Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Nascer e Crescer
versión impresa ISSN 0872-0754versión On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.1 Porto ene. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i1.14777
CASE REPORTS | CASOS CLÍNICOS
Pediatric bacillary pulmonary tuberculosis - case report
Tuberculose pulmonar bacilífera em idade pediátrica - caso clínico
Andreia LombaI, Ana FerrazI, Sónia Regina SilvaI, Maria Manuel FloresI, Alcina SaraivaII
I. Department of Pediatrics, Hospital Infante D. Pedro, Centro Hospitalar do Baixo Vouga. 3810-501 Aveiro, Portugal. andreiaflcorreia@gmail.com; anaibferraz@gmail.com; soniasilva81@sapo.pt; mariamanuelflores@gmail.com
II. Department ou Pulmonology, Hospital Infante D. Pedro, Centro Hospitalar do Baixo Vouga. 3810-501 Aveiro, Portugal. alcina.saraiva.11075@chbv.min-saude.pt
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Children are more susceptible than adults to development of tuberculosis after exposure to active disease, hence screening and chemoprophylaxis are particularly important. Although Portugal is considered to have a low burden of tuberculosis, educating the population on the importance of screening and treatment is vital to decrease the number of cases. Herein is reported the case of an 11-year-old girl with previous contact with active tuberculosis who was lost to follow-up and later diagnosed with bacillary pulmonary tuberculosis.
Keywords: chemoprophylaxis; mycobacterium tuberculosis; pediatric; pulmonary tuberculosis
RESUMO
Após exposição a doença ativa, as crianças são mais suscetíveis do que os adultos ao desenvolvimento de tuberculose, sendo o rastreio e a quimioprofilaxia particularmente relevantes nesta faixa etária. Apesar de Portugal ser considerado um país com baixo ónus de tuberculose, é importante educar a população acerca da importância do rastreio e tratamento, de modo a diminuir o número de casos. É apresentado o caso de uma adolescente de onze anos de idade que teve contacto com um caso de tuberculose ativa e foi perdida para seguimento, sendo mais tarde diagnosticada com tuberculose pulmonar bacilífera.
Palavras-chave: mycobacterium tuberculosis; pediatria; quimioprofilaxia; tuberculose pulmonar
Introduction
Pediatric tuberculosis (TB) represents a major public health concern worldwide. The World Health Organization reports that approximately 11% of the people developing TB each year are children aged less than 15 years.1 Children contribute to 3-6% of the total number of TB cases in developed countries and a significant proportion of TB morbidity and mortality cases are reported in childhood.1,2
In Portugal, a reduced rate of TB has been reported in the first decades of the 21st century in people aged less than 15 years. In 2017, only 2.2% of notified cases were reported in children under the age of 15 years and incidence rate in the 0−4-year age group was 6.1/100,000. TB incidence in the country was 15.6/100,000, placing Portugal in the group of low-TB-burden countries.3
Nonetheless, TB control in children has often been neglected due to the fact that they are ineffective bacillus transmitters, frequently escaping the attention of TB control programs.2
Children are infected with TB by contacting with infected patients and are thus considered excellent indicators for assessing TB status in the community, as well as the efficacy of adopted epidemiological control measures. Childhood infection is always suggestive of recent Mycobacterium tuberculosis transmission, indicating failure of the public health system in controlling the disease within the community.4
Herein is reported the case of an 11-year-old girl with a severe TB form, characterized by extensive cavitary, highly contagious lesions. The case had several diagnostic particularities which raised important epidemiological issues.
Case report
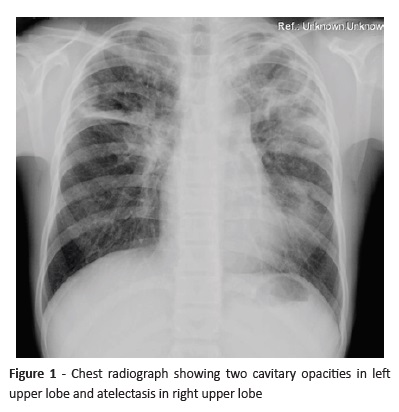
An 11-year-old, previously healthy female was sent to the Pediatric Emergency Room (ER) by the family doctor with a three-month history of insidious cough without other symptoms. She had previously received cough suppressants, a macrolide antibiotic, inhaled bronchodilators, and inhaled corticosteroids, with no improvement. The girl had been vaccinated with Bacille Calmette-Guérin vaccine at birth. Chest x-ray showed two cavitary lesions in the left upper lobe and atelectasis in the right upper lobe (Figure 1).
During physical examination in the ER, the girl was febrile (axillary temperature of 38.3ºC) with audible rales over the lung apices; no other relevant changes were evident. White cell count was 18,000/μL with left deviation (12,200/μL neutrophils). C-reactive protein was 6.68 mg/dL and sedimentation rate was 55 mm/h. Sputum contained frequent acid-fast bacilli, polymerase chain reaction for M. tuberculosis was positive, and M. tuberculosis was subsequently cultured. Tuberculin skin test (TST) was strongly positive (28 mm of induration). Pulmonary TB diagnosis was established and the patient was hospitalized and isolated in a negative pressure room.
Previous contact with TB cases was investigated and revealed that the girl’s father had been diagnosed with active pulmonary TB simultaneously with lung cancer three years earlier, subsequently dying. At that time, the girl had a TST with 13 mm induration and chemoprophylaxis with isoniazid (INH) was prescribed. However, she did not comply with chemoprophylaxis from the start and was subsequently lost to follow-up.
