INTRODUCTION
The aging of the world’s population and the increasing prevalence of diabetes are closely associated with the continuous increase in chronic kidney disease (CKD) prevalence. Data from the Portuguese registry of dialysis and transplantation 2021 showed a consistente increase in CKD 5D’s prevalence during the last 20 years in Portugal.
There were 12 601 patients on hemodialysis in Portugal at the end of 2021.1 In Europe 1 in 10 adults has some degree of CKD, but many do not know they have it.2 End stage renal disease (ESRD) patients correspond to 0.1% of the European population, however at least 2% of the European Union healthcare expenditure is assigned to ESRD patients’ treatment - The societal cost of ESRD patients is significantly higher than that of non-ESRD patients.
In high income countries (such as Portugal), despite the better healthcare service and the high costs of ESRD patient care, the CKD burden (measured in disability-adjusted life years-DALYs) has increased during the last 3 decades.3-5
Climate change is considered the greatest health threat of the 21st century, on the other hand, healthcare activities contribute significantly to the total national CO2 emissions - the global environmental burden from healthcare was between 1% and 5% of the total global burden.6 There is a strong correlation between a country’s healthcare carbon footprint (CFP) and the country’s healthcare spendings.7 In order to improve the long-term sustainability of nephrology, it is important to examine the association of nephrology’s carbon footprint, performance, and outcomes.
Nephrology is no exception to the bidirectional relationship between climate damaging activity and increased risk to renal patients from the climate emergency.
People living with kidney disease are particularly vulnerable to climate change effects in several ways. Firstly, extreme weather events such as flooding and overheating will increase the incidence of acute kidney injury especially in those with CKD. Extremely heat and limited access to water has been associated with CKD progression, rise of nephrolithiasis. Flooding and increased heating in previously temperate zones is likely to increase and vector-borne kidney diseases. In addition, there is the very real risk of interrupted treatment for patients with ESRD from infrastructure disruption in extreme weather events.8
On the other hand, nephrology, among healthcare services, has been pointed as one of the biggest contributors to healthcare’s CFP.
Dialysis modalities have a high water and power consumption, and hazardous waste generation per patient, that is disproportionally high compared to other medical therapies. As a speciality we therefore have a responsibility to minimize the environmental impact of kidney care.
SUSTAINABILITY OF NEPHROLOGY
The best step to reduce the CFP of kidney care is to prioritize primary and secondary prevention, with more investment on screening and in new approaches to reduce the CKD progression. Preventive strategies are significantly more cost-effective and eco-effective than kidney replacement therapies.9 Yet only 3% of healthcare expenditure is spent on prevention - there needs to be a paradigm shift from disease care and treatment to prevention and promotion of a healthy lifestyle for the good of future generations but also to reduce the environmental impact of health care.2
In Australia an annual CFP per patient on conventional hemodialysis (HD) was estimated at 10.2 tonnes CO2-equivalents(tCO2e) /patient/year - eight times the average healthcare footprint per capita (1.29 tCO2e/capita/year) and accounting for more than two-thirds of the estimated Australian mean annual per capita CO2 emission (15.4 tCO2e/capita/year).11,12 In the United Kingdom (UK), HD is estimated to have a CFP of 3.8 to 7.1 tCO2e/patient/year, more than 7 times the average per patient CFP in UK healthcare.10,11 Differences may be attributable to different assumptions, factors included in the calculation, type of energy sources, etc.
Water is required directly and indirectly for pharmaceutical production, energy generation, dialysate or peritoneal dialysis solutions production, hot water disinfection of the water distribution system, etc. Considering the water shortage in several areas, the environmental impact of dialysis modalities, beyond CFP, should be evaluated also with the water footprint (WFP) (an index that quantitatively measures the amount of water consumed in the process of production, consumption, and disposal of products).
