Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.1 Porto jan. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i1.14036
CASE REPORTS | CASOS CLÍNICOS
Ultrasound relevance in prenatal diagnosis of vacterl association - two clinical cases
A importância da ecografia no diagnóstico pré-natal da associação vacterl - dois casos clínicos
Joana FélixI, Joana Moreira BarrosI, Ana Rita SoaresII, Fátima SoaresI, Rosete NogueiraIII,IV, Pedro Tiago SilvaI
I. Department of Gynecology and Obstetrics, Hospital Pedro Hispano. 4464-513 Senhora da Hora, Portugal. joanapatriciafelix@gmail.com; joanajunior@msn.com; fatima.soares.romero@gmail.com; pedro.tiago@ulsm.min-saude.pt
II. Department of Medical Genetics, Centro Hospitalar Universitário do Porto. 4099-001 Porto, Portugal. anaritamsoares@gmail.com
III. Life and Health Sciences Research Institute (ICVS), Universidade do Minho 4710-057 Braga, Portugal. rosetenogueira@gmail.com
IV. CGC Genetics, Laboratory of Pathology. 4000-432 Porto, Portugal. rosetenogueira@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
VATER is a nonrandom association of congenital defects with common developmental pathogenesis including/which includes malformations like vertebral defects, anal atresia or imperforate anus, tracheoesophageal fistula with esophageal atresia, and radial or renal dysplasia. VATER acronym was initially used to describe this association, but other malformations, like cardiac defects and limb anomalies, were later also considered cardinal features and included, changing the acronym to VACTERL.
Although few cases have been reported, VATER/VACTERL spectrum association can be detected in first-trimester ultrasound.
Herein, the authors describe two cases of VATER/VACTERL association suspected during the 12-week ultrasound and confirmed in anatomopathological study. Prenatal VACTERL association diagnosis is challenging and rarely detected in the first pregnancy trimester. It requires skill and experience to interpret ultrasound findings and some features are difficult to recognize before birth. Early diagnosis is important for parental counselling and delivery planning. Management options include medical pregnancy termination and delivery in a tertiary center to improve outcomes.
Keywords: fetal malformations; fetal ultrasound; prenatal diagnosis; VACTERL association
RESUMO
VATER é uma associação não aleatória de defeitos congénitos associados com patogénese comum. Inclui malformações como anomalias vertebrais, atrésia ou imperfuração anal, fístula traqueo-esofágica com atrésia esofágica e displasia renal ou radial. O acrónimo VATER foi inicialmente utilizado para descrever esta associação, mas outras anomalias, como defeitos cardíacos e anomalias dos membros, foram mais tarde também consideradas alterações cardinais e incluídas, modificando o acrónimo para VACTERL.
Embora estejam descritos poucos casos na literatura, a associação do espetro VATER/VACTERL pode ser precocemente detetada na ecografia do primeiro trimestre de gravidez.
Os autores apresentam dois casos de associação VATER/VACTERL, em que a suspeita do diagnóstico na ecografia das 12 semanas foi confirmada através de estudo anatomopatológico. O diagnóstico pré-natal de associação VACTERL é desafiante e dificilmente estabelecido no primeiro trimestre de gravidez, requerendo competências específicas e experiência para interpretar o exame ecográfico. O diagnóstico precoce é importante para o aconselhamento do casal. A abordagem da condição pode passar por interrupção médica da gravidez ou realização do parto num hospital com cuidados diferenciados para o recém-nascido.
Palavras-chave: associação VACTERL; diagnóstico pré-natal; ecografia fetal; malformações fetais
Introduction
In the early 1970’s, VATER acronym was used to describe an association characterized by presence of vertebral anomalies, anal atresia or imperforate anus, tracheoesophageal fistula with esophageal atresia, and radial or renal dysplasia.1,2 VACTERL is one of several VATER adaptations, including cardiac and limb defects.1,3,4
The nonrandom VATER/VACTERL association derives from a common developmental pathogenesis consisting of a blastogenesis defect occuring early in gestation, before pregnancy day 35.5
Vertebral anomalies are very common features of the condition (up to 80%) and can result from segmentation defects, such as hemivertebrae, vertebral fusion, or absent vertebrae.1 Cardiac defects are also very common (40−80%) and can range from mild to severe, the most frequent being ventricular septal defects, auricular septal defects, and complex anomalies.1,6-8
Absence of gastric bubble on ultrasound (US) can help identify an esophageal atresia, but this sign is absent when tracheoesophageal fistula is present, what occurs in 50−80% of cases.5 Renal anomalies as agenesis or dysplasia occur in up to 25% of patients and prenatal ultrasound is important for diagnosis.1,2 Limb defects, as hypoplastic thumb, polydactyly, and radial aplasia are also frequent features and can be detected early in pregnancy.1 Anal atresia and imperforate anus are easily diagnosed after birth, but may be missed in fetal US.
