Introduction
Folic acid is a substrate in the intracellular methylation reactions essential to normal brain development and function. Methylation is important in deoxyribonucleic acid (DNA) synthesis, stability, and repair, gene expression, neurotransmitter synthesis and destruction, and in homocysteine metabolism.1,2
Folic acid deficiency is one of the most widespread nutritional deficiencies worldwide, with acknowledged adverse health consequences.1 Folic acid deficiency may contribute to the pathogenesis of neuropsychiatric disorders, including memory loss, cognitive development delay, mood disorders, delirium, and psychotic disorders.3
Vitamin B12, also called cobalamin, is the only vitamin of the human body containing cobalt and functions as a cofactor for methionine synthetase.4 Vitamin B12 deficiency is associated with neurologic, psychiatric, and neuropsychiatric disorders, including neuropathy, myelopathy, myeloneuropathy, cerebellar ataxia, optic atrophy, and cognitive disorders, as dementia, psychosis, and mood disorders.5-7
There are multiple reasons for the simultaneous study of folic acid and vitamin B12 deficit, including the close relationship between the metabolic pathways of the two vitamins and the comorbidities associated with the neuropsychiatric syndromes that both can elicit.6
Both vitamins have an essential role in the central nervous system functioning at any age, particularly in the homocysteine to methionine conversion, which is mediated by methionine synthetase and a crucial step for nucleotide synthesis and for gene and non-gene methylation.6
One-carbon metabolism (OCM) is essential for nucleotide synthesis of DNA and other molecules. This cycle is an intricate system involving transfer of a methyl group amongst multiple conformations.2
The primary cause of OCM alterations is impaired folic acid and vitamin B12 levels. One of the best understood consequences of this is an increased level of homocysteine, a highly toxic metabolite for neural and vascular development.8
The 2009 study by Kale et al had already sustained OCM changes in early psychosis, stating that it might have implications on psychosis neurodevelopmental pathophysiology, progression, and treatment.9 These changes, which include increased homocysteine and decreased folic acid and vitamin B12 serum levels, are hence frequently reported in patients with first-episode psychosis (FEP).9-11
Multiple studies throughout the years have associated folic acid and vitamin B12 deficiency with psychiatric disease, particularly schizophrenia, although not consensually.5,8-25 However, as far as we are aware, no study to date has related such vitamin deficiencies with isolated psychotic disease and independently of the individual’s psychiatric diagnosis, specifically in children and young adults, during the acute phase. Therefore, the aim of this study was to retrospectively analyse the association between folic acid and vitamin B12 serum levels and psychotic symptoms in children and young adults hospitalized due to psychiatric disease.
Material and methods
This was a retrospective cohort study of inpatients from the departments of Psychiatry and Child and Adolescent Psychiatry of Centro Hospitalar e Universitário de Coimbra, in Portugal. The study included patients aged up to 25 years old, hospitalized from 2005 to 2018, with folic acid and/or vitamin B12 serum level measurements retrieved during hospitalization. Data from patients who fulfilled the above-mentioned inclusion criteria were retrieved from their medical records and included age, sex, presence or absence of psychotic symptoms during hospitalization, final diagnosis, folic acid serum levels retrieved during hospitalization, vitamin B12 serum levels retrieved during hospitalization, and occurrence of psychiatric rehospitalizations. The study had no exclusion criteria.
Patients enrolled were divided in two groups according to presence or absence of psychotic symptoms during hospitalization. To determine the presence of such symptoms, researchers looked for changes in thinking and/or sensory perception reported in the medical release note. Since this was a retrospective study, no scales or scores were systematically applied to evaluate psychotic symptoms.
