Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.1 Porto jan. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i1.15081
ORIGINAL ARTICLES | ARTIGOS ORIGINAIS
Behavioral insomnia in a pediatric sleep clinic: restrospective study
Insónia comportamental numa consulta de sono pediátrica: estudo retrospetivo
Rosa MartinsI, Lia OliveiraI, Rosário FerreiraII
I. Department of Pediatrics, Hospital de Santa Maria, Centro Hospitalar Lisboa Norte, Academic Medical Centre of Lisbon. 1649-035 Lisboa, Portugal. rmmartins16@gmail.com; lcfoliveira@gmail.com
II. Pediatric Pulmomology Unit, Department of Pediatrics, Hospital de Santa Maria, Centro Hospitalar Lisboa Norte, Academic Medical Centre of Lisbon. 1649-035 Lisboa, Portugal. rosariotferreira@sapo.pt
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Background/Objective: Behavioral insomnia is a common sleep disorder among children, with potentially negative impact on health, behavior, and cognition. This study aimed to characterize a pediatric population referred to a Sleep Disorder Clinic of a tertiary hospital due to behavioral insomnia.
Methods: Retrospective and descriptive study based on the review of medical records of patients with insomnia over an eight-year period (2008−2016). Results are presented as median (minimum-maximum), mean (standard deviation), and percentage.
Results: A total of 964 children attended the Sleep Disorder Clinic in the considered time period, 162 (16.8%) of which due to insomnia and 137 (14.2%) to behavioral insomnia. Most children (58.4%) were male and the median age at referral was 45 months (5 months-18 years). The median bedtime was 10 pm (8 pm−4 am) and nocturnal awakenings were frequent, particularly in pre-school aged children. Regarding bedtime routines, 62% of children were not able to fall asleep alone, 48.9% had television in the bedroom, 43.1% (11.9% of which, teenagers) required an object to fall asleep, and 42.3% required lights on. Most patients (62%) had a routine to fall asleep, which was dependent on the caregiver in younger children and on television and reading in teenagers. The most frequent daytime symptoms were sleepiness in older children and irritability in younger children. Regarding treatment, 29.9% were taking drugs before referral.
Conclusions: Most children in this study were preschoolers, an important age window. Later sleep time, TV in the bedroom, and parental dependence to fall asleep were frequent, revealing a broad area for intervention. The authors propose greater investment in training health professionals and caregivers working in the area, in order to promote the adoption of adequate sleep hygiene as a form of prevention.
Keywords: behavioral insomnia; children; sleep
RESUMO
Introdução/Objetivo: A insónia comportamental é um distúrbio do sono frequente em idade pediátrica, com repercussões potencialmente negativas na saúde, comportamento e capacidade cognitiva das crianças. O objetivo deste estudo foi caracterizar a população referenciada a uma consulta pediátrica do sono de um hospital terciário por insónia comportamental.
Métodos: Estudo retrospetivo e descritivo baseado na revisão de processos clínicos de doentes seguidos por insónia na referida consulta especializada durante um período de oito anos (2008−2016). Os resultados são apresentados como mediana (mínimo-máximo), média (desvio padrão) e percentagem.
Resultados: No total, 964 crianças foram referenciadas à consulta de sono, 162 (16.8%) das quais por insónia e 137 (14.2%) por insónia comportamental. A maioria (58.4%) era do sexo masculino e a mediana de idades aquando da referenciação foi de 45 meses (5 meses-18 anos). A mediana da hora de deitar foi 22:00 (20:00-4:00), tendo sido frequentes os despertares noturnos, sobretudo em idade pré-escolar. Relativamente às rotinas na hora de deitar, 62% das crianças não adormeciam sozinhas, 48.9% tinham televisão no quarto e 43.1% (11.9% das quais, adolescentes) precisavam de um objeto e 42.3% de luz acesa para adormecer. A maioria (62%) das crianças tinha uma rotina para adormecer, dependente do cuidador em crianças mais novas e de televisão e leitura nos adolescentes. Os sintomas diários mais frequentemente referidos foram sonolência em crianças mais velhas e irritabilidade em crianças mais novas. Relativamente ao tratamento, 29.9% encontrava-se a receber tratamento farmacológico antes da referenciação.