Detailed morphological study is mandatory in presence of fetal malformations. The evaluation is echographic, but magnetic resonance imaging (MRI) can be used under certain circumstances.1
The anatomopathological study is important to confirm echographic abnormalities and investigate associated anomalies.3
Although prevalence of this condition is difficult to determine due to absence of universal diagnostic criteria, it is generally acknowledged as a rare association (1/10.000 to 1/40.000 live newborns).1
Diagnosis is usually established based on three or more cardinal defects, but these anomalies may not be evident until adulthood.1,3,9,10
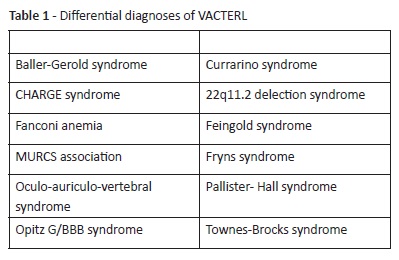
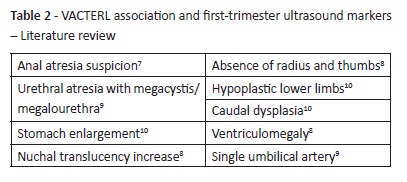
Exclusion of syndromes and other associations potentially confused with VACTERL should be performed within a multidisciplinary approach including a pathologist experienced in fetal pathology and a clinical geneticist (Table 1).1,4
The low prevalence and clinic heterogeneity of cases hampers etiological study. Most associations are now considered multiple polytopic defects likely caused by the interaction of genetic and environmental factors.5 Risk factors, like maternal diabetes and drugs, have been identified.5 Benjamin D. Solomon suggested a hereditary mode of transmission, but no consistent genetic anomalies have been found yet. In a very small percentage of VACTERL patients, a potentially linked genetic mutation was identified.1
US exam is the primary modality for fetal anatomy study. Technological developments and acquired experience have enabled detection of an increased number of malformations. Like most imaging exams, US depends on the skill and experience of the medical interpreter. Some anomalies can be easily identified, but others are difficult to detect in utero, even with a trained sonographer. In these cases, indirect signs may raise suspicion of an anomaly.1
With this case report, the authors wish to demonstrate how technical advances have enabled an increasingly early malformation detection. Table 2 displays a literature review of VACTERL malformations that can be identified in first-trimester US.3,11-15
Obstetric US assessment also includes further studies, as single umbilical artery (SUA) or polyhydramnios. These are important markers in prenatal diagnosis, due to their association with increased risk of multiple malformations.1,12,16
In patients with abnormal routine US, a more detailed assessment, either by fetal echocardiogram or MRI, is mandatory to improve morphological study. Further exams, including invasive procedures, may also be necessary to exclude other diagnoses (Table 1).1, 6
In the case reports herein described, anatomopathological evaluation was key for diagnosis, confirming defects observed in US and identifying other anomalies difficult to detect in imaging evaluation.
Cases reports
Case 1:
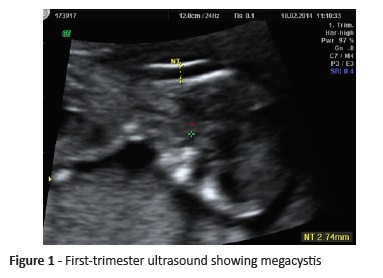
A pregnant woman with no relevant family or personal medical history was referred to our Hospital for first-trimester combined screening. US revealed a single fetus with 12 weeks and six days. Increased nuchal translucency (NT >95 percentile), megacystis, and SUA were detected. Chorionic villus sampling (CVS) was performed, with normal male karyotype result (46, XY).