Information regarding patients’ final diagnosis was also retrieved from the medical discharge note and compiled according to the nosological classification of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5TM) (American Psychiatric Association, 2013).26
Folic acid and vitamin B12 serum levels were determined from blood samples collected during hospitalization using an ADVIA Centaur immunoassay system (Siemens, Lisboa, Portugal). Direct competitive chemiluminescence immunoassay methods were performed to assess serum levels of both molecules. The expected variation of vitamin B12 serum levels in healthy subjects is between 211 and 911 pg/mL and of folic acid is > 5.38 ng/mL.
Participants’ anonymity was always assured, as well as confidentiality of all data collected throughout the study.
Data was analyzed using the Statistical Package for the Social Sciences (SPSS) version 23.0 software.
The Kolmogorov-Smirnov normality test was used for distribution analysis of continuous quantitative variables, followed by non-parametric Mann-Whitney U test and Spearman’s Correlation test. Qualitative variables were analyzed using the Chi-Square Independence (χ2) test.
Statistically significant differences were assumed for p values < 0.05. These were marked with * on tables.
Results
A total of 165 patients were included in this study and divided in two groups: patients with psychotic symptoms during hospitalization (PS group; n=83) and patients without psychotic symptoms during hospitalization (nPS group; n=82).
PS group included 61 males (73.5%) and 22 females (26.5%), with an average age of 20.7 years (ranging from 12 to 25 years). nPS group included 33 males (40.2%) and 49 females (59.8%), with a similar average age of 20.7 years (ranging from 12 to 25 years).
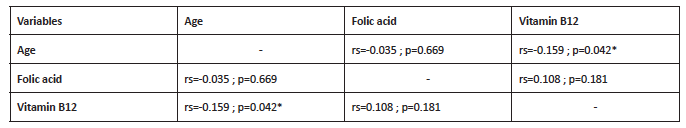
Patients’ final diagnosis was organized in 11 different groups, according to the DSM-5TM nosological classification (Table 1). In the PS group, most individuals were diagnosed with Schizophrenia Spectrum and Other Psychotic Disorders (75.91%), with 24.09% having other diagnoses (Depressive Disorders, Bipolar and Related Disorders, Personality Disorder, Neurodevelopmental Disorders and Substance-Related and Addictive Disorders). In the nPS group, the distribution of diagnosis across the nosological classification was wider, but no patients had Schizophrenia Spectrum and Other Psychotic Disorder (Table 1).
Table 1 Final diagnosis of patients included in the study, according to the DSM-5TM (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, American Psychiatric Association, 2013) nosological classification
nPS - group without psychotic symptoms; PS - group with psychotic symptoms
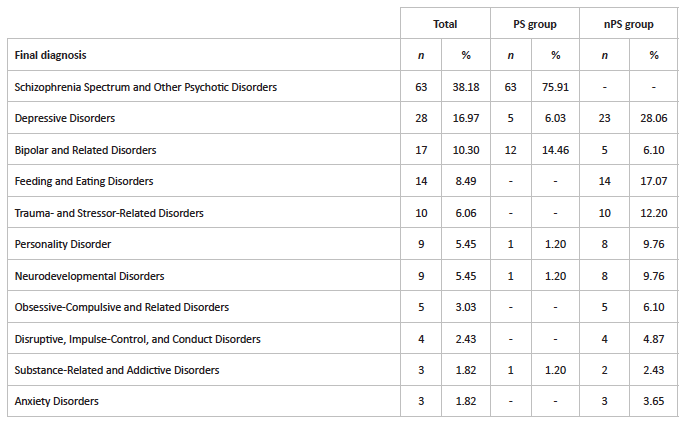
The nPS group displayed significantly higher serum folic acid levels than the PS group (p=0.01) (Table 3). Conversely, no statistically significant difference was found between both groups regarding serum vitamin B12 levels (p=0.30) (Table 2). Although folic acid and vitamin B12 serum levels were higher in females than in males, this difference was not statistically significant (p=0.28 and p=0.48, respectively) (Table 2). Regarding psychiatric rehospitalizations, both folic acid and vitamin B12 serum levels were lower in rehospitalized patients. Nonetheless, this was also a non-statistically significant difference (p=0.33 and p=0.27, respectively) (Table 2).