Conclusão: A maioria das crianças neste estudo encontrava-se em idade pré-escolar, a qual constitui uma importante janela de atuação. A hora de deitar tardia, presença de televisão no quarto e dependência dos pais para adormecer foram frequentes, o que revela a necessidade de intervenção na área. Os autores propõem um maior investimento na formação dos profissionais de saúde e cuidadores, de modo a promover a adoção de medidas de higiene do sono adequadas como forma de prevenção.
Palavras-chave: insónia comportamental; crianças; sono
Introduction
Insomnia is defined as difficulty in initiating or maintaining sleep and in children often manifests as refusal to go to bed, tantrums, difficulty in falling asleep alone or with lights off, and frequent nocturnal awakenings with the need for parental comfort.1 To be considered a sleep disorder, symptoms must occurs at least three times per week, persist for at least three months, and result in significant functioning impairment in the child or parents.2
The 2014 revision of the International Classification of Sleep Disorders (ICSD-3) grouped insomnia in three categories: “chronic insomnia disorder”, “short-term insomnia disorder”, and “other insomnia disorder”.2 However, for the purpose of evaluation and subsequent application of specific behavioral interventions in clinical practice, it is useful to acknowledge the following categories of childhood insomnia: behavioral insomnia of childhood (BIC), psychophysiological insomnia, and transient sleep disorders. Insomnia can also be classified into primary or secondary, according to the absence or presence of an underlying physical or psychological problem, respectively. Primary insomnia includes behavioral and psychophysiological insomnia.
BIC is the most prevalent type of childhood insomnia in children under the age of five, although it can persist until middle childhood or beyond. It usually presents as bedtime refusal, prolonged sleep onset, or nocturnal awakenings. BIC can be subdivided into three types: 1) sleep-onset association, characterized by frequent nocturnal awakenings and difficulty in children falling asleep on their own; 2) inadequate parental limit setting, defined as refusal in going to bed and a lack of parental rule-setting; and 3) a mixed type, with characteristics of the first two types.
The main causes and triggering factors of insomnia vary according to children’s age and development. BIC is often not recognized by parents as a problem, despite the well-known harmful consequences of sleep deprivation in cognitive development, behavioral changes, and physical health and its negative impact on the quality of life of children and their families.3-7
Behavioral sleep problems are found in all age groups: 25−50% of infants over the age of six months experience night awakenings, 15−30% of preschoolers have difficulty falling asleep or experience night awakenings, 15% of children in middle childhood display bedtime resistance and/or psychophysiological insomnia, and almost 11% of adolescents experience insomnia, mainly anxiety-related.8-10 In a population-based study conducted in Pennsylvania, one in every five children or pre-adolescents were shown to have insomnia symptoms; the highest prevalence (approximately 30%) was observed in girls aged 11−12 years, potentially more related to hormonal changes than to anxiety/depression.11 A population study conducted in Portugal with children aged two to ten years reported a 10.4% prevalence of sleep problems.3 However, data on the prevalence of behavioral insomnia in Portugal is unknown.
The therapeutic approach to these patients must include sleep hygiene, behavioral measures and, in individual cases, pharmacological treatment. Importantly, when initiating a behavioral strategy parents should be advised on healthy sleep habits. A good sleep hygiene is the cornerstone of a healthy sleep development: setting rules and routines helps children synchronize their circadian rhythm with the remaining family.1,12,13 Consistent bedtime routines are associated with better sleep outcomes, including longer sleep duration and reduced night awakenings.14
The main objective of this study was to characterize a pediatric population referred to a Sleep Disorder Clinic of a tertiary hospital due to behavioral insomnia to identify the most prevalent factors associated with the condition.
Methods
This was a retrospective descriptive study based on the review of medical records of children taken to a Sleep Disorder Clinic of a tertiary hospital with insomnia as main complaint over an eight-year period (from 2008 to 2016).
Insomnia type was classified according to the ICSD-3.3 Variables investigated included age, gender, personal medical history, family history of insomnia, sleep habits, nocturnal awakenings, naps, bedroom features (e.g. presence of television, videogames, or music), way of falling asleep (e.g. use of an usual object; need for lights on or for caregiver intervention; place of falling asleep), daytime symptoms (e.g. sleepiness, hyperactivity). Additionally, pharmacological and nonpharmacological therapeutic measures were reviewed.
Retrieved results were summarized as median (minimum-maximum) for continuous variables and percentage for nominal variables. Children were grouped as infants (0−2 years old), preschool-aged children (3−5 years old), school-aged children (6−10 years old), and teenagers (11−18 years old). A descriptive statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS®) version 20.
