Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Portuguese Journal of Nephrology & Hypertension
Print version ISSN 0872-0169
Port J Nephrol Hypert vol.31 no.4 Lisboa Dec. 2017
ORIGINAL ARTICLE
Factors associated with early fistula failure: how to improve it
C. Belino1, S. Pereira1, A. Ventura1, V. Martins2, C. Nogueira2, JC. Fernandes1
1 Department of Nephrology, Centro Hospitalar de Vila Nova de Gaia e Espinho, Vila Nova de Gaia, Portugal
2 Department of Vascular Surgery, Centro Hospitalar de Vila Nova de Gaia e Espinho, Vila Nova de Gaia, Portugal
ABSTRACT
Introduction: Around the world, risk factors for fistula failure have been considered in vascular access planning in order to improve results. However, primary fistula failure rates seem to be increasing. Considering this, we conducted a study to identify relevant factors for early fistula failure in a Portuguese cohort with end-stage kidney disease. Subjects and Methods: Retrospective case-control study which included patients from a hospital center who underwent fistula construction between 2012 and 2015. Patients with fistula failure at 6 weeks were matched with consecutive controls in a proportion of 1:1. Clinical and laboratory data were retrieved. Multiple regression analysis was performed to identify factors associated with early complications. Results: Total of 100 predialysis patients with fistula failure at 6 weeks. Mean age of 67.7±11.9 years; most were women (n=54). Factors associated with overall risk of complications were distal location of fistula (OR 2.8; p<0.05) and diabetes mellitus (OR 3.8; p<0.05). Congestive heart failure (OR 7.2; p=0.06) was associated with a tendency for greater risk of inflow complications. Conclusions: In this cohort, despite improvements in vascular access planning, traditional risk factors still have a significant impact on fistula outcomes. The role of new factors is still undefined and further studies are needed. An adequate patient education, an organized vascular access program with nurses, nephrologists and surgeons with expertise, with systematic use of Doppler ultrasound, are key factors for better outcomes.
Key-Words: Uremia; risk factors; early fistula failure
INTRODUCTION
A well-functioning vascular access is essential for a proper dialysis. The native arteriovenous fistula (AVF) has proven to be the preferred choice, since it has longer primary patency rate, requires fewer interventions and is associated with the lowest incidence of morbidity and mortality. However, a major problem is the unpredictability of successful maturation1-4.
Around the world, traditional risk factors for fistula failure have been considered in vascular access planning in order to improve results. However, a recent meta-analysis that examined patency rates of AVFs in 62 cohorts published from 2000 to 2012 showed an increase in primary AVF failure rate (23%) comparing to the previous years (15%)5. Higher prevalence of female gender, distal fistula location and presence of diabetes mellitus are some factors suggested as possible contributors for this failure rate. Age or peripheral artery disease could not explain differences in AVF outcomes. Other important issues such as vessel diameter and quality, surgical expertise and differences in vascular access surgical training and facilities, which were not considered, may also have impacted on results. In fact, the authors highlighted the complexity around vascular access choice, evaluation and management. Different study definitions and methods are important limitations that need to be addressed in order to reach further valid conclusions.
Also, a clearer view of the potential new players in fistula maturation is necessary. New insights have shown that uremic state and use of antithrombotic agents may play a role in fistula maturation. Uremia stimulates neointimal hyperplasia and smooth muscle cells proliferation promoting vascular stenosis, so it has been hypothesized that a higher uremic milieu present in more advanced renal failure may negatively impact AFV outcomes6-8. The use of antithrombotic agents, such as aspirin, clopidogrel or warfarin has been associated with a reduction in early vascular stenosis and thrombosis with an important effect in modulation of the altered vascular biology3,6. It´s not clear if different etiologies of kidney disease, particularly diabetic kidney disease, would have influence in outcomes9.
Considering this, a study was conducted in a Portuguese cohort of patients who underwent AVF construction recently in order to identify factors associated with greater risk for primary failure.
SUBJECTS AND METHODS
Study setting and population
This was a retrospective case-control study designed to incorporate patients undergoing AVF construction between 1.1.2012 and 31.12.2015 in a single Portuguese center. All patients were predialysis patients.
