Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.33 no.4 Lisboa dez. 2019
https://doi.org/10.32932/pjnh.2020.01.045
ORIGINAL ARTICLE
The Charlson Comorbidity Index – its impact on hospitalization and mortality in chronic renal disease
Luísa H. Pereira1, Filipa Mendes1, André Fragoso1, Ana P. Silva1,2, Pedro L. Neves1,2
1 Nephrology Department, Centro Hospitalar Universitário do Algarve, Faro, Portugal
2 Medicine and Biomedical Sciences Department, Algarves University, Faro, Portugal
ABSTRACT
Introduction: Renal replacement therapy has not always been shown to benefit end-stage renal failure patients who are elderly or have multiple comorbidities. The Charlson Comorbidity Index (CCI) predicts mortality and is frequently used for risk stratification in clinical practice. We evaluated correlation between the Charlson Comorbidity Index and hospital admissions and mortality in chronic kidney disease patients.
Methods: This retrospective observational study included 693 patients with an estimated glomerular filtration rate (eGFR)<30 ml/min/1.73m2, followed in pre-dialysis medical appointments (2008-2012). Based on the CCI, the subjects were collapsed into 4 risk groups: <25th percentile (CCI≤5.2; n=172) – G1; 25–50th percentile (CCI: 5.3–6.4; n=162) – G2; 50–75th percentile (CCI: 6.5–7.4; n=177) – G3; and >75th percentile (CCI≥7.5; n=182) – G4. Descriptive statistics, ANOVA, the chi-square and the log-rank tests were used for comparison between groups. The Bonferroni test was used as a post-hoc test. Kaplan-Meier analysis was used to evaluate mortality.
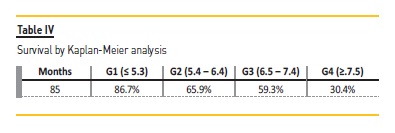
Results: Mean age was 70.1 years, 54% women, with an eGFR of 20.2±9.2 ml/min (Modification of Diet in Renal Disease). G1 patients were younger (p<0.001) and showed higher hemoglobin (p<0.001), eGFR (p=0.025), calcium (p=0.033) and albumin (p<0.001). In a multivariate logistic regression model adjusted for gender, age, hemoglobin, phosphorus, parathormone, eGFR, albumin and blood pressure, CCI is a risk factor for hospitalization (ORa=1.362, Cl 95% 1.175–1.580, p<0.0001). Multivariate Cox regression analysis identified higher scores of CCI as an independent risk factor for cardiovascular mortality (HRa=1.24, Cl 95% 1.053–1.467, p=0.010). Survival at 85 months was progressively shorter with higher CCI (G1=86.7%, G2=65.9%, G3=59.35 % and G4=30.4%, log-rank=34.465, p=0.0001).
Conclusion: The Charlson Comorbidity Index was shown to be a strong predictor of mortality and hospitalizations in patients with stage IV chronic kidney disease. It might be a valuable tool in dialysis decision-making for patients with advanced chronic kidney disease and severe comorbidity burden.
Key-Words: Charlson Comorbidity Index; Chronic Kidney Disease; Comorbidities; Elderly; Survival.
INTRODUCTION
Nowadays, as people age and live longer, they are more likely to develop several comorbid conditions, including chronic kidney disease (CKD)1,2,3. About 60% of deaths worldwide are related to chronic diseases and this number is expected to rise by 15% by 20204. Plus, CKD is the 15th and 20th cause of years lived with disability5 and disability-adjusted life years6.
Khan defined comorbidity in kidney failure patients as a significant concurrent or past disease in addition to CKD, which involved organs other than the kidneys but which may also be responsible for the renal failure2.
