Introduction
β-lactams (BL) are the first-line therapy for community- and hospital-acquired bacterial infections.1 The vast knowledge of its pharmacokinetics, associated with a broad spectrum of activity and low toxicity, makes them the most used group of antimicrobials.2
The BL family includes penicillins, cephalosporins, carbapenems, monobactams, and beta-lactamase inhibitors. They are the antibiotic class most commonly reported to cause allergic reactions.3 However, after appropriate assessment, more than 90% of subjects reporting allergy can tolerate penicillin.4 This mislabel occurs because most reported reactions can be related to intolerance, benign viral rash, or drug-infection interactions.4
An incorrect penicillin allergy diagnosis excludes a highly effective therapeutic option, with a potential increase of side effects, microbial resistance, and risk of infection recurrence.5,6 Using the tools available for a correct diagnosis allows to safely use these antibiotics.7
Types of hypersensitivity reactions to antibiotics
BL can originate any of the four types of hypersensitivity reactions proposed by Gell and Coombs (Table 1), which account for the most frequent immune-related adverse drugs reactions.8-11
Table 1 Immunologic aspects of hypersensitivity reactions according to Gell and Coombs classification. (Adapted from Regateiro F. and Faria E).
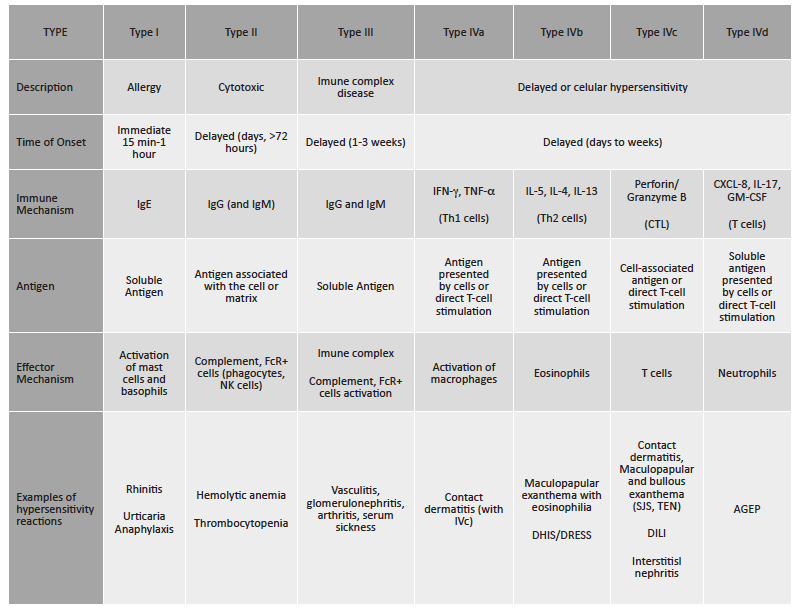
AGEP, acute generalized exanthematous pustulosis; DILI, drug-induced liver injury; DRESS/DiHS, drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms; FcR: Fc receptor; GM-CSF, granulocyte macrophage colony-stimulating factor; IFN-g, interferon-gamma; Ig, Immunoglobulin; IL, interleukin; NK, Natural Killer; SSJ, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis;TNF-a, Tumour necrosis factor alpha;
Immunoglobulin (Ig) E-mediated hypersensitivity reactions (Gell and Coombs type I) generally occur within one hour after drug administration. The drug or drug-protein complex is recognized by IgE antibodies bound to their high-affinity receptor on the surface of mast cells and basophils. Crosslinking of IgE leads to degranulation and release of a variety of pre-formed (histamine, triptase) and newly synthesized (leukotrienes, TNF-) mediators. Mediators are responsible for clinical manifestations, namely cutaneous (itching, hives, angioedema, generalized erythema), respiratory (rhinitis, laryngeal angioedema, wheezing), gastrointestinal (abdominal pain, nausea, vomiting, diarrhea), cardiovascular (tachycardia, hypotension), and in most severe cases, anaphylaxis with or without shock.10,12
Delayed hypersensitivity reactions are mostly mediated by T cells.10,12 Antibody-mediated reactions (Gell and Coombs types II and III) are uncommon. T-cell-mediated reactions (Gell and Coombs type IV) commonly occur after several days of treatment. The most common manifestations are maculopapular exanthema and delayed urticaria, and the most serious include severe cutaneous adverse reactions (SCAR), such as Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms syndrome, and acute generalized exanthematous pustulosis.10,12,13
Penicillins and cephalosporins: molecular structure
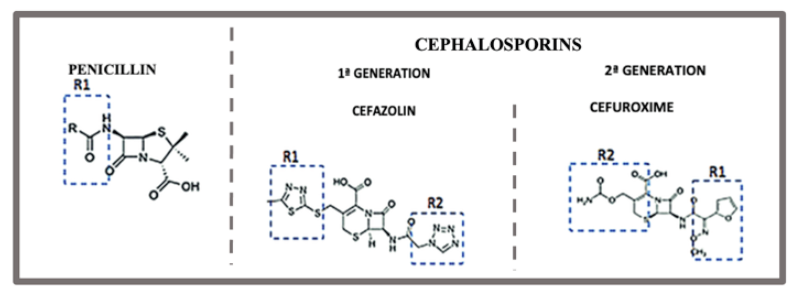
Penicillins and cephalosporins have similarities in their chemical structure.14,15 Both share a common -lactam ring, but penicillins have a 5-membered thiazolidine ring, and cephalosporins a 6-membered dihydrothiazine ring attached to the BL nucleus.16 The type and position of side chains differentiate penicillins and cephalosporins (Figure 1).17
The side chain is an important site of immunological recognition and hence of allergic cross-reactivity.17,18
Penicillins have low molecular weight; hence they must covalently bind to transport macromolecules to form a hapten-carrier complex in order to induce an immune response.12 Under physiological conditions, the penicillin central nucleus spontaneously opens, without defragmenting, binds to transport proteins, and forms the major antigenic determinant (penicilloyl polylysine).18-20
