Introduction
Pica refers to the persistent, compulsive craving for and ingestion of substances usually considered inedible. This behavior should be discordant with cultural practices and continue beyond the normal developmental phase of occasional indiscriminate and experimental mouthing and swallowing for at least one month (Box 1). An age cut-off of 24 months or more is suggested in the The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).9 The term originated from the Latin word for magpie, “pica”, a bird famed for collecting and hoarding unusual objects.2
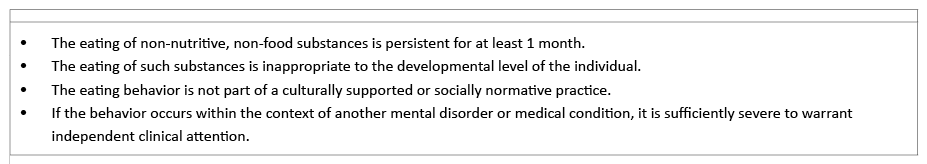
Box 1 The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for the diagnosis of pica1
Pica is considered a common, dangerous, and potentially life-threatening behavior in children, as it can lead to multiple complications, like chocking, intestinal obstruction/perforation, mucosa damage, poisoning, and infection, among others.2,3
Although epidemiological data in the literature about the exact pica prevalence is scarce, it seems to be more common during childhood, mainly at the ages of two to three years.3. Pica may persist into adolescence when associated with intellectual disability or manifest during pregnancy.3 Studies suggest that pica can be present in 5 to 25% of children with learning difficulties and its prevalence correlates with disability severity.4
Pica etiology is poorly understood and a wide range of explanatory mechanisms have been put forward. It has been conceptualized as a response to hunger or as oral gratification for anxiety and emotional stress relief in children.5 Additionally, associations with micronutrient deficiency, including iron, calcium, and zinc, and with sickle cell anemia have been reported.3,6
Psychiatric comorbidities, such as obsessive-compulsive disorder, depression, and anorexia nervosa are often reported.7 Several authors describe pica as an impulse control disorder and propose that it may appear in response to poor impulse control and within the obsessive-compulsive spectrum.8
Pica generally resolves in children of average intelligence after they have been trained to discriminate between edible and nonedible items and proper supervision has been provided.2.Besides behavioral interventions, little is known regarding other therapeutic interventions, including pharmacological treatment. In some cases, vitaminic or mineral supplementation or treatment with selective serotonin reuptake inhibitors may be prescribed.2,3
Attention deficit hyperactivity disorder (ADHD) is characterized by patterns of inattention and/or hyperactivity/impulsivity. It is likely caused by a dopaminergic dysfunction and responds to psychostimulant treatment.9 As impulsive symptoms are part of the diagnostic criteria for ADHD, which is identified as an inhibition and impulse control problem as described for pica, in this study the authors review the available literature on pica, ADHD, and treatment response during childhood and adolescence and present two case reports, with the aim of investigating the clinical overlap and treatment outcomes of these two disorders.7,8
Methods
A systematic literature review was conducted on PubMed and Cochrane databases during November 2019 using the key terms “pica”, “attention deficit”, “hyperactivity”, “child”, and “adolescent”. The search strategy included reviews and case reports and yielded 28 results. Abstracts of retrieved articles were screened and manual selection of papers was subsequently performed based on their relevance for the subject in matter. A total of 12 eligible records were identified. Six other records were additionally identified through referencing in those initially retrieved in the literature search. No restriction criteria were established regarding study design. Only articles written in English were considered.
Additionally, a retrospective analysis of two patients with pica and ADHD from the Child and Adolescent Psychiatry Department of Hospital Pediátrico was also conducted.
Results
To date, only three cases have been reported in the literature describing children with diagnosis of pica and ADHD (or hyperkinetic disorder; Table 1). Of these, two were male, two had average intelligence quotient (IQ), and two had normal blood work. The only two case reports of children with pica and ADHD with no intellectual disability or blood deficit had complete pica symptom remission after methylphenidate treatment.