Risk factors predicting either increased morbidity or mortality among dialysis patients have been well described by earlier research, but are poorly defined in the pre-dialysis population7. Population ageing has conditioned a progressive increase of very old, dependent and frail patients on dialysis8. These patients present multiple comorbidities that worsen prognosis and have a negative impact on their quality of life, since it had been shown that comorbidities tend to worsen after dialysis initiation, as does patients functional status. Estimated life expectancy for these patients, even with renal replacement therapy (RRT), has been quoted to be as low as 8 months1,9,10. According to the Portuguese Society of Nephrology Registry, in Portugal, 60.2% of incident dialysis patients in 2018 were over 65 years and the mean age of prevalent patients was 67.2 years11. Age per se is a strong predictor of mortality and the mortality rate is considerably higher for elderly patients on dialysis than those who are not10. Additionally, for elderly end stage renal disease (ESRD) patients, prompt RRT is costly and does not necessarily extend survival12.
These older patients who are initiated on dialysis require more medical interventions (including dialysis) and are more commonly hospitalized than those treated conservatively13. Given the rapid growth of elderly populations, it is necessary to adopt practical and useful tools to make mortality prediction easier. Assessment of the overall comorbidities may be helpful to identify those patients whose condition will probably evolve poorly.
The CCI score, a method that measures burden of disease, has proven to correlate well with survival and has been validated in ESRD patients14,15. It is divided into four groups according to score: low (<3 points), moderate (4–5 points), high (6–7 points) and very high (≥8 points)10,16.
The higher number of comorbid conditions in chronic dialysis patients is associated with an increased mortality risk, which may range from 20% to almost 60%, as compared to chronic dialysis patients without comorbidity2. The survival probability will be lower with higher scoreswith a score ≥8, the 12 and 24 month survival probability is 64% and 35%, respectively10,16.
The CCI is the most frequently used tool to measure co-existing diseases, and it has been validated for predicting the risk of mortality, disability, hospitalization and length of hospital stay in various clinical settings17.
Identification of factors that modify the strength of the relationship between CKD and adverse outcomes may improve the current understanding of how impaired kidney function leads to higher morbidity and mortality18.
Furthermore, the CCI might be a valuable tool regarding dialysis decision making for patients with advanced CKD and severe comorbidity burden, frequently with cognitive impairment and who might benefit from conservative care, centered on quality of life19.
In this study we evaluated the correlation between the CCI and hospital admissions in patients with CKD and the influence of the CCI on their mortality.
SUBJECTS AND METHODS
Study design and participants
We included in a retrospective observational study 693 patients, with an eGFR <30 ml/min/1.73m2, followed in a pre-dialysis clinic between January 2008 and December 2012.
The results were obtained through consultation of clinical processes, with written agreement of the patients and authorized by the Ethics Committee from the University Hospital Centre of Algarve – Faro Unit. By consulting electronic clinical processes we were able to obtain data referring to demographic characteristics, underlying disease, date of diagnosis, laboratory and imaging studies and hospitalizations from the beginning of follow up in low-clearance appointment until dialysis start or patient death. Comorbidity was assessed by the Charlson Comorbidity Index20, on the first visit, adjusted for age at time of follow-up.
Hospitalizations
The evaluation and characterization of hospitalizations was based on the hospital admission clinical record, which provides information on signs and symptoms, diagnostic exams, procedures, treatments and diagnosis on the day of discharge.
Mortality
Deaths were confirmed by review of autopsy reports, death certificates, medical records or information obtained from next of kin or family members and classified, according to its cause, as cardiovascular or non-cardiovascular death. Cardiovascular deaths were defined as mortality caused by coronary heart disease, heart failure, peripheral vascular disease and cerebrovascular disease.
Statistical analyses
Statistical analysis was performed with SPSS (version 23.0). Quantitative results were expressed as mean ± standard deviation (SD) for continuous variables with normal distribution, using the Kolmogorov-Smirnov test. Categorical variables were compared using the chi-square test. Based on the CCI, the subjects were collapsed into 4 risk groups according to the following criteria: <25th percentile (CCI≤5.2; n=172) – G1; 25–50th percentile (CCI: 5.3–6.4; n=162) – G2; 50–75th percentile (CCI: 6.5–7.4; n=177) – G3; and >75th percentile (CCI≥7.5; n=182) – G4.
