongly discussed after two RCTs published, in 2009, by Buchbinder et al.13 and Kallmes et al.14, but additional research upholds their plausibility3,4,15-18. Considering different points of view, the National Institute for Health and Clinical Excellence (NICE) issued, in April 2013, its appraisal guidance based on one of the most complete systematic reviews until now3,4. The NICEguidelines recommend VAPs like therapeutic optionin patients with recent, unhealed, well confirmedVCFs, who suffer uncontrolled pain despite optimal pain management3.
Potential mortality benefit in favour of VAPs remains controversial, although some sponsored studies suggest greater survival associated to better biomechanical stability16,19. Thereby, a powerful large observational study of 1,038,956 VCFs patients, where 141,343 BKP and 75,364 PVP were performed in 100% of US Medicare data set, showed 55% and 25% higher adjusted risk of mortality in a non-operated cohort compared to balloon kyphoplasty and percutaneous vertebroplasty cohorts, respectively (in both, p < 0.001). In this study, the BKP cohort had a 19% lower adjusted risk of mortality than the PVP cohort (p < 0.001)19.
Another controversial point is the cost-effectiveness of VAPs on account of small heterogeneous evidence concerning variable main objectives in all studies until now4,17.
Pain control is a primary goal in both modalities owing to accomplishment of a better quality of life.
One large clinical case series includes 868 VAPs performed during 12 years and shows successful results in 83% of vertebral tumours, 78% of osteoporotic VCFs and 73% of haemangiomas treated. Analgesic effect usually occurs within 6 to 48 hours after the procedure, with surprisingly low cement volume (average 2.8 ml)20. The factors involved in the analgesic mechanism of vertebral cementation are not clear. Initial suspicion of nerve-endings damage secondary to thermal and cytotoxic injury due to PMMA, reported by Deramond et al. after small in-vitro performed study, has not been confirmed uniformly later20-22.
A recent prospective in vivo study in 22 women with VCF does not observe statistically significant differences in their outcomes in spite of achievement of relevant temperature differences between the groups (average of 86.7° ± 10.7 °C in the highest group, 60.5° ± 3.7 °C in the medium and 44.8° ± 2.6°C in the lowest). Additionally, none of the eleven tested cements had maintained temperature superior to 45 ºC for more than 30 minutes (a minimal period of time needed to thermal injury of sensory nerves), with authors conclusion that back-pain improves only by mechanical consolidation22.
There are few contraindications as haemorrhagic diathesis, infection or epidural extended spine lesions, which may limit VAPs performance3,10. However, Table I numerous local or systemic adverse reactions linked to percutaneous vertebroplasty techniques may arise immediately or late in time (Table I)10,23-27.
The presentation of PCE ranges widely from asymptomatic radiologic findings to sudden death, even also respiratory distress, permanent pulmonary hypertension, severe lung failure, supraventricular arrhythmia or right heart failure23,28. Atypical and/or late clinical presentation of some symptoms, up to several years after the procedure, often makes difficult the diagnosis.
Typical radiological findings are several, radiodense, tubular opacities distributed diffusely in the branches of the pulmonary arteries, as well as shown in our patient.
The rate of PCE secondary to VAPs varies from 0% to 26% in published series with different follow-up periods and depends on cumulative risk of general, local and/or iatrogenic factors24-29. Like general risk factors are remarkable:
Chronic obstructive pulmonary disease
Pulmonary hypertension
Prior deep venous thrombosis.
Prior pulmonary embolism
The group of local risk factors includes:
Hypervascular tumoural VCFs
Numerous vertebroplasty procedures
Vertebral body wall incompetence
In last place, iatrogenic factors from PCE development are:
Low viscosity cement
Large volume of injected cement
Operator experience, and
Surgical technique performed (PVP vs. BKP)
Now, true delayed incidence of oligo- or asymptomatic PCE is difficult to know. Cement leakage incidence is more than 50% in some series (up to 90% in PVP and up to 37.5% in BKP) with estimated loss of injected volume around 22.9% in 10 years18,23,25,27,29.
The PCE treatment requires an individual approach and comprises from simple observation without any treatment to aggressive cardiovascular surgery, depending on the severity. Asymptomatic patients require only clinical and radiological observation but symptomatic cases usually need respiratory support, corticosteroids and standard anticoagulation for at least 6 months, according current guidelines23,28. Few severe cases with cardiopulmonary failure may require invasive respiratory support, removal of emboli by venous catheterization or cardiovascular surgery, or inferior vena cava filter implantation.
Our patient presented several risk factors, such as superior vena cava syndrome, prior pulmonary embolism and chronic heart failure due to heart transplant dysfunction. Six months after the diagnosis, his respiratory status remained stable, without need of additional treatment.
In our opinion, BKP is an excellent therapeutic option in selected dialysis patients, according to available recommendations.