Hemodialysis produces two types of water effluents that are frequently directed to sewage. The first is water rejected by the reverse osmosis (RO) systems and the second is the dialysate effluent. It is surprising that in areas with severe drought and/or water shortage (such as Portugal), the water resources management is not a daily reality and a legal imposition (or at least a moral obligation).
Progresses in water treatment technologies as well as eficient management of dialysate consumption will be key approaches to save water. Emerging technologies, such as NxStage® system and sorbent technology may reduce the consumption and allow dialysate regeneration, respectively.
Greenhouse gas emissions arise directly from healthcare facilities, as well as indirectly from the supply chain of healthcare devices, consumables and services. Two studies found that drugs production and distribution is a major contributor to both WFP and CFP, which could exceed the CO2 emissions and the water used directly on hemodialysis.10,13
Beyond its CFP and WFP, the environmental impact of drugs may be evaluated in another perspective: drugs that are not taken are discarded as domestic waste and drugs’ metabolites are eliminated on urine and on dialysis effluent and pollute waters. It should be noted that polypharmacy is frequent in CKD patients and up to 40% of medications prescribed to those with chronic conditions are never consumed.14
A single HD session can produce up to 2.5 kg of solid waste, being estimated that a patient on thrice-weekly dialysis not reusing their dialyzer produces 390 to 546 kg per year.15,16 More than one third of the waste produced in HD (and up to two thirds in peritoneal dialysis) is plastic, mainly PVC (the most important component of dialyzers and dialysis tubing)16 but less than one-third of non-hazardous plastic (23%-28%) is recyclable.17 It should be noted that plastic production requires significant amounts of chemicals, energy and water.
A starting point could be the reduction of the amount of waste (for instance by reducing wraps of dialysis disposables) and a correct classification and separation between hazardous and non-hazardous waste at bedside.18 Beyond the higher ecologic impact, a correct waste classification has relevant economic savings - the cost of hazardous waste management can be 10 to 30 times that of nonhazardous waste, which can result in significant savings without investment or compromising the quality of care. Taking the Italian example, the savings of 50 cents per hemodialysis treatment (100 to 250 g of hazardous waste) would lead to saving about 5 million Euros per year.18
As always information and education are mandatory - the first step to launching a green nephrology movement is to create awareness among all the involved actors (from patients and clinicians to politicians) of the significant environmental burden of nephrology.
Medical schools and postgraduate teaching need to embed health and environmental sustainability formation into curricula, a structured program into nephrology training residency would encourage trainees to develop the mindset to consider the sustainability impact of their everyday clinical practice.
In the first survey focused on the environmental sustainability of Portuguese nephrology we found that only 6% of respondents (8/136) had received prior formal training on this topic, but 93% would be willing to receive more information (119/128, 93.0%) (unpublished data, Laranjinha I et al).19 Table 1 presents the estimation of the annual water and energy consumptions, waste generation and CFP of the patients under hemodialysis in Portugal.
Table 1 Ecologic footprint of hemodialysis comparing with the total footprint of a Portuguese inhabitant.1,16,29
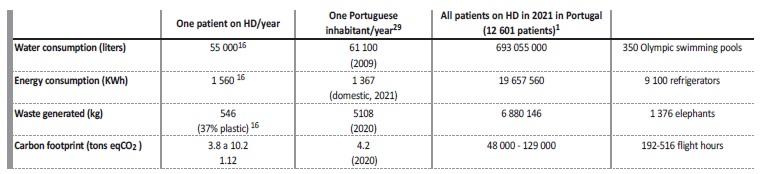
Footprint estimation of all the Portuguese patients on HD in 2021 (assuming that all the patients performed HD thrice weekly during the complete year of 2021, i.e., 156 treatments in 2021)
Analyzing these data, we realize that one patient on HD, only for its HD treatments, generates an environmental footprint comparable to the total of an average Portuguese inhabitant.