Those who had a failure-to-mature fistula at 6 weeks after construction were matched with consecutive controls in a proportion of 1:1. Functional mature fistula was defined according to the NFK KDOQI 2006 vascular access guidelines. A failure-to-mature fistula was one with early complications which compromised its ability to be puncturable. Early complications were defined as inflow complications (arterial disease, stenotic lesions at or just beyond the anastomosis) or outflow complications (stenotic lesions in the venous segment).
Data collection
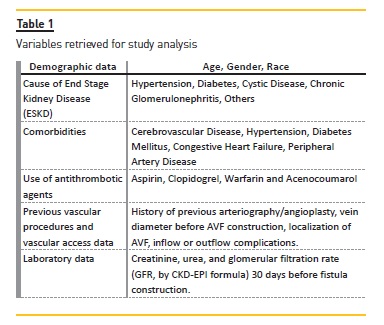
In our center, patients with advanced chronic kidney disease (stage 4 and 5) are referred to a vascular access consult to create a vascular access. This consultation is organized and performed by a multidisciplinary team (a nephrologist, a vascular surgeon and a specialized nurse). The same vascular surgeons who lead the consultation construct the fistulas. In a first observation, relevant clinical data concerning age, gender, race, primary renal disease, cardiovascular and metabolic co-morbidities, previous central catheters, cardiac and vascular interventions, presence of pacemaker, anticoagulation and antiplatelet use are recorded. Those data are incorporated with information obtained by Doppler ultrasound assessment of vasculature in order to guide the choice of AVF creation, with minimum vessel diameters of 2 mm. A second observation is made after 10 days of AVF construction to remove surgical suture and to confirm at least the presence of thill. A third observation is made after 6 weeks of construction to confirm adequate maturation. For those which failed to mature, we try to identify potential causes and how to manage them. Posterior interventions and re-evaluations are scheduled. All this information is recorded and available in a digital database, which was reviewed. Variables retrieved for study analysis are expressed in Table I.
Statistical analysis
Comparison of baseline characteristics between two groups was made with the chi-squared and Mann-Whitney tests. Multiple logistic regression analysis was used to identify significant predictors of early complications.
The following variables were categorized into analysis: age <65 years versus ≥65 years; diabetic versus nondiabetic kidney disease; creatinine <4.5 mg/dL versus ≥4.5 mg/dL; urea <150 mg/dl versus ≥150 mg/dL and GFR <15 ml/min/m2 versus ≥15 ml/min/m2.
RESULTS
Characteristics of patients
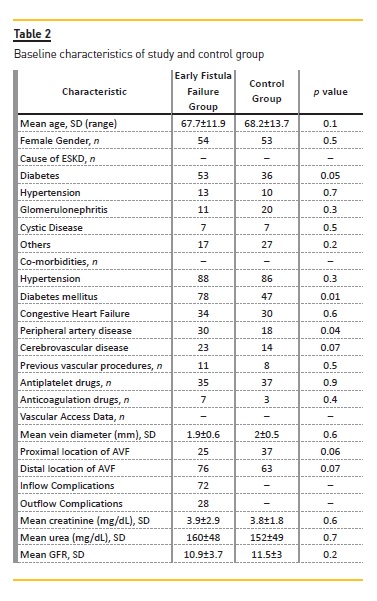
A total of 100 patients with fistula failure at 6 weeks were identified and matched (1:1). All patients were Caucasian. Global mean age was 67.9±12.8 [23; 90] years; most were female patients (n=105; 52.5%). Table 2 summarizes the main characteristics of groups.
Risk Factor for Poorer Outcomes
Factors associated with overall risk of complications were distal location of AVF (OR 2.8; p<0.05) and diabetes mellitus (OR 3.8; p<0.05). Antithrombotic agents were not associated with better results. When analysis was performed considering the type of complication, presence of congestive heart failure (OR 7.2; p=0.06) was associated with a tendency for greater risk of inflow complications. In this group of patients, the distribution of proximal (16 vs. 19) and distal (14 vs. 14) fistulas was similar between groups. No factor associated with risk of outflow complications was identified.