But the major antigenic determinant alone is insufficient to explain all penicillin-specific immune responses.18-20 A small proportion of penicillins (approximately 5%) are metabolized by other paths, and the resulting antigens are known as minor determinants (benzyl penicillin, penicilloate, and peniloate).18,20
Regarding cephalosporins, the process by which a hapten-protein complex is formed is unknown.21,22 Unlike penicillins, the central nucleus is extremely unstable and undergoes rapid fragmentation, resulting in unstable metabolites that do not enable protein haptenization. The haptenic determinants in cephalosporins are thus unknown.16,23
Apart from the central structure, side chains are important inductors of immunologic response.24 The R1 side chain remains intact and is the major responsible for cross-reactivity, while the R2 side chain makes little contribution to cephalosporin hypersensitivity.25
In both compounds, the reactivity of the native molecule must be investigated. However, in the case of penicillins, it is also important to investigate the immunogenicity of major and minor antigenic determinants resulting from their metabolism.26
Epidemiology
The most common side effects of BL in children are skin manifestations. Nevertheless, only a small number of these reactions are due to hypersensitivity mechanisms. Other probable causes are the coexistence of viral infections or reactions associated with other non-immunological mechanisms.27,28
The prevalence of self-reported reactions to BL in pediatric age varies from 1.7% to 5.2%,29-31 with amoxicillin (1.4%), other penicillins (1.2%), and cephalosporins (0.7%) being the most implicated drugs.29-31 Although IgE-mediated reactions are not uncommon, anaphylaxis is rare (approximately 0.015─0.004% for penicillins and 0.1─0.0001% for cephalosporins).4,32
Allergy to cephalosporins is generally managed in the context of patients with penicillin allergy.27 A 2012 literature review reported a 2.5% prevalence of cross-reactivity between penicillins and cephalosporins with similar side chains.33
Cross-reactivity
The cross allergy between penicillins and cephalosporins was assigned to the BL ring for decades, whereas side chains were associated with less relevant allergies.16 With the increasing knowledge of their molecular structure and metabolism and absence of cross-reactivity between antibiotics with the same ring, attention for the role of side chains in allergic reactions was raised.22 Nowadays, it is generally accepted that cross-reactivity is primarily determined by the R1 side chain.24,34,35
Regardless of the knowledge about the role of side chains, the risk of cross-reactivity between these agents has been overestimated in older studies. Before 1980, first-generation cephalosporins were produced by chemical modification of the penicillin structure, resulting in high levels of contamination.14 Additionally, some patients treated with penicillin developed IgG and IgM antibodies against cephalosporins with no clinical significance.33,36
Pichichero et al. conducted a metanalysis showing that patients allergic to penicillin had an increased risk of allergic reactions to first-generation cephalosporins, but cross-allergy was negligible with second- and third-generation counterparts.23 A prospective observational study in a pediatric population (n=664) with positive skin test for penicillin revealed cross-reactivity among molecules dependent on cephalosporin generation. A total of 23.9% of the allergic population in this study developed reactions to first- and second-generation cephalosporins, while only 0.3% presented manifestations to third- and fourth-generation molecules.37 In a meta-analysis of articles published between January 1980 and March 2019 estimating the risk of cross-reactivity to cephalosporins in patients with a proven IgE- or T-cell-mediated penicillin allergy, the rate of cross-reactivity varied with the degree of similarity between R1 side chains.38 This set of studies associated differences in cross-reactivity to a higher similarity between R1 side chains of the respective agents.23,37,38