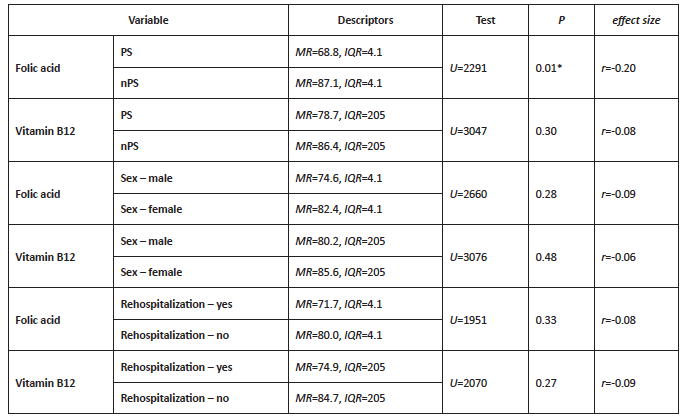
On one hand, a weak negative correlation was found between folic acid serum levels and age (rs=-0.035) and between vitamin B12 serum levels and age (rs=-0.159), although only the latter was statistically significant (p=0.042) (Table 3). On the other hand, a weak positive correlation was found between folic acid and vitamin B12 serum levels (rs=-0.108), which was not statistically significant (p=0.181) (Table 3).
Table 2 Association between psychotic symptoms and folic acid serum levels (µg/L), psychotic symptoms and vitamin B12 serum levels (pg/mL), sex and folic acid serum levels (µg/L), sex and vitamin B12 serum levels (pg/mL), folic acid (µg/L) serum levels and rehospitalizations (yes/no), and vitamin B12 (pg/mL) serum levels and rehospitalizations (yes/no)
IQR - interquartile range; MR - median of ranks; nPS - group without psychotic symptoms; PS - group with psychotic symptoms
Table 3 Correlation between folic acid serum levels (µg/L), vitamin B12 serum levels (pg/mL), and age (years)
rs - Spearman’s correlation coefficient
Lastly, a statistically significant association was found between presence of psychotic symptoms and rehospitalization (p=0.030), with patients with psychotic symptoms having a significantly higher probability of at least one rehospitalization (30%) than those without psychotic symptoms (16%) (Table 4).
Discussion
This study’s results show that folic acid serum levels are significantly lower in children and young adults hospitalized due to psychiatric disease associated with psychotic symptoms compared with same-aged psychiatric patients without psychotic symptoms. No statistically significant difference was found regarding vitamin B12 serum levels.
PS and nPS groups had a very similar patient number (83 and 82 patients, respectively) with the same age range (20.7 years on average for both groups). There was a male preponderance (73.5%) in the first group and a female preponderance in the second (59.8%). However, folic acid and vitamin B12 serum levels did not significantly vary with sex or age, contrarily to what happened with rehospitalizations. In this study, psychotic symptoms were found to increase the probability of at least one rehospitalization.
As far as we are aware, this is the first study directly investigating psychotic symptoms in youth independently of psychiatric diagnosis and testing their relationship with folic acid and vitamin B12 serum levels. In this sample, nPS group individuals also had an acute psychiatric disease and were hospitalized.
Patients’ final diagnosis was organized into eleven nosological groups according to the DSM-5TM. Although most patients in the PS group had Schizophrenia Spectrum and Other Psychotic Disorders (75.91%), 24.09% had other diagnoses (Depressive Disorders, Bipolar and Related Disorders, Personality Disorder, Neurodevelopmental Disorders and Substance-Related and Addictive Disorders). This was expected, since psychotic symptoms are frequently associated with Schizophrenia Spectrum and Other Psychotic Disorders and less common across other diseases. Still, these were included in the PS group and results were robust, suggesting that the presence of psychotic symptoms is apparently related to significantly lower folic acid serum levels in children and young adults, regardless of the diagnosis.