For comparison between groups we used analysis of variance (ANOVA) and for post hoc analysis, the Bonferroni test. The multivariable logistic regression models were used to assess predictive factors for hospitalization. The exponentials of the model parameters were the adjusted odds ratio (ORa) to other variables of the model, with 95% confidence interval.
The Kaplan-Meier method for measuring patient survival rate was applied and a comparison between the four percentiles was based on the log-rank test. The risk factors and their hazard ratio (HRa) were calculated and a multivariate Cox regression was used to find out predictors of cardiovascular mortality.
RESULTS
Patients mean age (±SD) was 70.1±12.5 years; 53.4% (n=371) were women and 46.5% (n=322) men. Median eGFR (MDRD) was 18.5 mL/min/1.73 m2. Mean CCI obtained in individual patients was 6.4±1.8. Table Ishows the distribution of CCI score.
There was a homogeneous distribution, G1 with 172 individuals (64.5 % women and 35.5% men), G2 with 162 individuals (50% women and 50% men), G3 with 177 individuals (42.9% women and 57.1% men) and, G4 with 182 individuals (56.6% women and 43.4% men) (Table I).
Older patients were more likely to be in the higher CCI score groups. Median systolic blood pressure found in these groups was 136.4±14.9 mmHg and mean hemoglobin 11.57±1.12g/dL.
Albumin and cholesterol mean values were 3.97±0.46 g/dL and 180.8±45 mg/dL, respectively. We found high mineral metabolism parameters, PTH (parathyroid hormone) =238±185.37 pg/mL, phosphorus=4.06±0.75 mg/dL and calcium=9.25±0.67 mg/dL.
As seen in Table I, we found significant differences between groups, with G1 patients younger (p<0.001) having a higher hemoglobin (p<0.001), eGFR (p=0.025), calcium (p=0.033) and albumin (p<0.001). For the remaining values, namely cholesterol, PTH and phosphorus, there was no significant variations between groups, with a p> 0.05. (Table I)
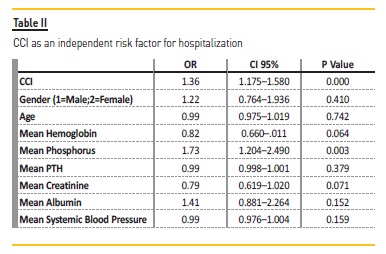
CCI as an independent risk factor for hospitalization
Multivariate logistic regression analysis was performed to identify independent risk factors associated with hospitalization. This model was adjusted for CCI, gender, age, hemoglobin, phosphorus, PTH, creatinine, albumin, and blood pressure.
The results show that higher levels of CCI are an independent risk factor for hospitalization (ORa=1.362, Cl 95% 1.175-1.580, p<0.0001), as well as phosphorus (ORa=1.73; Cl 95% 1.204–2.490, p=0.003) (ORa=2.039, p=0.005) (Table II).
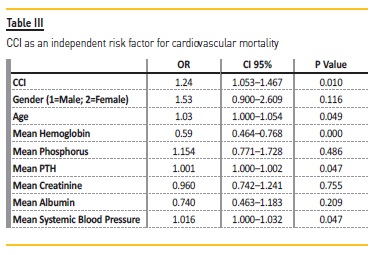
CCI as an independent risk factor for death
During the follow-up period (mean duration 40.8±8.6 months), 125 patients died due to cardiovascular events.
Multivariate Cox regression analyses clearly identifies higher scores of CCI as an independent risk factor for cardiovascular mortality (HRa=1.24, Cl 95% 1.053–1.467, p=0.010) (Table III). Also, low levels of hemoglobin (HRa=0.59, Cl 95% 0.464–0.768, p=0.0001) and increased levels of PTH (HRa=1.001, CI 95% 1.000–1.002, p=0.047) and blood pressure (HRa=1.016, CI 95%1.000–1.032, p=0.047) had greater hazard ratio for cardiovascular mortality (Table III).
