INTRODUCTION
The expenses with the replacement treatment of renal function (RTRF), in particular dialysis, are very high and can determine, in some countries, limits to its use and development. This is not the case in Portugal where all chronic kidney patients in need have free and universal access to treatment.
However, as Portugal has an extremely high incidence in dialysis and, on other hand, as many other expenses in the national Public Health Sector are also a priority, it is important to analyze which factors, in this context of the RTRF, have a greater influence in general health expenditures.
With this objective in mind, the main intervening factors are analyzed - price of dialysis treatment and prevalence in dialysis. The influence of its values and its evolution over the last few years on state expenditure is evaluated. Possible measures for correction are suggested.
DISCUSSION
Margaret Chan, Director-General of the World Health Organization, and many other scientists, in particular epidemiologists, have been insisting on the need for chronic kidney disease, and its prevention and treatment, to be considered worldwide as a public health problema due to the enormous repercussion it has at the human, family, social and economic level.
The enormous expenses inherent to the substitutive treatment of chronic kidney disease - dialysis and kidney transplantation - can reduce the state’s ability to intervene in a more effective way, such as the implementation and availability of adequate and effective measures to prevent chronic kidney disease and its progression.
Maintaining a continuous and informed analysis of the expenses involved in renal function replacement therapies should be a concern of the responsible entities. National dialysis expenses depend mainly on two factors:
1. The price of dialysis treatment
2. The number of patients undergoing dialysis (dialysis prevalence).
In Portugal, until 2008, payment was made for each dialysis treatment performed.
From this date, with the implementation of the Integrated Management of Chronic Kidney Disease model,1 it was decided to implemente a new type of payment, capitation type, which was given the name of comprehensive price (CP). The original idea of switching to a bundl reimbursement was, without any doubt, useful and appropriate.
As mentioned by Escoval and collaborators2 regarding the decision to implement the comprehensive price “the magnitude of the problem, in terms of public health, requires the adoption of a directed, targeted, planned and integrated action, based on clear and well-defined strategies in order to obtain health gains, improving the quality of care and streamlining the costs“.
However, it would have been important to take into account what various international organizations recommend. For example, the European Kidney Health Alliance (aliance of non-profit organizations) recommends: “Reimbursement treatment should be based on na accurate estimation of the total direct and indirect costs of CKD and its treatment”, and “if bundling of reimbursement is considered, the clinical consequences should be carefully considered and checked to avoid counterproductive effects”.3
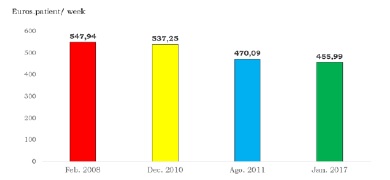
The CP value, identical for any of the techniques - hemodialysis and peritoneal dialysis - and for the public or private sector - had na initial value of 547.94 euros per patient and per week.
The CP only included part of the expenses4: three of the six, which comprise total patient care: dialysis treatment, medicines (a list has been published), and clinical diagnostic tests (a list has also been published). It did not include vascular access, hospital admission and transport.
A CP of equal value for the public and private sector seems to be completely inappropriate since the expense in the first is much higher: 1. More severe patients with multiple co-morbidities. 2. All installed capacity cannot be used as it has to receive patients with complications from the private sector. 3. The number of doctors, nurses and auxiliary staff in a public unit must be much higher.
In the two following years, after the implementation of the CP, it was found that the annual expense with dialysis had increased by more than 30% in relation to previous years. This change was not attributable to the increase in the number of patients on dialysis.
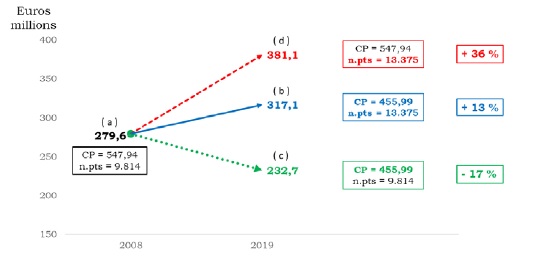
Over the last few years, the government has determined a successive reduction in CP values (Fig. 1), setting in 2018, retroactively to January 2017, the value of 455.99 euros/patient/week (euro-pt/wk).