Gunes et al. reported the case of a six-year-old girl with pica and ADHD with complaints of eating substances with no nutritive value − like hair, fibre, slime, play dough, toothpaste, ice, paper, wood, and glue − since her toddlerhood.10 This girl met DSM-IV criteria for ADHD. Physical and neurologic examinations and complete blood work revealed no abnormalities and she had an average IQ.11 The girl was prescribed 10mg of methylphenidate twice daily, with improvement in attention deficit, hyperactive, and impulsive behaviors and pica symptoms after four weeks and proper functioning during the following year.
Table 1 Cases of Pica and ADHD reported in the literature

ADHD, attention deficit hyperactivity disorder; IQ, intelligence quotient
Also Hergüner et al. described the case of an eight-year-old boy with pica and ADHD as comorbidity, both successfully treated with methylphenidate.12 The boy presented with complaints of eating carpet and cloth fibres for more than three years and met DSM-IV criteria for ADHD. He described this habit as a strong, irresistible impulse, which he could not resist to. Although the boy did not like this feeling and did not want to eat, he was unable to overcome it. In psychiatric assessment, he showed inattention, hyperactivity, and impulsivity. He had aggressive behavior towards his parents and peers, concentration problems, poor school performance, and increased motor activity. Obsessive, compulsive, anxiety, and/or depressive symptoms were not identified. Psychometric testing revealed normal intelligence level and medical history was unremarkable. Full laboratory examinations were within normal limits. The boy was diagnosed with pica and ADHD (combined type) according to DSM-IV.11 OROS methylphenidate 27mg daily was prescribed, with both ADHD and pica symptom improvement within three weeks. The boy remained symptom-free for six months.
Gautam et al. described a 12-year-old boy with hyperkinetic disorder and pica. According to the multiaxial International Classification of Diseases (ICD-10), the patient was also diagnosed with moderate mental retardation and iron deficiency anemia, both typically associated with pica symptoms.13,14 He started on fluoxetine 20mg once daily due to nail-biting behavior and iron supplementation. Initial management of hyperactivity symptoms was conducted with behavioral modification techniques and special education was planned, with gradual improvement of pica behavior and nail biting habits on subsequent follow-ups.
Retrospective analysis of pica patients at the Child and Adolescent Psychiatry Department of our institution further identified two cases of children with pica and ADHD and average IQ (Table 2).
Case 1 was a ten-year-old girl referred to our outpatient clinic with complaints of difficulty in paying and keeping attention and focusing at school. She had difficulties in maintaining school activities for frequently talking with peers during class and presented poor school performance and increased motor activity. The girl had been diagnosed with ADHD at the age of eight years and was on methylphenidate short-acting formulation of 20mg + 10mg daily at the time of referral. The mother described nail-biting behavior and the recurrent habit of chewing and eating paper sheets since the first year of school and particularly during the last few months. The girl also frequently nibbled at some school materials, like pencils and pens. Psychometric tests revealed an IQ corresponding to average intelligence level. Growth and physical development were normal (weight and height between the 25thand the 50thpercentile). Laboratory examinations, including complete blood count, serum ferritin, iron, zinc, vitamin B12, and folate levels, and liver, thyroid, and renal function tests were within normal range. There was no history of pica or other psychiatric disorders among family members. Due to lack of adherence and response to previous treatment, the girl was stared on 27mg of OROS methylphenidate formulation, with improvements in school and no ingestion of non-nutritive materials within four weeks.