Results
A total of 964 children attended the Sleep Disorder Clinic during the study period, 162 (16.8%) of which due to insomnia. Patients were mainly referred by pediatricians from the same or other hospitals (n=75; 46.3%) and by general doctors (n=31; 19.1%). Insomnia was classified as primary in 89.5% (n=145) and behavioral in 94.5% (n=137) of patients. Among behavioral insomnia patients, the following subtypes were identified: limit-setting (11.7%; n=16), sleep onset association (24.1%; n=33), and combined (64.2%; n=88).
BIC patients had a median age at first visit of 45 months (5 months−18 years) and a slight predominance of male gender (58.4%; n=80). Children under the age of six years were the most represented (63.5%; n=87), with infant and toddler predominance (n=55). The second most prevalent group was school-aged children (20.4%; n=28), while teenagers were the least prevalent group, with 14.6% (n=20).
The most frequent comorbidities in this pediatric population were atopic dermatitis, rhinitis and asthma (16.8%; n=23), and neurodevelopmental disorders (13.1%; n=19), with global developmental delay predominance (36.8%). Family history of insomnia was found in 30.7% of patients (n=42) and the most commonly affected relative was the mother (13.1%; n=18).
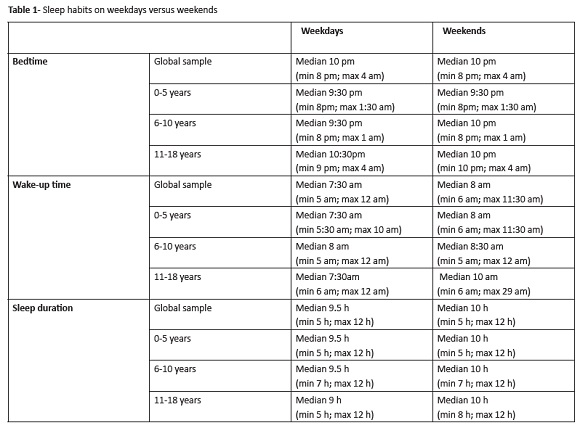
Children’s sleep habits are depicted in Table 1. In the overall population, the number of night sleeping hours was greater on weekend than weekdays, especially due to later wake-up hours in the former. When stratifying by age, sleep habits were similar in the 0−5 and 6−10-year-old groups during weekdays and weekends. Differences in sleep habits were attributed to the group of teenagers with later bedtime on weekdays and later waking-up hours on weekends (Table 1). Nocturnal awakenings occurred in 87.6% of children (n=120); most (42.4%; n=65) had one to three and 30.7% (n=42) had four to six awakenings per night.
Sixty-eight patients (49.6%) took naps, predominantly children below the age of three years (73.5%; n=50). Most of these children (79.4%; n=54) usually took one nap per day, with a reported median duration of each nap of 1.25 (0.5-3) hours.
Concerning bedroom features, 48.9% (n=67) had television, 24.1% (n=33) had music, and 12.4% (n=17) had videogames in the bedroom. Infants and preschoolers were who most frequently had television in the bedroom (28.5%; n=39), followed by school-aged children and teenagers (20.4%; n=28). Videogames were mostly reported in the older age group (8.8%; n=12).
