Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.2 Porto jun. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i2.20440
EDITORIAL
Cardiovascular care in cancer patients
Seguimento cardiovascular no doente com cancro
Sílvia ÁlvaresI,II,III
I. Editor-in-chief of Nascer e Crescer - Birth and Growth Medical Journal. Centro Hospitalar Universitário do Porto. 4099-001 Porto, Portugal. silviaalvares.dia@chporto.min-saude.pt
II. Department of Pediatric Cardiology, Centro Materno-Infantil do Porto, Centro Hospitalar Universitário do Porto. 4099-001 Porto, Portugal.
III. Unit for Multidisciplinary Research in Biomedicine, Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto. 4050-313 Porto, Portugal.
With improvements in cancer therapy and early diagnosis, pediatric cancer survival rates have significantly increased over the two last decades, with estimates indicating that around 80% of children will survive at five years after diagnosis. However, childhood cancer survivors (CCS) are at risk of developing cardiovascular (CV) disease, currently the second cause of late mortality and morbidity following recurrence of the original cancer. Indeed, mortality related to CV events is approximately eight-fold higher compared with age matched general population.1-3 Risk of coronary artery disease (CAD), cerebrovascular accidents, and congestive heart failure in these patients is respectively 10, 9, and 15 times greater than in siblings.3
The pathogenesis of this increased cardiovascular risk is multifactorial and complex, mediated by modalities of treatment such as radiation exposure, anthracyclines and other chemotherapeutic agents and stem cell therapy.1-6
Possible complications of chemotherapy and/or radiation include myocardial dysfunction and heart failure, CAD, valvular heart disease, arrhythmias (acquired long QT syndrome, atrial fibrillation and atrioventricular block), arterial hypertension, thromboembolic disease, pulmonary hypertension and pericarditis.1-6
Strategies to prevent cardiotoxicity range from improvement of radiotherapy techniques that minimize irradiation to the heart, minimizing exposure to the chemotherapy, use of medications thought to prevent myocardial damage (e.g. dexrazoxane), and initiating cardioprotective drugs at the right time.3-7
CV disease related to radiation exposure is dependent of dose, volume and technique of irradiation. Cardiovascular toxicity appears to be progressive, risk is life long, and manifestations include congestive heart failure, CAD, pericardial disease, cardiomyopathy, valvular abnormalities and conduction abnormalities. Radiation exposure is also associated with traditional CV risk factors, namely hypertension, dyslipidemia, and type 2 diabetes mellitus (T2DM).1,4-7
Anthracycline treatment may induce dilated cardiomyopathy, subclinical left ventricle dysfunction, congestive heart failure and arrhythmia. Cardiomyopathy may develop in one of three forms: 1) an acute/subacute form, immediately after anthracycline administration, manifesting as transient arrhythmia, pericarditis/myocarditis syndrome, or left ventricular failure and generally reversible; 2) a chronic form, presenting within one year of treatment, and 3) a late onset, with ventricular dysfunction and arrhythmia developing years after treatment. The two last forms are dose-dependent.2 CCS present clinical and subclinical toxicity at lower levels than adults. Younger age at diagnosis (particularly inferior to five years), female gender, combination therapy with other agents, mediastinal radiation, previous pre-morbid/co-morbid medical conditions (obesity, congenital heart disease, cardiac disease: coronary, valvular or myocardial, hypertension, diabetes mellitus, dyslipidemia) are associated with increased risk of anthracycline-related cardiomyopathy.2-8
Hematopoietic stem cell transplantation is associated with increased risk for CVD mortality and morbidity related to cardiomyopathy, congestive heart failure, cerebrovascular accident, CAD, rhythm disorders, hypertension, T2DM, and dyslipidemia.3
Additionally, CCS have higher rates of impaired glucose tolerance, T2DM, insulin resistance, and dyslipidemia, as well as increased risk of renal insufficiency and hypertension due to nephrotoxic medications, radiation to the abdomen, and graft-versus-host disease.3-10
Recommendations for CV assessment in pediatric cancer patients at diagnosis and follow-up state that initial evaluation should include clinical evaluation with identification of CV risk factors, electrocardiogram (ECG) and echocardiogram (ECHO), or cardiac magnetic resonance imaging if necessary. Periodic follow-up is required during treatment, according to clinical situation. After treatment patients should be monitored regularly and a complete history and physical examination is mandatory, with control of CV risk factors (e.g. diet, physical activity, smoking habits, drug use, physical activity).1,2,4,7-10
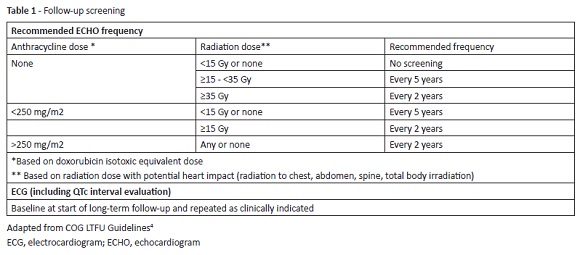
ECHO screening or comparable imaging assessment of cardiac function and ECG (with QTc interval evaluation) is recommended, according to Table 1.4,11
Biomarkers, as cardiac troponin I and troponin T, B-natriuretic peptide (BNP), and T-pro-B-natriuretic peptide (proBNP), are also useful, combined with history, physical examination and cardiac imaging to monitor patient’s clinical status.1,2,4,6-10,12
Cardiology consultation is necessary in patients with subclinical abnormalities on screening evaluation, left ventricular dysfunction, valvular disease, dysrhythmia, or prolonged QTc interval.4
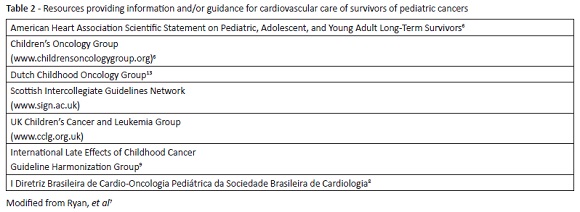
Medical societies and other organizations have produced guidelines, consensus statements and position papers regarding cancer survivor surveillance and monitoring; the majority concerns the adult population, but some are directed at the pediatric population and/or adult survivors of pediatric cancers (Table 2).