Univariate logistic regression showed that G4 (OR=7.516; CI 95% 3.280–17.218; p=0.000) has a greater risk of death than G1, followed by G2 (OR=3.320; CI 95% 1.364–8.080; p=0.008) and subsequently by G3 (OR=2.668; CI 95%1.085–6.562; p=0.033). Table IV and Figure 1 shows a progressively shorter survival at 85 months with higher CCI. Log-rank analysis was 34.463 with a p value of 0.000.
DISCUSSION
Risk stratification scores based on age, functional status, comorbidity and early versus late referral to dialysis have been proposed for elderly patients. Because dialysis does not always enhance survival in elderly patients, distinguishing the patients with poor prognosis before dialysis start is important.
The present study has identified, in a 693 patient population, CKD stage IV, baseline demographic, clinical and biochemical predictors of adverse outcome among a retrospective cohort of pre-dialysis patients. We showed that high CCI levels are an independent risk factor for hospitalization and cardiovascular mortality. A higher number of comorbid conditions in CKD pre-dialysis patients is associated with an increased risk of mortality, as shown by univariate logistic regression: G4 had a higher risk of death than G1 and the other groups.
Additionally, survival time was dramatically decreased in patients with CCI ≥7.5 (G4) regardless of age: 30.4% (G4) vs 86.7% (G1). ESRD is becoming an increasingly geriatric condition and the option for nondialytic management is increasingly recognized and delivered21.
This index requires 15 minutes (often less) to complete and the metric is easy to use. It can instantly supply information that might be used by a clinician to make the decision of initiating dialysis or not, a rising dilemma in our daily practice.
Di Iorio et al.22 reported that the crude mortality rate increased by approximately 60% of patient-years across incident hemodialysis patients when the CCI score was 6 in contrast to a CCI score of 3.
The mortality rate within CKD population using renal replacement technique is about 16 to 22%, which is considered by the literature to be very high. More than half of these deaths are related to cardiovascular disease15,23.
For a selected group of elderly patients with a heavy burden of comorbid illness, although dialysis may be technically feasible, the short-term mortality is often very high, particularly in those with advanced cardiovascular disease and/or diabetes24. In our study, during the follow-up period, 125 patients died due to cardiovascular events, representing 18% of the study population.
This probably should make us reconsider starting RRT on these patients. Morbidity may be increased by additional burdens imposed by dialysis, such as time spent on dialysis itself, transportation to and from dialysis units, loss of autonomy, neurological impairment, complications of the vascular access (mainly infection), pain and hospitalization days. Although patients may live longer with dialysis, the extension of lifetime may be associated with poor quality of life and degradation of their basal state10,21.
Some studies have demonstrated that the survival of elderly patients on dialysis may actually be considerably reduced, compared to that of the non-dialysis population of the same age25,26. Most patients with CKD have at least one comorbidity. A quarter of the patients, however, may present 3 or more comorbidities and 7% have 5 or more27.
Through the results obtained in our study, we can advance that the presence of comorbidities increases hospitalizations occurrence and, additionally, the more comorbidities presented by a CKD patient (higher CCI), the greater the hospitalization risk will be. The same is valid when we analyze the survival by Kaplan-Meier analysis (Table IV and Figure 1), since it will be progressively lower, the higher the CCI.
Tonelli et al.28 found that the risk attributed to hospitalizations was greater for diabetes, hypertension, myocardial infarction, cardiac insufficiency, chronic lung disease, lymphoma, and cancer, among others. Plus, according to Mix et al.29, among 1000 CKD patients at risk, 134 required hospitalization, with most of these hospitalizations caused by CKD-associated comorbidities26.
Our study indicated that higher CCI might be able to predict survival in incident dialysis patients and could therefore be used for risk stratification in clinical practice.
This study has several limitations. Information about factors such as smoking and functional impairment, which may affect survival, was not available. However, as with all studies that use datasets, the key comorbid conditions that contribute additionally to prognostic information besides laboratory and clinical parameters were reported.
Another limitation is that the CCI score was only obtained at baseline. Since comorbidity must have changed in some patients over time, this might have affected our results.
We considered that the inclusion of a larger sample, more variables such as ethnicity and a greater variety of CKD stages population could be important to provide more data.