Considering that, in 2021, there were 12 601 HD patients in Portugal (data from Portuguese Society of Nephrology) and assuming thrice weekly HD sessions, in order to dialyze these patients, 350 Olympic swimming pools of water and more than 19 million kWh of energy were consumed, almost 7 thousand tons of waste were produced and around 2 million dialyser units were used and disposed of. The CFP, waste generation and water and energy consumption of a hemodialysis patient is similar of a median Portuguese inhabitant -Hemodialysis centers and Nephrology units should calculate their own carbon footprint and define reduction goals.
Peritoneal dialysis might be perceived as more environment-friendly, because of its direct lower water and energy requirements (mainly for continuous ambulatory peritoneal dialysis (CAPD)). However, PD has a higher need of plastic use for the bags and packaging, which results in more waste; the solution production process consumes more water, and more energy is used for transportation.
Transplantation is the least expensive modality for society, especially in young patients with a long-life expectancy. Transplantation combines lower costs with higher survival and quality of life, but it is restricted to the patient population with the most favorable performance status and comorbidities.20
Nephrology and dialysis should change its approach from a “cradle to grave” life cycle to a circular model (“cradle-to-cradle” concept), involving biodegradable or recycling materials, or their repeated use (abandoning, if safe, the “single use” principle).
Moving beyond direct carbon emissions, an accurate estimation of the ecological footprint of a medical device requires a comprehensive life cycle assessment, from development, production, distribution, to use and elimination - these data are frequently not available.21 Industry must be an ally in this path to a greener nephrology, and we should promote this transition by including environmental criteria in the procurement process, making an eco-friendly attitude competitive between manufacturers.22 In close collaboration with nephrologists, manufacturers need to increase their efforts in the development of more environmentally sustainable devices and products.
Only one study was found evaluating the CFP of a nephrology department (that covers a population of 865 000). In this Unit, the total CFP distributed by functional departments was: 65.4% to the HD (225 patients) and peritoneal dialysis (54 patients), 30.5% procurement, 27.4% to the inpatient ward (14 bed ward) and 5.7% to the outpatient department (7800 appointments per year). On the other hand, the distribution of the total CFP considering the activity áreas was: 35% to the pharmaceutical subsector, 25% to medical equipment, 15% to travel (HD represents 34% of overall travel emissions), 13% to facility energy and 8.7% to waste.12
Some of the interventions to be implemented require no technology or investment, and there are several reports showing that the overall changes to improve nephrology environmental sustainability may increase costs in the short term (as an investment in equipment must be made) but will result in long term cost savings, contributing to financial sustainability over time.10
The international and national regulations (such as, in Portugal, Despacho n.º 242/96 that classifies all the waste produced in a hemodialysis room as biohazardous or toxic)23 are often inadequately restrictive and preclude a more rational waste management and recycling.
CONCLUSION
Urgent strategies are needed to balance the best kidney care with its environmental impact. Several initiatives have been released such as the creation of the “Sustainable Kidney Care Committee” of the UK kidney Association,24 the “Green Nephrology Committee” of the ERA-EDTA25 and the “The European Green Deal and Nephrology” by the European Kidney Health Alliance2,26 and several publications have been published such as the position statement by the Italian Society of Nephrology27 and the Environmental Guidelines for Dialysis published by the European Dialysis and Transplant Nurses Association/European Renal Care Association (EDTNA/ERCA).28
For instance, the UK Green Nephrology Program surveyed baseline practices and stimulated environmentally focused research with stakeholders to test innovations and alternatives to the actual heavy r0esource consuming nephrology. In Portugal, initiatives at the government and regulatory authorities’ level by changing legislation and publishing green nephrology guidelines might have powerful impacts.
Sustainability can be defined as meeting the needs of the presente without compromising the ability of future generations to meet their needs, and it can be analyzed in different facets, such as social, economic and environmental. Clearly, current nephrology is unsustainable, in all its facets, if its activities are maintained as we currently know them.