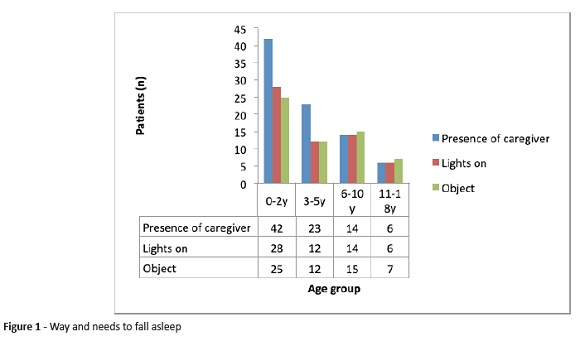
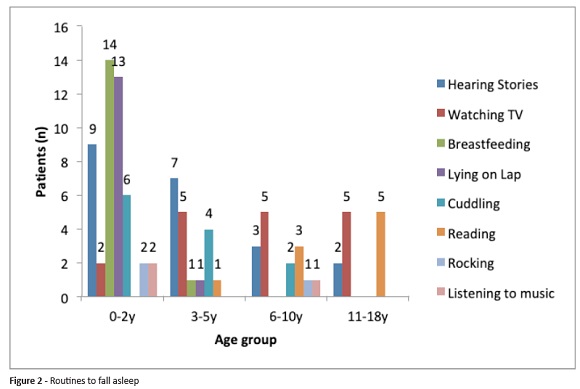
Regarding the way of falling asleep, most children (78.1%; n=107) used to fall asleep in bed. However, 62% (n=85) required the presence of a caregiver, 42.3% (n=58) required lights on, and 43.1% (n=59) required an object to fall asleep. The most frequently used objects were a doll (27%; n=37), a special pillow (5.1%; n=7), or a pacifier (2.9%; n=4). These findings tended to decrease with age (Figure 1). Most patients (62%; n=85) had a routine to fall asleep, particularly infants (29.9%; n=41) and preschoolers (13.1%; n=18). This routine mainly consisted of hearing stories (n=21), watching television (n=17), breastfeeding (n=15), lying on the lap (n=14), cuddling (n=12), reading (n=10), rocking (n=3), or listening to music (n=3). The favored type of routine according to age group is presented in Figure 2.
The most frequent daytime symptoms were irritability (29.2%; n=40), difficulty to concentrate (24.1%; n=33), headaches (15.3%; n=21), and sleepiness (7.3%; n=10). Analysis of symptoms according to age group revealed that the most common symptom among infants was irritability (n=16) and among teenagers was sleepiness (n=11).
Concerning therapeutic measures, around thirty-three percent (33.6%; n=46) of patients were receiving pharmacological treatment, most of which were infants (11.7%; n=16) and preschoolers (11.7%; n=16). Most patients were taking medication prescribed by the attending physician before referral (89.1%; n=41). Eleven children kept the previously prescribed pharmacological treatment and only five children started drug therapy during follow-up. Melatonin was the most frequently prescribed drug (47.8%; n=22), followed by hydroxyzine (13%; n=6), cetirizine (8.7%; n=4), clonazepam (6.5%; n=3), risperidone (6.5%; n=3), chloral hydrate (4.3%; n=2), and others (zolpidem, clonidine, promethazine, fluvoxamine, trazodone).
Overall, 21.2% (n=29) of patients were discharged and 33.6% (n=46) were lost the follow-up after leaving the clinic by parental decision. The remaining patients are currently on follow-up.
Discussion
The frequency of insomnia types reported in this pediatric population agrees with previous reports: behavioral insomnia was the most common type and, as shown in this study, is a frequent reason for referral to a pediatric sleep outpatient clinic, especially in pre-school male children.1 This suggests that many pediatricians and general physicians do not have enough training and/or experience to address this frequent childhood condition.
Sleep disorders may significantly affect child development, as they are associated with health and behavioral problems.6,15,16 Chronic insomnia may significantly impair cognitive development, mood regulation, attention, behavior, and quality of life, not only in children but in the entire family, resulting in sleep deprivation of parents and caregivers, with associated quality of life compromise.4,5
Genetic factors are known to contribute to a higher insomnia prevalence. This was confirmed in the present study, in which family history of insomnia was found in a significant percentage of patients (30.7%), with the mother being the most commonly affected relative.17,18
Although in this study the duration of night sleep reported by parents seems adequate, it may also be overestimated. By relying solely in parental report, only bedtime schedules were considered instead of the real time that children slept. As expected from the well-known decrease in night sleep with age, teenagers were the age group with the shorter sleep duration (median of 9 hours during weekdays).19 Indeed, this sleeping hour number seems reduced considering that the 50 percentile of sleep duration from 11 to 16 years old should be greater than 9 hours.19 Furthermore, a later bedtime was found in teenagers, as reported for this age group.20 A phase delay is usual in teenagers, leading to short sleep periods, as school starts early in the morning. Consequently, sleep default is frequent and manifests as difficulty waking up in the morning and sleepiness.21 The attempt to compensate sleepiness with naps during the day or unlimited sleep time during weekends leads to additional nocturnal delayed sleep. This irregular sleep schedule between weekdays and weekends, as well as the use of stimulating substances (caffeine) or drugs (licit and illicit), use of electronic devices in the bedroom before bed, social and family pressures, hormonal changes, and the need to belong to a group also contribute to poor sleep quality during adolescence.22
As expected, the frequency and number of nocturnal awakenings reported in this study were globally high and generally related to sleep-onset associations, a more prominent characteristic in preschoolers. After a physiological nocturnal awakening, the child needs the same intervention to go back to sleep. Although the reported number of awakenings in the considered age group is normal, the problem arises from the inability to go back to sleep alone, extending the alertness period. Most children are expected to be able to self-sooth and fall asleep on their own by the age of one year, even after the usual nocturnal awakenings reported in this age group.23 For this purpose, transition objects may be a way of gradually preparing young children for falling asleep on their own.12 In the present study, a significant number of patients (43.1%) required an object to fall asleep, with this percentage reducing with age, as expected. Furthermore, maintaining a bedtime routine consisting in the same activities in the same order immediately before going to bed is associated with better sleep outcomes.14 In this sample, although most patients had a sleep routine, these were parentor TV-dependent.
