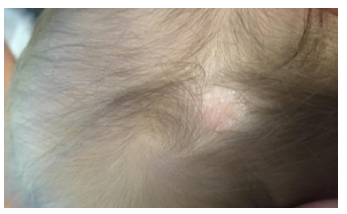
A full-term female infant born by vaginal delivery presented with an oval skin defect on the parietal scalp measuring 0.5x0.5 cm (Figure 1). Physical examination was otherwise normal, with no syndromic manifestations. Pregnancy and delivery were uneventful. The child had no family history of skin defects or congenital anomalies of any organ. Brain ultrasound revealed no abnormality and radiography showed no bony defect. The scalp lesion was conservatively managed, with complete epithelisation after several weeks. At eight-month follow-up, the girl was growing and developing normally and scar tissue had formed over the defect (Figure 2).
Discussion
Aplasia cutis congenita (ACC) is a rare malformation (present in 1 to 3 in 10,000 live births) characterized by localized absence of certain skin layers, mostly on the scalp, but potentially in any part of the body.1
ACC etiology remains unclear. It is likely multifactorial and includes genetic and exogenous factors (placental infarcts, teratogenic substances like methimazole, intrauterine infections, trauma, and neural tube defects).
The typical lesion is small (usually 1-2 cm, ranging from 0.5 to 10 cm), well-circumscribed, and may have different aspects (circular, oval, linear, stellate). ACC is often identifiable with a proper clinical exam, but lesions with similar presentation at birth should be considered and ruled out (traumatic lesion, scalp abscess, brain tissue heterotopic, and skull-spinal dysraphism).
ACC is usually an isolated finding, as in the present patient, but can be associated with other congenital anomalies, including Adams-Oliver syndrome, Bart syndrome, and Setleis syndrome.2 When accompanied by a skull or dura defect, ACC can cause brain and sagittal sinus exposure in addition to large vein exposure. This in turn increases the risk of infection, sagittal sinus thrombosis, and hemorrhage.3
Diagnosis is mainly clinical, but imaging studies are indicated in patients with large, irregular, or membranous lesions to assess underlying bone defects, brain anomalies, or vascular malformations. The clinical examination is classified into nine groups according to the number and localization of Frieden lesions, accompanying anomalies, and inheritance patterns.4 In the present case, ACC presented with no associated anomalies (group 1 of Frieden classification).
Given the high clinical presentation variability, the treatment approach must always be individualized.5,6 Treatment depends on the presence of complications and the infant’s condition and may consist of a conservative approach, surgery, or a combination of both. Management includes prevention and treatment of disease complications, such as infections, electrolyte imbalance due to epidermal water loss and bleeding, nutritional deficiency from chronic blood loss, and pain due to wound dressing.4 Traditionally, a conservative approach is used for small defects that heal uneventfully with gradual epithelization, as in the present case.1,5
In conclusion, ACC is mostly a benign isolated small scalp lesion without complications, and hence best treated conservatively. However, since it causes great anxiety for parents, its correct diagnosis and clinical follow-up are crucial, as well as genetic counseling when in presence of other conditions.