DISCUSSION
Understanding how to optimize the primary patency of fistulas is fundamental to improving survival and quality of life of patients1-3. Education and proper vascular access programs are pillars to obtain good results4,10.
The authors present a model of vascular access program which has allowed a reduction in central catheter use with increments in fistula number and patency rates in their center. Four steps have been identified in order to increase the rates of a functioning mature access: process of care (early education, vascular access team and timely surgery referral); preoperative evaluation; surgical strategy and monitoring programs10,11.
An education program must start in the early phases of chronic kidney disease and should be continuous, multidisciplinary, structured, and adjusted to patient goals and preferences11. Without proper information, patients are unable to make an informed decision regarding the dialysis access choice. In fact, patient knowledge and education can predict modality and vascular access choice. Low initial rates of AVF use reported in United States and Canada could be partially explained by poor knowledge of vascular access choices and lack of education during follow-up12. Predialysis educational programs performed by a multidisciplinary team (including a dedicated nephrologist and nurse) were associated with decreased mortality and longer time until dialysis initiation, which would give more time for fistula creation and maturation13,14. Vascular access education is also associated with increased fistula use at dialysis initiation11,12. The nephrologist should focus on the systematic and patient-level barriers in achieving a functional AVF, with emphasis on creation, maturation and cannulation that consider patient´s goals and preferences11. Information about the importance of vein preservation with prevention of injury to vessels used in AVF construction should be given. Written pamphlets can be of great use. Avoidance of PICCS (peripherally inserted central catheters) and subclavian catheters to minimize central vein stenosis and other complications must be outlined17.
Several entities have developed save my veins bracelets or medic-alert bracelet to remind patients and to alert health professionals11,12.
The creation of a successful vascular access team must also promote staff education and expertise. Nurses and vascular surgeons assume a central role in this part, since a deficit in skills in the area of assessment/cannulation and surgical construction can have devastating consequences10-13.
The preoperative evaluation is a cornerstone. The integration of patient and vascular characteristics allows defining the type of access and surgical strategies.
There are some factors that can´t be changed, such as patient comorbidities. Diabetes mellitus, congestive heart failure and distal localization of FAV were associated with risk for early complications in this study, which is consistent with current literature9,15.
Peripheral artery disease, which reflects vascular burden, was also significantly more frequent in early fistula failure group. This study wasn´t powered enough to detect if primary kidney disease or the use of antithrombotic agents can affect fistula outcomes. Some small studies16-22 showed encouraging results with use of aspirin, clopidogrel and dipyridamole, with beneficial effects on endothelium. Similarly, anticoagulant drugs may delay vascular occlusion, but is proven that they do not attenuate the pathophysiologic process, so adjunctive therapy is required. This study is also one of the first in vivo investigations trying to establish an association between uremia and early fistula failure.
The authors hoped that the obtained results could help to clarify the question about the better time to refer to AVF construction. A pro-mitogenic effect of uremia in human vascular smooth muscle cells was observed in a recent investigation performed by Aitken et al.6 with higher serum urea levels being related with poorer fistula outcomes. These results were not supported by our findings. Despite similar glomerular filtration rates, time of data collection was different (30 days versus 2 weeks before AVF construction) such as the medium urea levels, may be because of distinct laboratory methods of measurement. Also, the study presented by Aitken had many flaws and the authors assumed that there were many confounding issues.
Other factors like patient comorbidities, hemodynamics, vascular characteristics, surgical skills and vascular planning probably have had a superior impact in AFV maturation5,6,9.
Likewise, it is possible that other uremic toxins may play a more important role than urea. In fact, some authors have suggested that timing of access creation may be important to AVF outcomes but this point is not clear23-27. In DOPPs study23, longer time from referral to surgical evaluation or longer time from creation of vascular access to cannulation was associated with less probability of starting dialysis with a fistula. The UK renal Association recommends referral when patient is at kidney disease stage 4, considering primary disease and probable rate of decline. The guidelines from the Canadian Society of Nephrology are similar (creatinine clearance 15-20 ml/min/m2) and 2006 Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines suggest referral at least 6 months before the anticipated need for dialysis. In this cohort, managed by an organized program, FAV creation with lower glomerular filtration rates, reflecting a more advanced kidney disease, did not contribute to poorer outcomes.
