LETTER OF RESEARCH
Patients with chronic kidney disease (CKD) are at risk of cardiovascular (CV) disease and increased CV mortality1. Cardiac structure is altered in CKD patients, and it is known that one-third of patients will present with left ventricular hypertrophy (LVH), a prevalence that rises to 70-80% in CKD stage 5 patients2. Hemodynamic changes, increased systemic blood pressure, and altered mineral metabolism contribute to this phenomenon, namely abnormally high levels of FGF233.
Long-term outcomes in kidney transplantation have improved over the last decades, and CV disease and fractures have emerged as importante events in transplanted patients4. Cardiovascular disease is the leading cause of death after renal transplantation, with these patients at twice the risk of death of the general population5.
Based on a prospective study of a cohort of 84 patients admitted to renal transplantation who agreed to participate in a bone and CV health-related study (ClinicalTrials.gov ID NCT02751099)6, we performed a case-control analysis to evaluate if transplantation would impact on the echocardiographic assessment (with the reduction of uremic toxics, namely FGF23), comparing 1-year of transplantation with maintenance in the waiting list. Recruitment of patients (the cases) was performed on the day the patient was called for transplant (excluding patients under 18 years old, admitted to double transplantation, with intellectual disability, and who did not consent to take part in the study) and these patients were followed over a period of 12 months.
At the end of the first year of transplantation, 69 patients continued in the study (6 refused to remain in the study; 5 had primary nonfunction of the graft and were excluded, and 4 patients died). These 69 patients were paired for age, sex, dialysis vintage, presence of diabetes, and hypertension with a dialysis population listed for kidney transplantation at our unit (controls) on a 1-to-1 basis. We compared the evolution of left ventricular mass index (LVMI) and presence of LVH in both populations: in the case cohort at baseline and after 1-year of transplant; in the control cohort we evaluated the last echocardiogram performed while on the waiting list and the one performed the year before. Echocardiograms were performed in M mode and 2D to access LVH (calculated using the Devereux formula, indexed to body surface area). LVH was defined as LVMI > 95 g/m2 in women and >115 g/m2 in men. The institutions’ local ethics committees and the National Committee for Data Protection approved data collection and treatment.
We found no statistical difference between the demographic characteristics of both populations, in line with our expectations. Although LVMI was similar in both populations, we found a significant difference in the presence of LVH if we added 12 months of dialysis in a patient that otherwise could be submitted to transplant, as shown in Table 1.
Table 1 Comparisons of two cohorts: transplanted cohort (cases) and the dialysis cohort (controls)
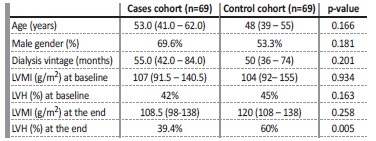
Statistical analysis: Wilcoxon rank-sum test. LVMI - left ventricular mass index; LVH - left ventricular hypertrophy
Nevertheless, there are limitations to this evaluation: this is na observational, unicentric study, with a reduced sample of patients. Another limitation is the fact that different operators performed the echocardiograms, and we should acknowledge that 12 months is a brief period to observe major differences in echocardiographic findings.
Other studies have shown that LVH is present in a very expressive portion of renal transplanted persons7, as it was in our population, where 42% had LVH. Even so, we could find a reduced of its percentage after 1-year of transplant, which we did not find in waiting list patients.
Although a 12-month period is very short to observe long-term modifications in cardiac structure, we found that LVH was reduced after 1-year of transplantation, reinforcing the benefits of transplantation in CKD patients.