Some other elements were also included in the CP (vascular access and blood transfusions).
The impact on annual expenditure on dialysis at the national level, observed in 2019 (13 375 patients), resulting from the decrease in the CP value, from 547.94 (euro-pt/wk) in 2008 to 455.99 (euro-pt/wk), was approximately 64 million euros.
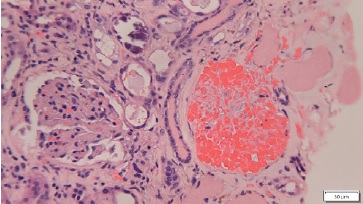
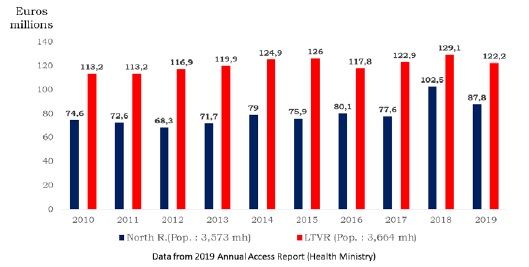
It is also known, that the private hemodialysis sector (peritoneal dialysis in Portugal is only performed in the public sector) - which represents more than 90% of all hemodialysis treatments performed in the country - is today the sector that bears the greatest burdens of the private health sector directly dependent on payment by the state (46% in 2010 and 61% in 2018) (Fig. 2).
All these data demonstrate how important it is to maintain a permanente and updated observation in this area. What we can now admit is that since the costs of dialysis supplies, drugs and diagnostic tests have likely not dropped over the years, it is more likely that the data used to calculate the CP value was wrong. However, it must be recognized that there are currently no data that allow us to say, even today, whether or not the CP has an adequate value.
It is important to emphasize that the dialysis clinics, in the public and private sectors, do not seem to have been minimally affected by the decrease in the value of CP, managing to maintain the excelente quality of dialysis that they had been practicing until then. In addition, and most likely due to the initially higher value of the CP, we must recognize that a significant number of infrastructures in the dialysis units were renovated at the private sector level.
However, despite corrections in the CP value, from 2010 to 2019, expenses with dialysis increase significantly. Mainly due to the increase in the number of patients undergoing treatment.
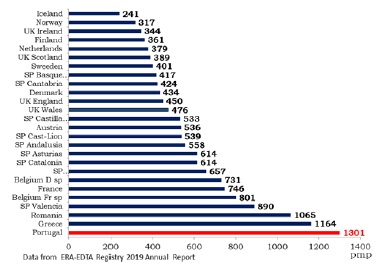
Portugal has one of the highest prevalence in dialysis of all countries in Europe and in the world (Fig. 3).
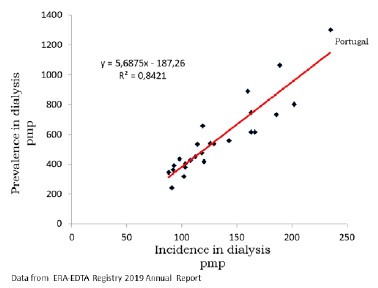
This results from the huge flow of patients entering dialysis annually (incidence), much higher than the outflow due to kidney transplantation, mortality and recovery of kidney function. The observation of data on the movement of patients registered in Portugal confirms that the incidence largely exceeds the sum of all the factors that lead to patients leaving dialysis. In Portugal, incidence is by far the determining factor of the high prevalence of dialysis observed in the country (Martins-Prata M. Incidence in dialysis in Portugal and Spain, information not published, request by email mateus.prata@gmail.com) and, as in other countries, there is a close relationship between incidence and prevalence in dialysis (Fig. 4).
The prevalence of dialysis in Portugal is not just high. There is a permanent and very significant annual increase. Between 2008 and the end of 2019, the prevalence of dialysis observed in Portugal increase from 924 pmp to 1301 pmp, an increase of 40.8% during this 11-year interval, with an annual growth, always positive, that ranged between 1.4% and 5.6%.5 This is a higher increase than that recorded in most other European countries. In some of them there was even a decrease during this same period: -26.8% in Ireland, -12.5% in Denmark and -4.7% in Scotland, respectively (Fig. 5).
