Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Nascer e Crescer
versión impresa ISSN 0872-0754versión On-line ISSN 2183-9417
Nascer e Crescer vol.27 no.2 Porto jun. 2018
QUAL O SEU DIAGNÓSTICO? | WHAT IS YOUR DIAGNOSIS?
Nephro urology case
Caso Nefrourológico
Andreia A. MartinsI; Ivete AfonsoI; Maria Sameiro FariaII; Teresa CostaII; Armando ReisIII; Rui MachadoIV; Conceição MotaII
I Department of Pediatrics, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos. 4454-509 Matosinhos, Portugal. andreiaamartins87@gmail.com; ivete.afonso@hotmail.com
II Unit of Pediatric Nephrology, Department of Pediatrics, Centro Materno Infantil do Norte. Centro Hospitalar do Porto. 4099-001 Porto, Portugal. mariasameirofaria@gmail.com; teresa.v.c.tavares@gmail.com; conceicaocmota@gmail.com
III Department of Urology, Centro Hospitalar do Porto. 4099-001 Porto, Portugal. armandobreis@hotmail.com
IV Department of Angiology and vascular Surgery, Centro Hospitalar do Porto. 4099-001 Porto, Portugal. rmvasc@gmail.com
ABSTRACT
The Nutcracker Syndrome (NS) originates from the compression of the left renal vein in its trajectory, mostly between the aorta and the superior mesenteric artery, or less frequently between the aorta and the lumbar spine. Although asymptomatic in most cases, it can be a rare cause of hematuria.
We present the case of an 11-year-old male adolescent who was referred to a Pediatric Nephrology evaluation for a two-month-long gross hematuria. The patient also had anemia without hemodynamic repercussion. After the initial work-up, it was concluded to be a non-glomerular, extra-renal hematuria. Abdominal and renal ultrasound with Doppler was normal. The abdominal and pelvic computerized angiotomography revealed, after a careful examination, the presence of NS. Due to persistent gross hematuria with the need for transfusional support, at the age 13, the patient underwent a renal autotransplantation.
The diagnosis of NS is essentially clinical, imagiological and necessarily a diagnosis of exclusion. The treatment must be individualized and requires a multifactorial approach.
Keywords: Hematuria; Nutcracker syndrome
RESUMO
A Síndrome de Nutcracker (SN) resulta da compressão da veia renal esquerda ao longo do seu trajeto, na maioria dos casos entre a aorta e a artéria mesentérica superior ou, menos frequentemente, entre a aorta e a coluna lombar. Apesar de na maioria dos casos ser assintomática, constitui uma causa rara de hematúria.
Descreve-se o caso de um adolescente de 11 anos referenciado à consulta de Nefrologia Pediátrica por hematúria macroscópica com dois meses de evolução, associada a anemia sem repercussão hemodinâmica. Após investigação, concluiu tratar-se de uma hematúria não glomerular, de origem extra-renal. A ecografia abdominal e renal com Doppler não revelou alterações. A angiotomografia computorizada abdominopélvica, após cuidadosa análise, revelou a presença de SN. Por hematúria persistente com necessidade de suporte transfusional, aos 13 anos foi submetido a autotransplante renal. O diagnóstico da SN é essencialmente clínico, imagiológico e necessariamente de exclusão. A orientação terapêutica deve ser individualizada e requer uma abordagem multifatorial.
Palavras-chave: Hematúria; Síndrome de Nutcracker
A 11-years-old male adolescent, with prior repetition tonsillitis, was referred to a Pediatric Nephrology consult for a two-month-long persistent gross hematuria. He also had iron-deficiency anemia without hemodynamic repercussion. There was no history of fever, asthenia, abdominal or lumbar pain, dysuria, pollakiuria, edema, recent infection or abdominal trauma. Of notice, the mother had history of nephrolithiasis.
The physical examination showed the patient had normal blood pressure, mucocutaneous pallor and a body mass index of 21 kg/m2 (85th-97 th percentil).
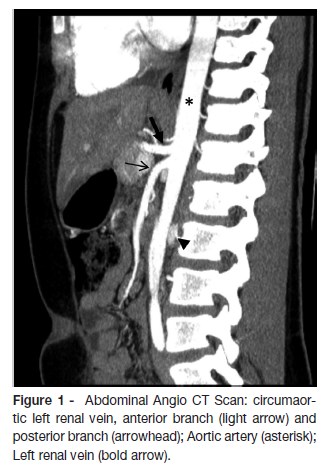
The patient had a microcytic hypochromic anemia and the urinalysis revealed hematuria, without dysmorphic erythrocytes, and orthostatic non nephrotic proteinuria. The remaining laboratorial tests (coagulation, renal function, total proteins, albumin, lipid profile, immunoglobulins, autoimmune panel, complement, urinary electrolytes) were normal. The abdominal ultrasound was unremarkable in two different occasions and there were no masses, nephrolithiasis or morphologic changes in the renal ultrasound and the Doppler was normal. Afterwards, an abdominal and pelvic computerized angiotomography (Angio CT scan) showed a circumaortic left renal vein without further related changes (figure 1). Cystoscopy showed a normal urethra and bladder and bleeding originating from the left ureter. When the Angio CT scan images were revised, a proximal dilation of the left renal vein was discovered, with the retroaortic branch imprisoned between the aorta and the spine (figure 2).