In conclusion, in this study, the CCI was shown to be a strong predictor of mortality and hospitalizations in patients with stage IV CKD.
Nowadays, identifying the ideal patient for conservative treatment and how to approach and manage care are issues of great debate. Our findings can help to stratify the risks of starting dialysis in elderly patient populations and are informative for the dialysis decisionmaking process. Conservative treatment might be considered for ESRD patients with multiple comorbidities and low survival rates, since treatment aims for patients with ESRD are not only to prolong life, but also to achieve the greatest possible well-being and function.
References
1. Ng YY, Hung YN, Wu SC, Ko PJ, Hwang SM. Progression in comorbidity before hemodialysis initiation is a valuable predictor of survival in incident patients. Nephrol Dial Transplant. 2013;28(4):1005-1012. doi:10.1093/ndt/gfs512. [ Links ]
2. Rattanasompattikul M, Feroze U, Molnar MZ, et al. Charlson comorbidity score is a strong predictor of mortality in hemodialysis patients. Int Urol Nephrol. 2012;44(6):1813-1823. doi: 10.1007/s11255-011-0085-9. [ Links ]
3. Jesky M, Lambert A, Burden ACF, Cockwell P. The impact of chronic kidney disease and cardiovascular comorbidity on mortality in a multiethnic population: a retrospective cohort study. BMJ Open. 2013;3(12):e003458. doi: 10.1136/bmjopen-2013-003458. [ Links ]
4. Hazzan AD, Halinski C, Agoritsas S, Fishbane S, DeVita MV. Epidemiology and challenges to the management of advanced CKD. Adv Chronic Kidney Dis. 2016;23(4):217-221. doi:10.1053/j.ackd.2016.04.005. [ Links ]
5. Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743-800. doi:10.1016/S0140-6736(15)60692-4. [ Links ]
6. Manuscript A. Europe PMC Funders Group Europe PMC Funders Author Manuscripts Europe PMC Funders Author Manuscripts Global, regional, and national disability-adjusted life years ( DALYs ) for 306 diseases and injuries and healthy life expectancy ( HALE ) for 188 count. Lancet. 2016;386(10009):2145-2191. doi:10.1016/S0140-6736(15)61340-X.Global. [ Links ]
7. Holland DC, Lam M. Predictors of hospitalization and death among pre-dialysis patients: a retrospective cohort study. Nephrol Dial Transplant. 2000;15(5):650-658. doi: 10.1093/ndt/15.5.650. [ Links ]
8. Shum CK, Tam KF, Chak WL, Chan TC, Mak YF, Chau KF. Outcomes in older adults with stage 5 chronic kidney disease: comparison of peritoneal dialysis and conservative management. Journals Gerontol - Ser A Biol Sci Med Sci. 2014;69 A(3):308-314. doi:10.1093/gerona/glt098. [ Links ]
9. Seow YY, Cheung YB, Qu LM, Yee ACP. Trajectory of quality of life for poor prognosis stage 5D chronic kidney disease with and without dialysis. Am J Nephrol. 2013;37(3):231-238.doi:10.1159/000347220. [ Links ]
10. Bento C, Fructuoso M, Costa R, Castro R, Morgado T. Very elderly patients on haemodialysis: evolution and its relation with comorbidities. Port J Nephrol Hypertens. 2014;28(4):325-329. http://www.scielo.mec.pt/pdf/nep/v28n4/28n4a08.pdf. [ Links ]
11. Portuguese Registry of Dialysis and Transplantation 2018; Available at http://www.bbg01.com/cdn/rsc/spnefro/gabreg/305/RelatriosAnuais2018.pdf. Accessed December 14, 2019. [ Links ]
12. Lin YT, Wu PH, Kuo MC, et al. High Cost and low survival rate in high comorbidity incident elderly hemodialysis patients. PLoS One. 2013;8(9):1-8. doi:10.1371/journal.pone.0075318. [ Links ]