Naps are part of a healthy sleep pattern in young children, with obvious well-known benefits. Despite being frequent and normal in this group, children’s age as well as the number and duration of naps is very variable, with no standard pattern.19,24 In this study, naps were more frequent in young children, which is consistent with previous reports.24
Some published evidence suggests a role for falling asleep habits and lack of bedtime rules in the development of sleep disorders, particularly behavioral insomnia.13,25 A high frequency of inadequate sleep habits was reported in this population of insomnia patients which, although decreasing with age, were still common among teenagers. Among these, a high proportion of children watched television and used electronic devices in the bedroom before falling asleep. The negative impact of such habits in the quality of sleep in children and teenagers is well documented.26
Daytime symptoms associated with poor nocturnal sleep quality reported in this population were similar to those previously reported, with irritability being the most common insomnia symptom in young children and daytime sleepiness most common in older children.4
Although not specified, neurodevelopmental disorders were common in this study, what is in line with previous research. Attention-deficit disorder/hyperactivity disorder, autism spectrum disorder, and depression are conditions associated with sleep disorders as insomnia.17 As a significant number of patients in this study had atopic disease, including rhinitis, the authors speculate that this can partly justify symptoms suggestive of poor sleep quality. Symptoms of nocturnal asthma and rhinitis disrupt sleep continuity due to frequent awakenings, affect daytime sleepiness and school performance, and increase school absenteeism.27,28 Co-occurring night time allergic rhinitis symptoms may further contribute to sleep disruption, daytime fatigue, and somnolence.29
Insomnia treatment starts with a detailed assessment of causes and triggers, in order to understand the underlying mechanisms and define the best therapeutic approach. The main strategy for treating primary insomnia should be the adoption of adequate sleep hygiene routines. Sleep hygiene was the basis of the therapeutic approach used in all patients in this study, with pharmacological treatment only used in refractory cases.
Behavioral techniques are also a treatment option. However, its practical applicability is often difficult and requires a significant parental effort. The benefits of behavioral interventions and of several proposed techniques (e.g. extinction, gradual extinction, minimal checking with systematic extinction, positive routines and reinforcement, relaxation techniques such as meditation, programmed awakening, sleep remodeling) are well demonstrated, with positive effects in children’s and parents’ quality of sleep.4,30,31
Cultural background is an important factor potentially affecting sleep habits, namely regarding sleep place, sleep duration, sharing parents’ bed, or using transition objects. This issue should be considered when planning an intervention, as parents’ expectations and tolerance to sleep behavioral problems seem to have a strong cultural influence.1,3,32
There is currently no evidence supporting the use of drugs alone for BIC treatment.4 The pharmacological approach must always be accompanied by behavioral measures. Furthermore, there are no specific medications for insomnia in children. The use of drugs in this patient population is based on clinical experience and empirical data from adults, and most have an only short-term effect and thus may not be a good option for the intended purpose.33 In a recent review, Bruni et al. suggested that the pharmacological treatment of insomnia should be guided by the underlying mechanism and pathophysiology.34
In this study, approximately one third of patients were on pharmacological treatment at the time of clinical presentation. The most used drug was melatonin, a non-prescription pharmacological treatment, easily accessible to caregivers. Melatonin decreases sleep onset latency but not night awakenings. Therefore, the effect of melatonin is well described in sleep-onset insomnia and delayed sleep phase syndrome only, with little evidence of its effects on sleep maintenance insomnia.35 As behavioral treatment was initiated, less than half of patients were maintained on drug treatment.