At the age of 13, due to persistent gross hematuria associated with anemia needing transfusional support, the patient underwent a renal autotransplantation. In the postoperative period, a renal artery thrombosis of the autotransplanted kidney complicated the procedure with consequent left nephrectomy.
What is your diagnosis?
DIAGNOSIS
Posterior Nutcracker Syndrome (NS)
DISCUSSION
The NS is a rare, probably underdiagnosed cause of recurrent non glomerular hematuria in children.1,2 Its prevalence is unknown.1-5 Typically, it manifests between the third and fourth decade, but it can be diagnosed at any age and there is a slight female predominance.1-6
The etiopathogenesis is not fully understood. Some theories include an abnormal origin of the superior mesenteric artery from the abdominal aorta, posterior renal ptosis, and a decrease in retroperitoneal fat with a consequent decrease in the aortomesenteric angle (AMA).1,4
The most frequent form of NS (anterior nutcracker) is associated with left renal vein (LRV) compression between the abdominal aorta (AA) and the superior mesenteric artery (SMA), in a shape similar to the handles of a nutcracker.1-7 In about 3% the compression of the LRV occurs between the AA and the lumbar spine (retroaortic renal vein) designated posterior nutcracker.1 In most cases, it represents a normal variant, clinically asymptomatic, named nutcracker phenomenon.4-6 When symptomatic, they lead to gross or microscopic hematuria, orthostatic proteinuria (which may be in the nephrotic range), left flank and/or lumbar pain and periureteral or gonadal varices.1-6 Non glomerular hematuria is the most common symptom, due to the rupture of thin-walled varices to the adjacent renal calyx.2,4-6 Usually, the bleeding is self-limited, without hemodynamic repercussion or anemia.1,3,4
The diagnosis requires a clinical suspicion and can be confirmed by imagiological techniques.1,2,4,7 A renal ultrasound with Doppler is the non-invasive exam of choice, with a sensitivity of 69-79%.3,4,6 It allows to measure the anteroposterior diameter and the peak flow velocity of the LRV in two points (usually in the origin from the aorta and the point where it is stenosed).3,6 When the ultrasound is not enlightening, a computerized tomography or magnetic resonance arteriography should be made.1-4 These techniques allow for a better definition of the anatomical relation between the LRV, AA, SMA and lumbar spine, and should be carefully reported.1-4 The gold standard test for the diagnosis of NS is the phlebography, which can reveal the compression and collateral circulation.7 The pressure gradient between the renal vein and the inferior vena cava can also be measured.7 However, there are limitations in measuring this pressure gradient and its interpretation in pediatric age.7
The treatment of a NS must be individualized, based on the severity and persistence of symptoms.1-6 Knowing that most cases (75%) in children resolve spontaneously, a conservative approach is the first choice.1-6 However, in cases with severe chronic pain, massive hematuria, chronic kidney disease or with no response to a conservative treatment after more than 24 months, a surgical approach should be attempted and the type of intervention depends on each centers experience.1,4,6 In this case, due to persistent hematuria with the need for transfusional support, a surgical intervention was decided after 20 months of conservative treatment.
REFERENCES
1. Sousa B, Tavares M, Braga A, Vieira A, Mariz C, Freitas A, et al. Síndrome de nutcracker como causa de hematúria recorrente. Acta Pediatr Port 2002; 33:441-4. [ Links ]
2. Calado R, Braz M, Lobo L, Simão C. Síndrome de nutcracker: Hematúria sem diagnóstico? Acta Med Port 2011; 24:695-8. [ Links ]
3. Ahmed K, Sampath R, Khan MS. Current trends in the diagnosis and management of renal nutcracker syndrome: A review. Eur J Vasc Endovasc Surg 2006; 31:410-6. [ Links ]
4. Teixeira E, Machado M, Grilo E, Moreira A, Cordinhã C, Carmo C, et al. Síndrome de Nutcraker: Um diagnóstico a Evocar. Acta Pediatr Port 2016; 47:182-6. [ Links ]
5. Barka M, Mallat F, Hmida W, Chavey SO, Ahmed KB, Abdallah AB, et al. Posterior nutcracker syndrome with left renal vein duplication as a cause of gross hematuria and recurrent left varicocelo in an eight-year-old boy. Int J Case Rep Images 2014 ;5:572-5. [ Links ]
6. Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc 2010; 85:552-9. [ Links ]
7. Machado M, Machado R, Mendes D, Almeida R. May-Thurner syndrome associated with a nutcracker syndrome, clinical case and literature review. Angiologia e Cirurgia Vascular. 2017; 2: 52-6. [ Links ]
CORRESPONDENCE TO
Andreia A. Martins
Department of Pediatrics
Hospital Pedro Hispano
Unidade Local de Saúde de Matosinhos.
Rua Dr. Eduardo Torres
4454-509 Matosinhos
Email: andreiaamartins87@gmail.com
Received for publication: 02.01.2018
Accepted in revised form: 03.04.2018