References
1. Boonen S, Wahl DA, Nauroy L, et al. with the CSA Fracture Working Group of International Osteoporosis Foundation. Balloon kyphoplasty and vertebroplasty in the management of vertebral compression fractures. Osteoporos Int 2011; 22(12): 2915-2934. [ Links ]
2. Itshayek E, Miller P, Barzilay Y, et al. Vertebral augmentation in the treatment of vertebral compression fractures: review and new insights from recent studies. J Clin Neurosci 2012; 19(6): 786-791. [ Links ]
3. National Institute for Health and Care Excellence. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoportic vertebral compression fractures. NICE Technology Appraisal Guidance [TA279]. April 2013. Available at: http://www.nice.org.uk/guidance/ta279 [ Links ]
4. Stevenson M, Gomersall T, Lloyd Jones M, et al. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral fractures: a systematic review and cost-effectiveness analysis. Health Technol Assess 2014; 18(17) DOI 10.3310/hta18170. [ Links ]
5. ONeill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 1996; 11(7):1010-1018. [ Links ]
6. Felsenberg D, Silman AJ, Lunt M, et al. Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 2002; 17(4):716-724. [ Links ]
7. Demetriades A, Wong F, Ellamushi H, Afshar F, Yeh J. Balloon kyphoplasty treatment for a spontaneous vertebral fracture in renal osteodystrophy. BMJ Case Rep 2011; 2011 pii: bcr0220113890. [ Links ]
8. Fusaro M, Tripepi G, Noale M, et al. High prevalence of vertebral fractures assessed by quantitative morphometry in hemodialysis patients, strongly associated with vascular calcifications. Calcif Tissue Int 2013; 93(1): 39-47. [ Links ]
9. Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie 1987;33(2):166–168. [ Links ]
10. Eskey CJ. Vertebroplasty and Kyphoplasty: Indications and Techniques. In: Alfredo Quiñones-Hinojosa, ed. Schmidek and Sweet Operative Neurosurgical Techniques (6th edition). Philadelphia: W.B. Saunders: 2012;1973-1983. [ Links ]
11. Shi-Ming G, Wen-Juan L, Yun-Mei H, Yin-Sheng W, Mei-Ya H, Yan-Ping L. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for osteoporotic vertebral compression fracture: A metaanalysis. Indian J Orthop 2015; 49(4):377-387. [ Links ]
12. Vogl TJ, Pflugmacher R, Hierholzer J, et al. Cement directed kyphoplasty reduces cement leakage as compared with vertebroplasty: results of a controlled, randomized trial. Spine (Phila Pa 1976). 2013; 38(20):1730-1736. [ Links ]
13. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009; 361(6): 557-568. [ Links ]
14. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009; 361(6): 569-579. [ Links ]
15. Staples MP, Kallmes DF, Comstock BA, et al. Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: meta-analysis. BMJ 2011; 343:d3952. [ Links ]
16. Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the medicare population. J Bone Miner Res 2011; 26(7):1617-1626. [ Links ]
17. Borgström F, Beall DP, Berven S, et al. Health economic aspects of vertebral augmentation procedures. Osteoporos Int 2015; 26(4): 1239-1249. [ Links ]
18. Maestretti G, Sutter P, Monnard E, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J 2014; 23(6): 1354-1360. [ Links ]
19. Edidin AA, Ong KL, Lau E, Kurtz SM. Morbidity and mortality after vertebral fractures: Comparison of vertebral augmentation and nonoperative management in the Medicare population. Spine (Phila Pa 1976) 2015; 40(15): 1228-1241. [ Links ]
20. Gangi A, Guth S, Imbert JP, Marin H, Dietemann JL. Percutaneous vertebroplasty: indications, technique, and results. Radiographics 2003; 23(2):e10. [ Links ]
21. Deramond H, Wright NT, Belkoff SM. Temperature elevation caused by bone cement polymerization during vertebroplasty. Bone 1999; 25 (2 Suppl):17S-21S. [ Links ]
22. Anselmetti GC, Manca A, Kanika K, et al. Temperature measurement during polymerization of bone cement in percutaneous vertebroplasty: an in vivo study in humans. Cardiovasc Intervent Radiol 2009; 32(3):491-498. [ Links ]
23. Krueger A, Bliemel C, Zettl R, Ruchholtz S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J 2009; 18(9):1257-1265. [ Links ]
24. Wang E, Yi H, Wang M, Huang C. Treatment of osteoporotic vertebral compression fractures with percutaneous kyphoplasty: a report of 196 cases. Eur J Orthop Surg Traumatol 2013; 23 (Suppl 1):S71-75. [ Links ]
25. Pitton MB, Herber S, Koch U, Oberholzer K, Drees P, Düber C. CT-guided vertebroplasty: analysis of technical results, extraosseous cement leakages, and complications in 500 procedures. Eur Radiol 2008; 18(11):2568-2578. [ Links ]
26. Ren H, Shen Y, Zhang YZ, et al. Correlative factor analysis on the complications resulting from cement leakage after percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. J Spinal Disord Tech 2010; 23(7):e9-15. [ Links ]
27. Lee IJ, Choi AL, Yie MY, et al. CT evaluation of local leakage of bone cement after percutaneous kyphoplasty and vertebroplasty. Acta Radiol 2010; 51(6):649-654. [ Links ]
28. Wang LJ, Yang HL, Shi YX, Jiang WM, Chen L. Pulmonary cement embolism associated with percutaneous vertebroplasty or kyphoplasty: a systematic review. Orthop Surg 2012; 4(3):182-189. [ Links ]
29. Potet J, Weber-Donat G, Curis E, et al. Incidence of pulmonary cement embolism after real-time CT fluoroscopy-guided vertebroplasty. J Vasc Interv Radiol 2013; 24(12):1853-1860. [ Links ]
Dr. Vladimir Petkov Stoyanov
Department of Nephrology and Dialysis, Hospital Del Tajo
Av Amazonas Central s/n, c.p. 28300, Aranjuez, Madrid, Spain.
E-mail: vpetkov75@gmail.com
Disclosure of Potential Conflicts of Interest: None declared.
Received for publication: 21/09/2015
Accepted in revised form: 10/11/2015