Following pulmonary TB diagnosis, investigation of subsequent contacts was initiated by public health authorities and five school colleagues were identified with TB infection, starting chemoprophylaxis.
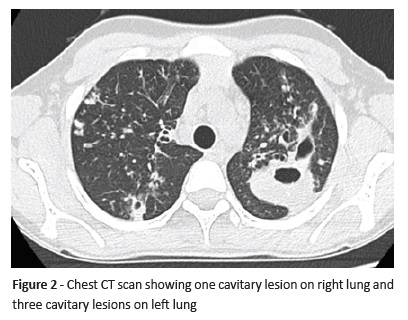
As the girl’s father had an M. tuberculosis strain sensitive to INH, rifampicin (RIF), and pyrazinamide (PZA), treatment with these three drugs was initiated (INH 300 mg, RIF 600 mg, and PZA 750 mg). During hospitalization, chest computed tomography revealed multiple bilateral cavitary lesions and endobronchial disease (Figure 2). Progressive clinical and radiological improvement was apparent.
The girl was discharged home 30 days later, after sputum was negative on direct smear. Antibiogram confirmed M. tuberculosis susceptibility to all first-line drugs. She was observed weekly in the local Pulmonology Diagnostic Centre and twice-weekly in the Pediatric Clinic and was put under directly observed therapy. Subsequent chest x-rays showed clinical improvement. The girl completed three months of triple therapy and an additional six months of double therapy with INH and RIF. Treatment was uneventful, with good outcome.
Discussion
A case of severe bacillary pulmonary TB with cavitary lesions in a young girl was reported. TB diagnosis in children is challenging, since clinical presentation is often non-specific and bacteriological confirmation is achieved in less than 15% of cases. This is the main reason why a detailed assessment including careful exposure history, clinical examination, and relevant investigation is required.4 As bacteriological confirmation is not always possible, TB diagnosis should be based on clinical findings suggestive of TB, exposure history, evidence of abnormalities on chest x-ray or other imaging exams, and/or evidence of tuberculosis infection (positive TST and/or interferon gamma release assay).5
Young children, particularly infants, have a high risk of progression from latent TB infection (LTBI) to active TB disease.6 Therefore, identification of latently infected children is important as TB preventive strategy. LTBI is defined as M. tuberculosis infection without clinical features or radiographic findings of TB disease.1 Children with LTBI should start chemoprophylaxis, usually with INH as monotherapy for nine months.7 In the present case, chemoprophylaxis was prescribed at the time of contact identification, but patient did not adhere to treatment and missed several appointments and subsequent follow-up.
Child TB is usually a non-contagious form of disease, but in this case late detection likely led to a severe and highly contagious form of pulmonary TB. Insidious symptoms resulted in a late TB diagnosis, with subsequent important pulmonary parenchyma lesions with multiple cavities. Cavitary TB forms, such as in this case, are usually reported in adults, and their occurrence in children is a warning sign to the community. Delayed diagnosis of a highly contagious, extended pulmonary TB form raises major epidemiological concerns in a child community. Public health authorities should carry out intensive identification of subsequent patient contacts within the community.
Careful monitoring of treatment compliance is recommended.4 Poor compliance to TB treatment represents the main reason for treatment failure. Consequently, the widespread use of directly observed therapy is encouraged, through a patient-centered strategy in which ingestion of each TB medication dose is observed.1
In conclusion, this case shows that extensive and contagious pulmonary TB forms are still present in children in countries considered to have a low burden of disease and healthcare professionals should be aware of this diagnosis to actively identify cases. It also emphasizes that prevention strategies must be optimized by designing case-tailored interventions to ensure acceptance, compliance, and completion of the chemoprophylaxis regimen.
REFERENCES
1. Berti E, Galli L, Venturini E, de Martini M, Chiapinni E. Tuberculosis in childhood: a systematic review of national and international guidelines. BMC Infectious Diseases. 2014; 14:1471-2334. [ Links ]
2. Cruz AT, Starke, JR. Pediatric Tuberculosis. Pediatrics in Review. 2010; 31;13. [ Links ]
3. Portugal. Ministério da Saúde. Direção-Geral da Saúde. Tuberculose em Portugal - Desafios e Estratégias 2018 Lisboa: Direção-Geral da Saúde, 2018. [ Links ]
4. Fildan AP, Tofolean D, Toma C, Tudorache E, Dantes E. Severe cases of pediatric tuberculosis. Jurnalul Pediatrului; 2015; 18;33-7. [ Links ]
5. Migliori GB, Sotgiu G, Rosales-Klintz S, Centis R, D’Ambrosio L, Abubakar I, et al. ERS/ECDC Statement: European Union standards for tuberculosis care, 2017 update. Eur Respir J. 2018. 17;51. [ Links ]
6. Kitai I, Demers A. Pediatric Tuberculosis. In: Menzies D, editor. Canadian Tuberculosis Standards, 7th edition; 2013, p. 219-45. [ Links ]
7. Carvalho A, Carvalho I, Marques L, Pereira L, Brito MJ, Duarte, R. Consensus about the management of the child exposed to a patient with tuberculosis. Acta Pediatr Port 2014; 45;242-51. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Andreia Lomba
Department of Pediatrics
Hospital Infante D. Pedro
Centro Hospitalar do Baixo Vouga
Avenida Artur Ravara
3810-501 Aveiro
Email: andreiaflcorreia@gmail.com
Received for publication: 11.07.2018
Accepted in revised form: 17.06.2019