A study from 2006 described a high frequency of low folic acid levels in patients with a recent psychiatric hospitalization compared with healthy controls, but the presence or absence of psychotic symptoms was not assessed.15
A recent meta-analysis by Firth et al (2017) reported that, in patients with FEP, poor nutritional status, namely regarding folic acid, is independent and sometimes precedent of treatment with antipsychotics compared with healthy controls.12 These findings were compatible with an Indian study reporting low folic acid and vitamin B12 levels in untreated FEP patients.9 That study also showed that lower folic acid levels in those patients could not be attributed to dietary differences.9 On the other hand, in the study by Ayesa-Arriola et al (2012) folic acid and vitamin B12 levels did not differ amongst non-affective FEP patients and healthy controls, what makes the relationship between FEP and folic acid levels debatable in comparison with the general population without psychiatric diseases.11
Another meta-analysis had already reported folic acid and vitamin B12 deficiency in patients with schizophrenia, while a Korean study stated that high folic acid levels seemed to decrease the risk of this disease and a Dutch study found an increased risk of low folic acid levels.8,13,16,17,21 However, a clear association between folic acid levels and schizophrenia remains controversial.4,8,10,11,13,14,16,18,24
It should be noted that a statistically significant negative correlation was found between folic acid levels and severity of negative symptoms in a large number of non-smoking schizophrenic outpatients.19 The study by Song et al (2014) also found that low folic acid serum levels and high homocysteine serum levels were associated with more severe symptoms in schizophrenia, particularly on the negative symptom domain.14 This seems to support an association between low folic acid serum levels and severity of negative symptoms in schizophrenic patients. However, a different study did not find this association.11 The present study focused on positive rather than negative symptoms.
Low folic acid serum levels were also found in depressed patients.18 Conversely, Reif et al (2005) 25 found no statistically significant difference regarding folic acid or vitamin B12 in an ethnically homogeneous female population with different psychiatric disease, and Ipcioglu et al (2008)23 found no statistically significant effect of FEP or depression on folic acid or vitamin B12 serum levels, suggesting that patients did not differ from healthy controls.
Vitamin B12 deficiency has been reported to be frequent among hospitalized psychiatric patients, particularly with schizophrenia, with no hematological consequence for most of them.22 In the study by Jayaram et al (2013), psychiatric symptoms including schizophrenia, psychotic episodes, affective bipolar disorder, and depressive disorder were reported in patients with vitamin B12 deficiency, but psychotic symptoms were not independently assessed.20 Also in a recent study by Kapoor et al (2017), a higher prevalence of neuropsychiatric symptoms, including psychosis, was found in vegetarians, as well as an association with vitamin B12 but not with folic acid deficiency.5
In line with what was previously described regarding folic acid, also low vitamin B12 levels seem to be associated with more severe negative symptoms in schizophrenia.10 However, other studies report otherwise, with higher (but not statistically significant) vitamin B12 serum levels in patients with chronic schizophrenia.24
Except for Reif et al (2005), all studies referred to in this discussion selected healthy individuals as control group.25 In all of them, psychotic symptoms were not independently assessed, but rather the diagnosis of FEP, schizophrenia, depressive disorder, among others, or psychiatric disease in general, what precludes direct comparisons between those studies and the present one.
This study has several limitations that should be acknowledged. Firstly, it is a retrospective study with a relatively small sample of patients, and groups were not homogenized regarding sex. Secondly, no known exclusion criteria were applied regarding folic acid and vitamin B12, like smoking, alcohol ingestion, and exposure to certain drugs or specific genetic characteristics.2 Additionally, no further analytical parameters were collected concerning time from the first hospitalization day and folic acid and/or vitamin B12 serum levels assessment. Another limitation is the fact that the presence or absence of psychotic symptoms was only determined based on patients’ discharge note. Finally, a control group with healthy subjects was missing in this study.