Given the extraordinarily high prevalence of dialysis observed in Portugal, it is extremely important to analyze the influence it may have on the costs that the national health budget has to support annually with dialysis treatments.
Fig. 6 seeks to show how the decrease in CP alone would allow for a 17% decrease in expenses; the rise in prevalence, on the contrary, leads to an increase of 36%. The positive effect of decreasing CP it is not only completely nullified by the opposite effect resulting from the increase in prevalence, but it is even surpassed, with a 13% increase in expenses.
Everything seems to indicate that the high prevalence of dialysis represents the most important factor responsible for the high level of state expenditure in the treatment of chronic kidney disease. Moreover, new facts have recently emerged that help to better understand the preponderant effect of prevalence levels in dialysis annual cost.
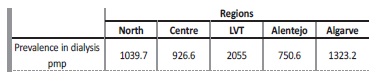
De Almeida et al, in a recently published article,6 not only confirmed the significant difference in prevalence in dialysis between Portugal and other European countries, but also demonstrated, for the first time, that similar, or even more significant differences, can be observed across different regions of the country (Table 1).
The causes underlying these “striking differences” are not known and little work has been done in this field, mainly because it is not allowed to consult data from the national dialysis records.7
The Lisbon and Tagus Valley Region (LTVR), with a population very similar to the North Region (NR) (just over 100 thousand inhabitants), has much higher annual costs with dialysis, with this difference varying between 26.6 and 50.1 million euros/year.8 Over the 10 years (2010 to 2019) LTVR spent 416 million more than NR. As the CP is the same in all regions, it is easy to conclude that the difference observed in the annual cost of dialysis between the two regions is mainly due to the number of patients undergoing treatment in each one of them (Fig.7).
We can therefore conclude that, of the two factors that influence anual expenditure on dialysis - CP and prevalence in dialysis - the first has had a positive effect, tending to reduce this expenditure through successive corrections of its initial value. On the contrary, the high number of patients undergoing dialysis treatment and its permanent increase is responsible for the extremely high expenses that the state has been supporting.
It is essential to bear in mind that the expenses considered correspond only to those included in the CP, not including other very significant ones regarding hospitalization, transport of patients and even other occasional expenses, all of them supported by the budget of the Ministry of Health.
It is very likely that the total expenditure on dialysis will reach 3%, or more, of the entire national budget for health. It is imperative to seek to act on the main factors responsible for this situation.
A reduction of the current level of CP will probably still be possible, provided that a thorough analysis is carried out, always taking into account the maintenance of the quality of the treatments. We agree that it will be hard work for politicians responsible for public health.
Another way of acting is to search, through precise analysis, on the reasons that lead to such a large number of patients having to enter dialysis. The clinical and laboratory characterization of patients at the time of entry into dialysis could lead to the knowledge of the reason, or reasons, of such a high influx of patients entering dialysis. Knowledge of these causes would certainly make it possible to establish the indispensable, adequate and effective measures, to allow a reduction in the incidence/prevalence to levels closer to what can be observed in most other European countries. This would probably be the most appropriate and effective way to reduce the enormous impact that spending on dialysis has on the state’s health budget.
For those who doubt the need to urgently take these measures, a careful reading of the 2019 Finnish Dialysis Register9 is recommended, in which one can verify the concerns that they decided to take, although with prevalence levels half of ours, to try to understand the cause of some small differences in the prevalence in dialysis observed between regions. Differences much lower than those observed among us.
CONCLUSION
Of the two factors that influence dialysis expenses in Portugal, the one that has the most impact seems to be the result of the huge number of patients entering dialysis annually. This fact is observed across the country but is particularly evident in the LVTR where expenditures greatly exceed those in other regions. Although the determining causes of this very high prevalence in dialysis are not known, there is still no research on this subject.
The considerable savings that could be made in dialysis expenses, by correcting the two factors that most influence it, could greatly contribute, if the responsible authorities decide to act, to be created and implemented adequate and effective measures that may correct the current situation: a country with one of the highest incidence and prevalence in dialysis in Europe and in the world.