Cross-reactivity between agents whose side chains are similar but not identical is also possible and has been documented, being presumably attributed to similar three-dimensional structure and physicochemical properties.18,24,39 Table 2 depicts the pharmacological groups exhibiting cross-reactivity due to identical and similar side chains, respectively.14,18,27,40
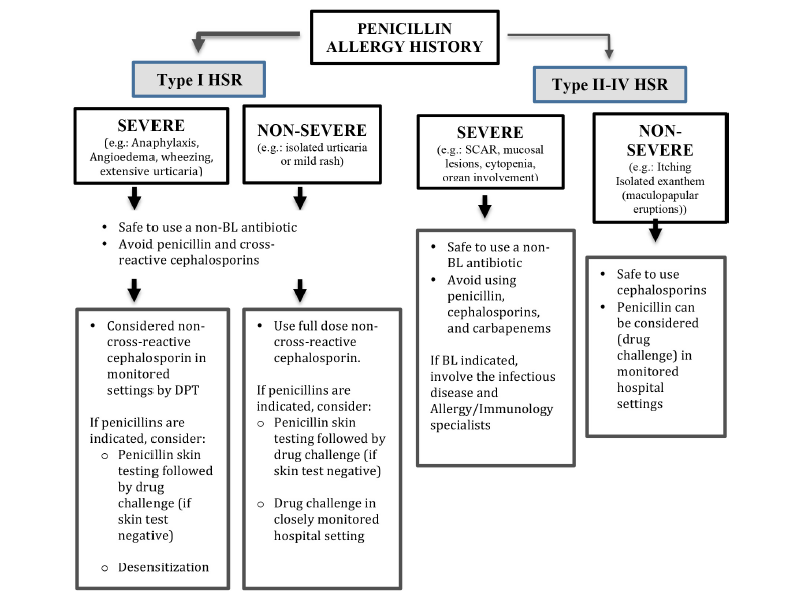
In patients allergic to penicillin, recent studies recommend the use of cephalosporins depending on the development and severity of clinical manifestations (Figure 2).4,11 While the use of first-generation cephalosporins should be avoided in patients allergic to penicillin, the risk of cross-reactivity to third- or fourth-generation cephalosporins is limited.11,27,41
Table 2 Penicillins and cephalosporins with identical or similar side chain (Adapted from Min-Hye Kim et al.)
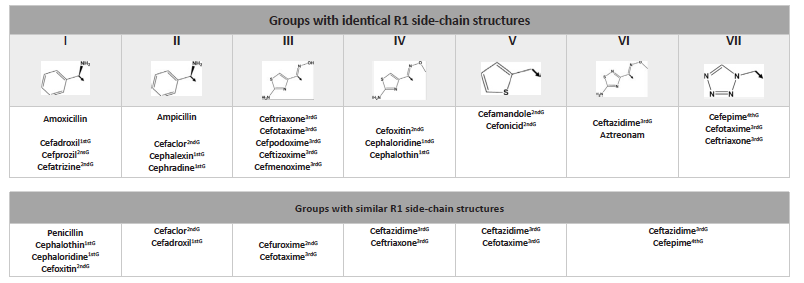
G, generation
Diagnosis
The evaluation of patients with antibiotic allergy begins with a careful history, including clinical manifestations, treatment of the allergic reaction, timing of the reaction, and details of the drugs used.42,43
The study should be conducted within a period of at least four to six weeks after the suspected allergic reaction.22 Assessment of IgE-mediated penicillin allergy should start with skin testing.44
For immediate reactions, a skin prick test and intradermal test with immediate reading can be considered.4 Penicillin skin testing is usually performed with major antigenic determinants (penicilloyl polylysine), minor determinant mixture, ampicillin or amoxicillin, and benzylpenicillin.26 Drug tests are compared with positive (histamine) and negative (usually glycerinated saline) controls.4
In patients with a negative penicillin skin test, the absence of immediate allergy should be confirmed by an oral drug provocation test (DPT, also named graded challenge) with the culprit drug.26,42 DPT consists of administering the drug in a graduated manner under close surveillance. The starting dose is usually 1/100 or 1/10 of the single therapeutic dose,43 after which the patient is observed for at least 30─60 minutes. If no adverse reaction is observed, increasing doses are administered until the full therapeutic dose.4,22,43
Skin test and DPT together have a negative predictive value for excluding IgE-mediated penicillin allergy of more than 99%.44
Patients with a history of severe allergic reactions, positive penicillin skin test, or DPT may cross-react with cephalosporin. Due to structural and molecular differences in these drug classes, skin test to penicillin does not predict cephalosporin allergy. Nonetheless, if the cephalosporin has a similar side chain, skin test may have diagnostic value.20,45 Therefore, some clinicians additionally perform skin test using a cephalosporin with a different side chain.44 Patients with negative cephalosporin skin test can perform a cephalosporin graded challenge.22
Testing for non-immediate reactions is not standard. Delayed intradermal or patch test reading can be used but is associated with low sensitivity and poor negative predictive value.43 If negative, DPT can be considered for non-SCAR T-cell-mediated hypersensitivity. In delayed reactions, DPT can be continuously used, being contraindicated for severe T-cell-mediated reactions.11,44
Conclusion
BL represent the first-line treatment of several bacterial infections and are the most frequent cause of hypersensitivity drug reactions.1 Clinical manifestations are heterogeneous, ranging from mild to severe and from immediate to delayed.10,12
When investigating the potential for cross-reactivity, the drugs’ molecular structure and metabolism under physiological conditions should be considered. The current evidence indicates that similarity between R1 side chains is the main cross-reactivity inducer, advising against the use of first-generation cephalosporins with similar side chains in patients with a history of allergic reaction to penicillin. Limited cross-reactivity is reported to third- or fourth-generation cephalosporins.