As prevention is more effective than treatment in defining appropriate sleep routines, parents should be informed by the pediatrician or general practitioner about sleep hygiene and adequate sleep routines during routine visits. Family physicians/general practitioners and pediatricians have an important role in promoting sleep hygiene in children. Properly educating these professionals is extremely important, since sleep disorders of behavioral origin can be prevented with adequate sleep hygiene measures.5,36 An adequate sleep hygiene is based on three major aspects: environment, schedule, and activities before bedtime. Informed parents can resort less to specialized care, which is more expensive, avoiding additional costs to the health system and improving quality of sleep and professional performance.31
Regarding outcomes, only 21.2% of children were discharged and a significant percentage (33.6%) was lost the follow-up after parents deciding to leave the clinic. The authors believe that this shows the difficulty in changing routines and applying sleep hygiene measures and new behavioral measures.
This study’s retrospective design implies some limitations. On the one hand, it prevented to assess families’ socioeconomic level, a factor that has been identified as shaping the quality of sleep in children and adolescents. On the other hand, it prevented identifying the type of intervention performed and assessing its relative efficacy, what would be interesting. Another study limitation is the fact that it relied on parental reporting rather than on objective measures.
The authors believe that some of these children could be managed in primary/general pediatrician care. However, whenever associated sleep disorders (such as sleep-disordered breathing or restless leg syndrome) or relevant comorbidities are suspected or there is inadequate child response or failure by caregivers to comply with the prescribed behavioral interventions or medication, the child should be referred to a pediatric sleep clinic.
Conclusion
In this study, most children with insomnia in a specific and selected population were preschoolers, an important age window for developmental measures and interventions. Late sleep time, TV in the bedroom and dependence on parents to fall asleep were frequent, revealing a broad field for intervention.
Discussing these problems in advance during medical visits, together with early diagnosis and intervention, have the potential to improve sleep habits and prevent behavioral insomnia, thus minimizing their impact on parents’ and children’s quality of life. The authors consider that a greater investment in training health professionals and caregivers in this area would be important for that purpose.
REFERENCES
1. Owens JA, Mindell JA. Pediatric Insomnia. Pediatr Clin North Am 2011; 58:555-69. [ Links ]
2. American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd edition, American Academy of Sleep Medicine, Darien, IL 2014. [ Links ]
3. Silva FG, Silva CR, Braga LB, Neto AS. Hábitos e problemas do sono dos dois aos dez anos: estudo populacional. Acta Pediatr Port 2013; 44:196-202. [ Links ]
4. Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A; American Academy of Sleep Medicine. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006; 29:1263-76. [ Links ]
5. Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep 2009; 32:599-606. [ Links ]
6. Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analyses of short sleep duration and obesity in children and adults. Sleep 2008; 31:619-26. [ Links ]
7. Gozal D, O.Brien LM. Neurocognitive dysfunction and sleep in children: from human to rodent. Pediatr Clin North Am 2004; 51:187-202. [ Links ]
8. Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry 2002; 43:713-25. [ Links ]
9. Kerr S, Jowett S. Sleep problems in pre-school children: a review of the literature. Child Care Health Dev 1994; 20:379-91. [ Links ]
10. Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr 2000; 21:27-36. [ Links ]
11. Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med 2014; 15:91-5. [ Links ]
12. Nunes ML, Cavalcante V. Clinical evaluation and treatment of insomnia in childhood. J Pediatr 2005; 81:277-86. [ Links ]
13. Ferber R. Sleeplessness in children. In: Ferber R, Kryger M editors. Principles and practice of sleep medicine in the child. Philadelphia: W. B. Saunders; 1995. p.79-89. [ Links ]