Importantly, there are some disadvantages related with an earlier FAV construction, such as increased cardiovascular morbidity and mortality and adverse psychological factors9,11,12. Further studies are needed to clarify the right time of AVF construction.
Regarding all this, complex decisions are very common.
As an example, the benefits of a more proximal fistula in high risk patients must be balance with risk of complications like deleterious cardiac impact and steal syndrome, particularly in elderly2,9. Also, recent evidence has been shown that grafts or even central catheters may not be inferior to AVFs in fragile patients, patients with severe comorbidity burden or in the very elderly. Functional status, illness experiences, health priorities and life expectancy are fundamental issues to be considered28-30.
Several scores and predictive models of arteriovenous maturation are being developed in order to help reach more accurate decisions31-35. A recent trial about preoperative computer simulation for planning of vascular access surgery in hemodialysis patients is being conducted35. Noninvasive markers of endothelial function such as peripheral arterial tonometry (PAT), which provides a measure of pulse wave amplitude during reactive hyperemia, can also be used to estimate vascular health and predict outcomes36.
Using Doppler ultrasound for vascular territory assessment is a valuable tool and is probably underused.
This image technique is the only one that allows simultaneous visualization of vascular anatomy and its blood supply. Functional data can also be retrieved, like pulse wave velocity (PWV) and flow mediated dilatation (FMD) of the brachial artery. Pulse wave velocity reflects arterial stiffness and is an independent predictor of cardiovascular mortality. FMD is a measure of the change of brachial artery diameter in response to artery cuff occlusion and subsequent nitric oxide release, allowing the evaluation of macrovascular endothelial cell function36,37. This is also an exam that can be directly executed by the surgeon who will be creating the vascular access, and this is an important advantage.
International guidelines recommend its use in all AVF candidates31. However, this is a technique that is timeconsuming and requires an experienced examiner and special equipment. Effort must be made in training and education in this area31. Surgical technique also requires profound theoretical and practical knowledge. Avoidance of acute angles, hypotension and low blood flow can help to prevent early fistula failure11,34. Assisted maturation, which regards operative salvage techniques in early dysfunctional fistulas, plays an important role in achieving functional maturation and long-term patency, as an alternative or in conjunction with other minimally invasive procedures38. Referral to an experience center or centralization of the proceedings can help to overcome the gap in vascular access surgical expertise and facilities38.
The monitoring and surveillance program is critical for prevention of early failure and sustenance of longterm patency. There are a number of methods described in the literature: physical examination (PE); measurement of access blood flow (Qa); ratio intra access pressure/mean arterial pressure and recirculation rate, among others. Many of these methods have good accuracy to detect stenosis and have been shown to improve AVF patency10. A well-designed program should be able to detect early dysfunction and a close monitoring of the progression of a known stenosis or other vascular complication, allowing a timely referral for surgical or endovascular intervention16.
Nurses are key players in this program. Nephrologists who follow these patients should be proficient in the skills of VA monitoring. Any abnormality should make it necessary to maintain a close clinical monitoring or refer for another VA consultation for further assessment10.
Finally there are important limitations to this study. It is a relatively small cohort of patients, with data collected retrospectively and the results need to be validated in a large, prospective, multicenter analysis.
Patient data were taken from digital processes and there may have been a bias related to missing coded diagnostics. The study only includes vascular morphologic measures (vascular diameter). Furthermore, it did not consider all the factors proven to be associated with fistula maturation, which could have modified the obtained results.
CONCLUSIONS
Despite optimization of clinical and surgical issues surrounding AVF construction, traditional risk factors such as AFV distal location, diabetes mellitus and probably congestive heart failure still play a significant role in poorer outcomes in this cohort. The role of new factors is still undefined and further studies are needed.
An adequate patient education, an organized vascular access program with nurses, nephrologists and surgeons with expertise, with systematic use of Doppler ultrasound, are key factors for better outcomes.