Table 2 Pica and ADHD cases reported at the Child and Adolescent Psychiatry Department of Hospital Pediátrico
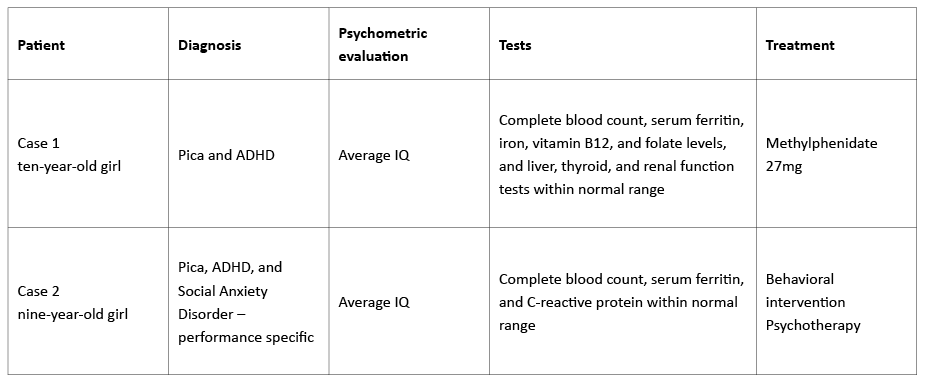
ADHD, attention deficit hyperactivity disorder; IQ, intelligence quotient
Case 2 was a nine-year-old girl referred to our outpatient clinic by the family doctor due to habits of eating pens, crayons, pencils, glue sticks, and paper, as well as biting nails since infancy. However, she was only referred to specialty appointment when the mother noticed colored stools due to ingestion of wax crayons. The child described this habit as a strong impulse to which she could not resist and which worsened during school test period. She was ashamed of this behavior, which she felt unable to overcome. Parents and teachers also complained about her fidgeting behavior. In psychiatric assessment, the girl exhibited inattention, hyperactivity, and impulsivity symptoms and met ADHD criteria. She also feared being negatively judged by peers in school and met Social Anxiety Disorder criteria. Physical and neurologic examinations and complete blood work were normal and IQ was average. The girl started a multidisciplinary intervention based on behavioral training and psychotherapy to reduce pica and performance-related anxiety symptoms. Due to parental refusal, no pharmacological intervention directed at ADHD symptoms was initiated. Although she still reports difficulties in concentrating and behaving well in class and maintains some nail-biting behaviors, her pica and performance anxiety symptoms improved after behavioral intervention.
Discussion
Little is yet known about pica etiology and treatment. Due to poor impulse control, several authors have conceptualized it as lying within the spectrum of compulsive-impulsive disorders. As in ADHD, impulsivity seems to be a cardinal pica feature.
There is a general impression among clinicians that children with ADHD often present comorbid pica at some point in their lives. However, pica is seldom diagnosed, possibly due to the generalized notion that its symptoms vanish with ADHD improvement through psychotherapeutic or, more frequently, psychopharmacologic interventions, namely methylphenidate.
Only single cases of comorbid pica and ADHD in young patients have been reported in the literature and, although a few authors have reported this association for over a decade, its prevalence is still largely unknown. Some children with comorbid pica and ADHD treated with methylphenidate have an excellent pharmacological response regarding both conditions, which seems to support the dopaminergic system dysfunction theory regarding pica etiology.
Some authors report the exacerbation of pica symptoms with thioridazine, which is well known for its anti-dopaminergic actions.15 Also, one study reported a higher incidence of pica symptoms in patients receiving typical antipsychotic medication.16 Other authors describe a reduction in pica symptoms with bupropion, an antidepressant acting as a norepinephrine and dopamine reuptake inhibitor, in developmentally disabled adults.17 These data may also support the potential role of dopaminergic system dysfunction in the etiology of this condition.
In this study, the authors analysed clinical data and physiopathological cues available in the literature regarding pica and ADHD and added two clinical cases from their institution reporting a decrease in pica symptoms after ADHD assessment and treatment. Despite being independent clinical conditions, retrieved data suggests that pica and ADHD may share some neurobiological ground. Specifically, a subgroup of pica cases may be related to impulse control problems or dopaminergic system dysfunction and methylphenidate may be a reasonable treatment option for these patients.
Due to the still limited available evidence regarding pica and ADHD, it is necessary to increase the scientific and clinical body of evidence regarding this subject. Simultaneously, clinician’s awareness about this association and reporting of cases identified is crucial to support further studies and research in this area.