13. Schell AJO, Arnold RM. Conservative care of end stage renal disease. 2019:1-18.
14. Hall SF. A users guide to selecting a comorbidity index for clinical research. J Clin Epidemiol. 2006;59(8):849-855. doi:10.1016/j.jclinepi.2005.11.013. [ Links ]
15. Van Manen JG, Korevaar JC, Dekker FW, Boeschoten EW, Bossuyt PMM, Krediet RT. How to adjust for comorbidity in survival studies in ESRD patients: a comparison of different indices. Am J Kidney Dis. 2002;40(1):82-89. doi: 10.1053/ajkd.2002.33916. [ Links ]
16. Quan H, Li B, Couris CM, et al. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676-682. doi: 10.1093/aje/kwq433. [ Links ]
17. Lin Y, Yang C, Chu H, et al. Association between the Charlson Comorbidity Index and the risk of 30-day unplanned readmission in patients receiving maintenance dialysis. BMC Nephrol. 2019;20(1):1-8. doi: 10.1186/s12882-019-1538-0. [ Links ]
18. Tonelli M. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17(7):2034-2047. doi:10.1681/ASN.2005101085. [ Links ]
19. Scott J, Owen-Smith A, Tonkin-Crine S, et al. Decision-making for people with dementia and advanced kidney disease: a secondary qualitative analysis of interviews from the Conservative Kidney Management Assessment of Practice Patterns Study. BMJ Open. 2018;8(11). doi: 10.1136/bmjopen-2018-022385. [ Links ]
20. Indice de Comorbilidad de Charlson (CCI). http://www.samiuc.es/index.php/calculadores-medicos/calculadores-de-evaluadores-pronosticos/indice-de-comorbilidad-de-charlson-cci.html. [ Links ]
21. Belino C, Meng C, Neto R, Gonçalves E, Pestana M. Supportive care in advanced chronic kidney disease: comprehensive conservative care. Port J Nephrol Hypertens. 2018;32(2):149-158. [ Links ]
22. Di Iorio B, Cillo N, Cirillo M, Gaspare De Santo N. Charlson Comorbidity Index is a predictor of outcomes in incident hemodialysis patients and correlates with phase angle and hospitalization. Int J Artif Organs. 2004;27(4):330-336. doi: 10.1177/039139880402700409. [ Links ]
23. Silva AP, Fragoso A, Pinho A, et al. Phosphorus as an early marker of morbidity and mortality in type 2 chronic kidney disease diabetic patients. J Diabetes Complications. 2013;27(4):328-332. doi: 10.1016/j.jdiacomp.2013.02.007. [ Links ]
24. Carson RC, Juszczak M, Davenport A, Burns A. Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol. 2009;4(10):1611-1619. doi: 10.2215/CJN.00510109. [ Links ]
25. OHare AM, Choi AI, Bertenthal D, et al. Age affects outcomes in chronic kidney disease. J Am Soc Nephrol. 2007;18(10):2758-2765. doi: 10.1681/ASN.2007040422. [ Links ]
26. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296-1305. doi: 10.1056/NEJMoa041031. [ Links ]
27. Palmer SC. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals With chronic kidney disease. Jama. 2011;305(11):1119. doi: 10.1001/jama.2011.308. [ Links ]
28. Tonelli M, Curhan G, Pfeffer M, et al. Relation between alkaline phosphatase, serum phosphate, and all-cause or cardiovascular mortality. Circulation. 2009;120(18):1784-1792. doi: 10.1161/CIRCULATIONAHA.109.851873. [ Links ]
29. Mix TCH, St. Peter WL, Ebben J, et al. Hospitalization during advancing chronic kidney disease. Am J Kidney Dis. 2003;42(5):972-981. doi: 10.1016/j.ajkd.2003.06.001. [ Links ]
Luísa Helena Olim Ribeiro Pereira
Avenida da Madalena, ed. Século XXI, nº 73, 2ºI,
9020-330, Funchal, Madeira, Portugal
Email: luisahelenapereira91@gmail.com
Disclosure of potential conflicts of interest: none declared
Received for publication: Dec 1, 2019
Accepted in revised form: Dec 31, 2019