Fetal death was diagnosed in the 16-week ultrasound (Figure 1). Nuchal edema and megacystis were constant features. The patient was admitted for second-trimester uterine evacuation medical protocol.
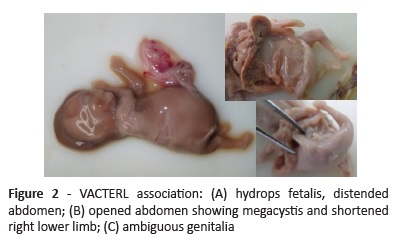
Fetal anatomopathological evaluation confirmed nuchal edema and megacystis identified in ultrasound, together with anal imperforation, ambiguous genitalia, urethral atresia, rectovesical fistula, right renal agenesis, and small right lower limb, consistent with VACTREL association diagnosis (Figure 2). Placental pathological study confirmed SUA and identified velamentous cord insertion and thrombotic vascular lesion in fetal vessels of stem villi at histological study.
Case 2:
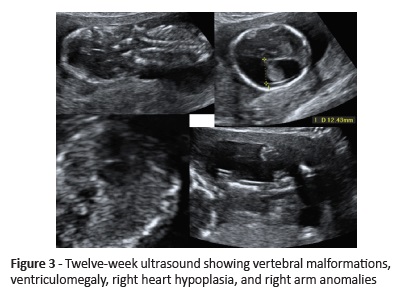
A nullipara woman with no relevant personal or family medical history was referred to our Hospital to perform first-trimester aneuploidy screening. She presented with a single fetus of 12 weeks and three days with 4.2-mm NT (> 95 percentile) associated with ventriculomegaly, cystic hygroma, abnormal cervical spine, right heart hypoplasia, ulnar deviation of the right hand, and left clubfoot (Figure 3).
CVS was performed and karyotype was normal for a female fetus (46, XX).
Parents decided to terminate pregnancy due to malformative syndrome.
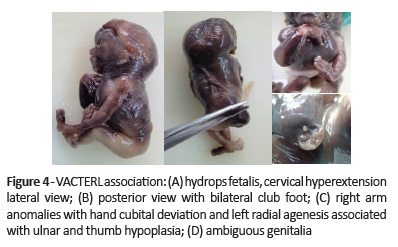
Anatomopathological exam confirmed cystic hygroma, cervical hyperextension, ventriculomegaly, and right arm anomalies with cubital hand deviation. Additional features identified included atypical facies, preauricular pits, other vertebral defects, renal anomalies, and ambiguous genitalia, as well as left radial agenesis associated with ulnar and thumb hypoplasia and bilateral minor defects of the hands, legs, and feet. (Figure 4). Histological exam revealed histiocytoid cardiomyopathy.
SUA and marginal cord insertion were additional placental features.
Discussion
An association is defined by the nonrandom co-occurrence of a group of malformations that occur together by chance more often than expected. VACTERL association diagnosis is usually established after birth, but antenatal identification of anomaly patterns is possible.
In Case 1, 12-week ultrasound showed nonspecific fetal abnormalities, precluding VATER/VACTERL association diagnosis.
As alterations on routine US led to more detailed study, CVS was performed and early second-trimester ultrasound was scheduled. Although this 16-week exam revealed a fetus without vitality and with nuchal edema and megacystis, VACTERL diagnosis relied on fetal anatomopathological exam.
On the other hand, in Case 2 the first trimester ultrasound allowed to identify three typical features of the condition: cardiac anomaly and vertebral and limb defects.
In both cases, the anatomopathological exam was key to confirm malformations previously identified on US and provided additional findings that enabled VACTERL association diagnosis.
Parental counseling is not easy in these situations, but pregnancy termination may be considered a valid choice in presence of severe anomalies, as in the two presented cases. These couples should also be informed that 90% of VACTERL associations are sporadic and have a low recurrence risk.1
Conclusion
US is the gold standard in fetal anatomy study and a valid tool for detecting prenatal anomalies associated with VACTERL association since the first pregnancy trimester.