In conclusion, CCS exposed to cardiotoxic therapy require long-term cardiac follow-up and monitoring. Nonpharmacological measures, such as exercise, healthy lifestyle, risk factor control, and treatment of comorbidities, are important in this population at high risk for premature CV disease. As manifestations can occur years to decades after exposure, this is a difficult issue: patients must be informed of the potential cardiotoxicity risks and consequences and provided with adequate follow-up in clinical practice. A coordinated effort among pediatric and adult oncologists and cardiologists is necessary to define best practices and improve outcomes for this patient population.
REFERENCES
1. Kleinmahon JA, Landeck BF. Evaluation and Long-Term Outcomes of Cardiac Toxicity in Paediatric Cancer Patients. In: Karen Wonders, Brittany Stout editors. Pediatric Cancer Survivors. Croatia; 2017. p. 65-78. DOI: 10.5772/67043. [ Links ]
2. Shankar SM, Marina N, Hudson MM, Hodgson DC, Adams MJ, Landier W, et al. Monitoring for cardiovascular disease in survivors of childhood cancer: report from the Cardiovascular Disease Task Force of the Children’s Oncology Group. Pediatrics 2008; 121:e387-96. [ Links ]
3. de Ferranti SD, Steinberger J, Ameduri R, Baker A, Gooding H, Kelly AS, et al. Cardiovascular Risk Reduction in High-Risk Pediatric Patients: A Scientific Statement from the American Heart Association. Circulation 2019; 139:e603-34. [ Links ]
4. Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, Version 5.0. Monrovia, CA: Children’s Oncology Group. October 2018. Disponível em: https://www.survivorshipguidelines.org/. [ Links ]
5. Westerink NL, Nuver J, Lefrandt JL, Vrieling AH, Gietema JA, Walenkamp AME, et al. Cancer treatment induced metabolic syndrome: Improving outcome with lifestyle. Crit Rev Oncol Hematol. 2016; 108:128-36. DOI: 10.1016/j.critrevonc.2016.10.011. [ Links ]
6. Lipshultz SE, Adams MJ, Colan SD, Constine LS, Herman EH, Hsu DT, et al. Long-term cardiovascular toxicity in children, adolescents, and young adults who receive cancer therapy: pathophysiology, course, monitoring, management, prevention, and research directions: a scientific statement from the American Heart Association. Circulation. 2013; 128:1927-95. DOI: 10.1161/CIR.0b013e3182a88099. [ Links ]
7. Ryan TD, Nagarajan R, Godown J. Cardiovascular Toxicities in Pediatric Cancer Survivors. Cardiol Clin. 2019; 37:533-44. DOI: 10.1016/j.ccl.2019.07.002. [ Links ]
8. I Diretriz Brasileira de Cardio-Oncologia Pediátrica da Sociedade Brasileira de Cardiologia. Arq Bras Cardiol. 2013; 100:1-68. [ Links ]
9. Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine, LS, Dwyer M, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015; 16:e123-36. DOI: 10.1016/S1470-2045(14)70409-7. [ Links ]
10. Armstrong GT, Oeffinger KC, Chen Y, Kawashima T, Yasui Y, Leisenring W, Stovall M, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013; 31:3673-80. DOI: 10.1200/JCO.2013.49.3205. [ Links ]
11. Wong FL, Bhatia S, Landier W, Francisco L, Leisenring W, Hudson MM, et al. Cost-effectiveness of the children’s oncology group long-term follow-up screening guidelines for childhood cancer survivors at risk for treatment-related heart failure. Ann Intern Med. 2014; 160:672-83. DOI: 10.7326/M13-2498. [ Links ]
12. Wolf CM, Reiner B, Kühn A, Hager A, Müller J, Meierhofer C, et al. Subclinical Cardiac Dysfunction in Childhood Cancer Survivors on 10-Years Follow-Up Correlates with Cumulative Anthracycline Dose and Is Best Detected by Cardiopulmonary Exercise Testing, Circulating Serum Biomarker, Speckle Tracking Echocardiography, and Tissue Doppler Imaging. Front Pediatr. 2020; 8:123-34. DOI: 10.3389/fped.2020.00123. [ Links ]
13. Sieswerda E, Postma A, van Dalen EC, van der Pal HJH, Tissing WJE, Rammeloo LAJ, et al. The Dutch Childhood Oncology Group guideline for follow-up of asymptomatic cardiac dysfunction in childhood cancer survivors. Ann Oncol. 2012; 23:2191-98. DOI: 10.1093/annonc/mdr595. [ Links ]