References
1. Allon M, Robbin ML. Increasing arteriovenous fistulas in hemodialysis patients: problems and solutions. Kidney Int 2002; 62:1109. [ Links ]
2. Anel RL, Yevzlin AS, Ivanovich P. Vascular access and patient outcomes in hemodialysis: questions answered in recent literature. Artif Organs 2003; 27:237. [ Links ]
3. Smith G, Gohil R, Chetter I. Factors affecting the patency of arteriovenous fistulas for dialysis access. J VascSurg 2012; 55:3. [ Links ]
4. NKK-K/DOQI Clinical Practice Guidelines For Vascular Access: Update 2006. Guideline 8: Clinical outcome goals, 8.1 goals for access placement, 8.1.2 prevalent functional AVF placement rate. [ Links ]
5. Al-Jaishi AA, Oliver MJ, Thomas SM, Lok CE, Zhang JC, Garg AX, et al. Patency rates of the arteriovenous fistula for hemodialysis: a systematic review and meta-analysis. Am J Kidney Dis 2014; 63(3):464-478. [ Links ]
6. Aitken E, Jackson A, Kong C, Coats P, Kingsmore D. Renal function, uraemia and early arteriovenous fistula failure. Nephrology 2014, 15:179. [ Links ]
7. Vaziri ND, Pahl NM, Crum A, Norris K. Effect of uraemia on structure and function of immune system. J Ren Nutr 2012, 22(1):149-156. [ Links ]
8. Langer S, Paulus N, Yoeppel TA, Greiner A, Buhl A, Krombach GA, et al. Cardiovascular remodelling during arteriovenous fistula maturation in a rodent uraemia model. J Vasc Access 2011; 12(3):215-223. [ Links ]
9. Lily M, Lynch JR, Wish JB, Huff ED, Chen SC, Armistead NC, et al. Prevalence of arteriovenous fistulas in incident hemodialysis patients: correlation with patient factors that may be associated with maturation failure. Am J Kidney Dis 2012; 59(4):541-549. [ Links ]
10. Ventura A, Susana P. Focus on: the nephrologist´s role in arteriovenous fistulae monitoring and surveillance. Port J Nephrol Hypert 2015; 29(3):207-212. [ Links ]
11. Lomonte C, Basile C. Preoperative assessment and planning of haemodialysis vascular access. Clin Kidney J 2015; 8:278-228. [ Links ]
12. Moist LM, Al-Jaishi A. Preparation of the dialysis access in stages 4 and 5 CKD. Adv Chronic Kidney Dis 2016; 23(4): 270-227. [ Links ]
13. Lindberg JS, Husserl FE, Ross JL, et al. Impact of multidisciplinary, early renal education on vascular access placement. Nephrol News Issues 2005; 19(3):35-36. [ Links ]
14. Wu IW, Wnag SY, Hsu KH, et al. Multidisciplinary predialysis education decreases the incidence of dialysis and reduces mortality – a controlled cohort study based on the NFKDOQI guidelines. Nephrol Dial Transpl 2009; 24(11):3426-3433. [ Links ]
15. Basahr K, Zafar A, Elsheikh S, et al. Predictive parameters of arteriovenous fistula functional maturation in a population of patients with end-stage renal disease. PLoS One 2015; 10: e 0119958. [ Links ]
16. Jackson A, Coats P, Kingsmore D. Pharmacotherapy to improve outcomes in vascular access surgery: a review of current treatment strategies. Nephrol Dial Transplant 2012; 27:2005-2016. [ Links ]
17. Collaborative overview of randomized trials of antiplatelet therapy-II: maintenance of vascular graft or arterial patency by antiplatelet therapy. Antiplatelet Trialists Collaboration. BMJ A1994; 308:159-168. [ Links ]
18. Osborn G, Escofet X, Da Silva A. Medical adjuvant treatment to increase patency of arteriovenous fistulae and grafts. Cochrane Database Sys Rev 2088; 4:CD002786.