In the present two cases, anatomopathological examination was important to confirm US anomaly findings and detect other malformations enabling the final diagnosis of VACTERL.
REFERENCES
1. Solomon, B. VACTERL/VATER Association.: Orphanet J Rare Dis, 2011, 6:56. [ Links ]
2. Krapp M, Geipel A, Germer U, Krokowski M, Gembruch U.First-trimester sonographic diagnosis of distal urethral atresia with megalourethra in VACTERL association. Prenat Diagn. 2002; 22:422-4. [ Links ]
3. Gilbert-Barness E. Potter’s Pathology of Fetus, Infant and Child. 2nd ed. vol 1 chap1. Philadelphia: Mosby; 2007. [ Links ]
4. Bergmann C, Zerres K, Peschgens T, Senderek J, Hörnchen H, Rudnik-Schöneborn S.. Overlap between VACTERL and hemifacial microsomia illustrating a spectrum of malformations seen in axial mesodermal dysplasia complex (AMDC). Am J Med Genet A. 2003; 121A:151-5. [ Links ]
5. Debich-Spicer, Gilbert-Barness E. Embryo & Fetal Pathology color atlas with ultrasound correlation. Cambridge University Press, 2004.
6. Jongsong T, Wanapirak C, Piyamongkol W, Sudasana J. Prenatal sonographic diagnosis of VATER association. J Clin Ultrasound. 1999; 27:378-84. [ Links ]
7. Lam Y,Shek T, Tang M. Sonographic features of anal atresia at 12 weeks. Ultras Obstet Gyneco. 2002; 19:523-4. [ Links ]
8. Dane B, Kayaoğlu Z, Dane C and Aksoy F. VACTERL-H syndrome: first trimester diagnosis. J Turk Ger Gynecol Assoc. 2011; 12:266-9. [ Links ]
9. Krapp M, Geipel A, Germer U, Krokowski M and Gembruch U. First-trimester sonographic diagnosis of distal urethral atresia with megalourethra in VACTERL association. Prenat Diagn. 2002; 22:422-4. [ Links ]
10. Santos J, Nogueira R, Pinto R, Cerveira I, Pereira S. First trimester diagnosis of VACTERL association. Clinics and Practice. 2013; 3:e5. [ Links ]
11. Källén K, Mastroiacovo P, Castilla EE, Robert E, Källén B. VATER non-random association of congenital malformations: study based on data from four malformation registers. Am J Med Genet. 2001; 101:26-32. [ Links ]
12. Solomon B, Bear KA, Kimonis V, de Klein A. Clinical Geneticists’ Views of VACTERL/VATER. Am J Med Genet, 2012, 158A:3087-100. [ Links ]
13. Solomon BD, Baker LA, Bear KA, Cunningham BK, Giampietro PF, Hadigan C, Hadley DW, et al. An approach to the identification of anomalies and etiologies in neonates with identified or suspected VACTERL (vertebral defects, anal atresia, tracheo-esophageal fistula with esophagealatresia, cardiac defects, renal and limb anomalies) association. J Pediatr. 2014; 164:451-7.e1. [ Links ]
14. Mori M, Matsubara K, Abe E, Matsubara Y, Katayama T, Fujioka T, et al. Prenatal diagnosis of persistent cloaca associated with VATER (vertebral defects, anal atresia, tracheo-esophageal fistula, and renal dysplasia). Tohoku J Exp Med. 2007; 213:291-5. [ Links ]
15. Debost-Legrand A, Goumy C, Laurichesse-Delmas H, Déchelotte P, Perthus I, Francannet C, et al. Prenatal diagnosis of the VACTERL association using routine ultrasound examination. Birth Defects Res A Clin Mol Teratol. 2015; 103:880-6. [ Links ]
16. Ertugrul I, Dogan V, Beken S, Ozgur S, Okumuş N, Orün UA, et al. UHL’S anomaly as a part of VACTERL association. Genet Couns. 2015; 26:273-6. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Joana Félix
Department of Gynecology and Obstetrics
Hospital Pedro Hispano
Rua de Dr. Eduardo Torres
4464-513 Senhora da Hora
Email: joanapatriciafelix@gmail.com
Received for publication: 05.03.2018
Accepted in revised form: 17.06.2019