Introduction
Non-odontogenic cysts within the jaws are not a common finding, especially in pediatric age. It is well documented that cysts in the pediatric population tend to be developmental and odontogenic. (1) Nasolabial cyst is a rare development cyst, comprising only 0.7% of all jaw cysts. It occurs in the upper lip, laterally of the midline, or near the lateral and canine tooth junction. (1), (2) The pathogenesis of nasolabial cysts remains uncertain. Currently, the most widely accepted theory is that it originates from the inferior and anterior portion of the nasolacrimal duct. This theory is supported by the fact that the nasolacrimal duct is lined with pseudostratified columnar epithelium, also found in nasolabial cyst cavities. (3), (4) Clinically, nasolabial cysts are characterized by unilateral volume increase in the nasolabial region, causing an elevation of the nose wing, projection of the upper lip, and sometimes nasal obstruction. They present slow and asymptomatic growth. (2 Local pain and abrupt lesion enlargement may occur when associated with infection, which may be present in up to 50% of cases. (3), (4) The diagnosis is usually based on clinical course, with imaging tests valuable in assisting it. For being soft tissue lesions, nasolabial cysts are not visualized with traditional plain film radiographs. Traditional computed tomography (CT) or magnetic resonance imaging (MRI) show a soft tissue mass of varying size usually well demarcated. (1), (2
Treatment of nasolabial cysts can be accomplished through fine-needle aspiration, incision and drainage, cystic enucleation by intraoral access, endoscopic dorsal marsupialization, and intralesional injection of sclerosing agents. (1), (2), (4
Case report
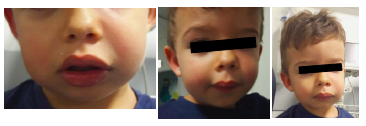
A 26-month-old male with a personal history of allergy to penicillin resorted to the Emergency Department for edema of the upper lip and left malar region with less than 24 hours of evolution and perception of progressive worsening, according to the mother. No other associated complaints or previous history of trauma or insect bite were reported. The patient had good general condition and no fever. Extraoral examination revealed facial asymmetry with rubor and edema of the upper lip, slight elevation of nasal ala, and deformity of the left nasolabial sulcus (Figures 1 and 2). A small and circumscribed fluctuant area in the maxillary region was detected on palpation. Observation by an otolaryngologist (ENT) revealed intraoral edema of the left oral vestibule and no intranasal alterations.
CT scan with intravenous contrast was performed, revealing a premaxillary left abscess with ipsilateral nasolabial phlegm (Figure 3). Based on clinical history and imagiological findings, diagnosis of infected nasolabial cyst was proposed.
Treatment with endovenous clarithromycin and clindamycin and systemic corticosteroid therapy with dexamethasone was initiated, and the patient was admitted to the Pediatric Department with progressive improvement of inflammatory signs. During hospitalization, stomatological observation discarded associated dental pathologies.
At discharge, the patient was completely asymptomatic and was referred to ENT consultation for follow-up. He remained asymptomatic, with no additional infectious episodes.
Discussion
Although nasolabial cyst is a rare diagnosis in children, this case illustrates the most common features in patients with this condition. Although the case refers to a male patient, nasolabial cysts are more frequent in females, according to the literature. (1)-(5 The differential diagnosis may include other lesions affecting the anterior maxillary region, such as odontogenic cysts and periapical abscesses and granulomas. (3)-(5 Pulp vitality testing of adjacent teeth is essential to confirm the diagnosis since coincidental dental lesions are a frequent cause of abscesses and require exclusion as a possible etiological factor. (3 In the present case, this differential diagnosis was excluded by stomatological observation. Other possible diagnoses, such as dermoid and epidermoid cysts, are usually associated with yellow discoloration of the overlying mucosa, whereas in nasolabial cysts, the mucosa preserves its normal pink hue or appears blue-tinged. (4
The traditional approach to this lesion in the adult population is surgical excision via intraoral/sublabial approach. (1 However, data regarding the best approach in pediatric age is scarce. Additionally, as nasolabial cysts are usually located near the nasal cavity floor, complications as nasal mucosa perforation during surgical excision are not uncommon. (3 In this case, given the patient’s age and favorable clinical evolution after resolution of the acute infectious process, a wait-and-watch attitude with regular follow-up was chosen as the preferential approach. In the future, surgical removal may be considered if the patient presents complaints or new infectious events.
Conclusion
Data in the literature and from the present case report suggest that, although nasolabial cysts are a rare finding in pediatric age, pediatricians, ENT, and dental practitioners should be aware of its key features and be able to distinguish it from other odontogenic lesions. More studies are required to determine the best approach for treating this condition in pediatric populations.