19. Taubert D, Berkels R, Schroder H, et al. Aspirin induces nitric oxide release form vascular endothelium: a novel mechanism of action. Br J Pharmacol 2004, 143:159-165. [ Links ]
20. Dember LM, Beck GJ, Allon M, et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: a randomized controlled trial. JAMA 2008; 299:2164-2171. [ Links ]
21. D´Alya M, Smith RM, Martone C, et al. The effect of systemic anticoagulation in patients undergoing angioaccess surgery. Ann VascSurg 2008; 22:11-15. [ Links ]
22. Crowther MA, Clase CM, Margetts PJ, et al. Low-intensity warfarin is ineffective for the prevention of PTFE graft failure in patients on hemodialysis: a randomized controlled trial. J Am SocNephrol 2001; 13:2331-2337. [ Links ]
23. Pisoni RL, Young EW, Dykstra DM, et al. Vascular access use in Europe and the United States: results from DOPPS. Kidney Int 2002; 61:305. [ Links ]
24. Basahr K, Zafar A, Elsheikh S, et al. Predictive parameters of arteriovenous fistula functional maturation in a population of patients with end-stage renal disease. PLoS One 2015; 10: e 0119958. [ Links ]
25. Avorn J, Winkelmayer WC, Bohn RL, et al. Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J ClinEpidemiol 2002 Jul;55(7):711-716. [ Links ]
26. O´Hare Am, Bertenthal D, Walter LC, Garag AX, Covinsky K, Kaufman JS, Rodriguez RA, Allon M. When to refer patients with chronic kidney disease for vascular access surgery: should age be a consideration? Kidney Int 2007, 71:555-561. [ Links ]
27. Lazarides MK, Georgiadis GS, Antoniou GA, Staramos DN. A meta-analysis of dialysis access outcome in elderly patients. J VascSurg 2007; 45:420-426. [ Links ]
28. Lomonte C, Forneris G, Gallieni M, Tazza L, Meola M, Lodi M, et al. The vascular access in the elderly: a position statement of the Vascular Access Working Group of the Italian Society of Nephrology. J Nephrol 2016; 29:175-184. [ Links ]
29. Allon M. Arteriovenous grafts: much maligned but in need of reconsideration? Semin Dial 2017; 30(2):125-133. [ Links ]
30. Allon M, Lee T. Reassessing recommendations for choice of vascular access. Clin J Am Soc Nephrol 2017; 12: 865-867. [ Links ]
31. Al Shakarchi J, McGrogan D, Van der Veer S, Sperrin M, Inston N. Predictive models for arteriovenous fístula maturation. J Vasc Access 2016; 17(3):229-232. [ Links ]
32. Lol CE, Allon M, Moist L, et al. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I). J Am SocNephrol 2006; 17:3204-3212. [ Links ]
33. Bosanquet D, Rubasingham J, Imam M, et al. Predicting outcomes in native AV forearm radio-cephalic fistulae; the CAVeA2T2 scoring system. J Vasc Access 2015; 16(1):19-25. [ Links ]
34. A. Masengu, MaxwllaP, Hanko JB. Investigating clinical predictors of arteriovenous fistula functional patency in a European cohort. CKJ 2015; 1-6. [ Links ]
35. Zonnebeld N, Huberts W, van Loon MM, Delhaas T, Tordoir JH. Preoperative computer simulation for planning of vascular access surgery in hemodialysis patients. J Vasc Access 2017;1 8(1):118-124. [ Links ]
36. MacRae JM, Ahmed S, Hemmelgarn B, Sun Y, Martin BJ, Roifman I, et al. Role of vascular function in predicting arteriovenous fistula outcomes: an observational pilot study. Can J Kidney Health Dis 2015; 2:19. [ Links ]
37. Zamboli P, Fiorini F, D`Amelio A, Fatuzzo P, Granata A. Color doppler ultrasound and arteriovenous fistulas for hemodialysis. J Ultrasound 2014; 17:253-263. [ Links ]
38. Kordzadeh A, Panayiotopolous YP. Algorithmic salvage techniques in non-maturing radiocephalic arteriovenous fistulae with their long-term patency. J Vasc Access 2017; 18(5):443-449. [ Links ]
Carolina Lã Belino, MD
Department of Nephrology, Hospital Center of Vila Nova de Gaia e Espinho
Rua Conceição Fernandes, 4434-502,Vila Nova de Gaia, Portugal.
E-mail: carolinabelino@hotmail.com
Disclosure of potential conflicts of interest: none declared.
Received for publication: Jul 24, 2017
Accepted in revised form: Oct 30, 2017