14. Mindell JA, Li AM, Sadeh A, Kwon R, Goh DYT. Bedtime Routines for Young Children: A dose-Dependent Association with Sleep Outcomes. Sleep 2015; 38:717-22. [ Links ]
15. Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. A longitudinal study of preeschoolers´ language-based bedtime routines, sleep duration, and well-being. J Fam Psychol 2011; 25:423-33. [ Links ]
16. Quach J, Gold L, Arnup S, Sia K-L, Wake M, Hiscock H. Sleep well-be well study: improving school transition by improving child sleep: a translational randomised trial. BMJ Open 2013; 3: e004009. [ Links ]
17. Nunes ML, Bruni O. Insomnia in childhood and adolescence: clinical aspects, diagnosis, and therapeutic approach. J Pediatr (Rio J) 2015; 91(Suppl 1):S26-35. [ Links ]
18. Zhang J, Li AM, Kong APS, Lai KY, Tang NL, Wing YK. A community-based study of insomnia in Hong Kong Chinese children: Prevalence, risk factors and familial aggregation. Sleep Med 2009; 10:1040-6. [ Links ]
19. Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 2003; 111:302-7. [ Links ]
20. Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep 1993; 166:63-8. [ Links ]
21. Louzada F, Menna-Barreto L. Relógios biológicos e aprendizagem. São Paulo: EDESPLAN; 2004. [ Links ]
22. Fossum IN, Nordnes LT, Storemark SS, Bjorvatn B, Pallesen S. The association between use of electronic media in bed before going to sleep and insomnia symptoms, daytime sleepiness, morningness, and chronotype. Behav Sleep Med 2014; 12:343-57. [ Links ]
23. Goodlin-Jones BL, Eiben LA, Anders TF. Maternal well-being and sleep-wake behaviors in infants: an intervention using maternal odor. Infant Ment Health J 1997; 18:378-93. [ Links ]
24. Anders TF, Sadeh A, Apparedy V. Normal sleep in neonates and children. In: Ferber R, Kryger M editors. Principles and practice of sleep medicine in the child. Philadelphia: W. B. Saunders. 1995. p.7-18. [ Links ]
25. Hayes MJ, Parker KG, Sallinen B, Davare AA. Bedsharing temperament and sleep disturbance in early childhood. Sleep 2001; 24:657-62. [ Links ]
26. Paavonen EJ, Pennonen M, Roine M, Valkonen S, Lahikainen AR. TV exposure associated with sleep disturbances in 5-to 6-year-old children. J Sleep Res 2006; 15:154-61. [ Links ]
27. Koinis-Mitchell D, Kopel SJ, Boergers J, Ramos K, LeBourgeois M, McQuaid EL, et al. Asthma, allergic rhinitis, and sleep problems in urban children.J Clin Sleep Med 2015; 11:101-10. [ Links ]
28. Fagnano M, Bayer AL, Isensee CA, Hernandez T, Halterman JS. Nocturnal asthma symptoms and poor sleep quality among urban school children with asthma. Acad Pediatr 2011; 11:493-9. [ Links ]
29. Peroni D, Piacentini G, Alfonsi L, Zerman L, Di Blasi P, Visona’ G, et al. Rhinitis in pre-school children prevalence, association with allergic diseases and risk factors. Clin Exp Allergy 2003; 33: 1349-54. [ Links ]
30. Halal CSE, Nunes ML. Education in children´s sleep hygiene:which approaches are effective? A systematic review. J Pediatr 2014; 90:449-56. [ Links ]
31. Hiscock H, Bayer JK, Hampton A, Ukoumunne OC, Wake M. Long-term mother and child mental health effects of a population-based infant sleep intervention: cluster-randomized controlled trial. Pediatrics 2008; 122:e621-27. [ Links ]
32. Sadeh A, Mindell JA, Luedtke K, Seifer R, Tremblay A, Civita R, et al. Sleep and psychological characteristics of children on a psychiatric inpatient unit. J Am Acad Child Adolesc Psychiatry 1995; 34:813-9. [ Links ]
33. Ramchandani P, Wigs L, Webb V, Stores G. A systematic review of treatments for settling problems and night-waking in young children. Br Med J 2000; 320:209-13. [ Links ]
34. Bruni O, Sette S, Angriman M, Baumgartner E, Selvaggini L, Belli C, et al. Clinically Oriented Subtyping of Chronic Insomnia of Childhood. J Pediatr 2018; 196:194-200. [ Links ]
35. Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol 2015; 19:122-33. [ Links ]
36. Gruber R, Cassoff J, Knauper B. Sleep health education in pediatric community settings: rationale and practical suggestions for incorporating healthy sleep education into pediatric practice. Pediatr Clin North Am 2011; 58:735-54. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Rosa Martins
Department of Pediatrics
Hospital de Santa Maria
Centro Hospitalar Lisboa Norte
Academic Medical Centre of Lisbon
Avenida Professor Egas Moniz
1649-035 Lisboa
Email: rmmartins16@gmail.com
Received for publication: 20.09.2018
Accepted in revised form: 11.11.2019