A previously healthy 15-year-old male was admitted to the Emergency Department with steady and progressively worsening abdominal pain in the right lower quadrant (RLQ), accompanied by anorexia with 12 hours of evolution.
On admission, he was afebrile, and the physical examination revealed good general condition, soft abdomen with localized tenderness in RLQ without significant rigidity, and positive Blumberg and Rovsing signs. The remaining physical exam was normal. As the clinical picture suggested acute appendicitis, preoperative assessment was performed, excluding difficult airway and cardiopulmonary abnormalities.
Urgent laparoscopic appendectomy was performed under general anesthesia, without complications during endotracheal intubation or mechanical ventilation. The patient remained hemodynamically stable, with normal urine output and minimal blood loss, and 150 mL of 0.9% saline solution were administered during the unremarkable 55-minute surgical procedure.
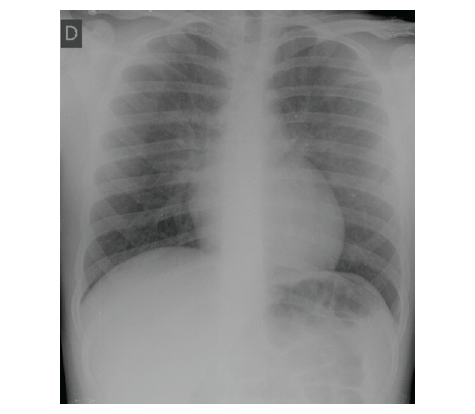
Immediately after extubation, during which no vomit or aspiration were observed, the patient developed hypoxemia (SpO2 82%), intense productive cough (requiring aspiration of clear frothy secretions), tachypnea, and subcostal retractions, requiring additional O2 (FiO2 40% using Venturi mask). Blood pressure was 135/60 mmHg, and heart rate was 70 bpm. He was sleepy yet easily awakened, with proper peripheral perfusion and normal central and peripheral pulse, no edema, and normal cardiac auscultation. Thorax expansion was symmetrical and pulmonary auscultation showed symmetrical decreased breath sounds with dispersed fine crackles. Arterial gasometry showed pH 7.36, pCO2 45 mmHg, pO2 48 mmHg, HCO3 - 26.8 mmol/L, and BE -0.5 mmol/L and chest radiograph revealed bilateral diffuse opacities with ill-defined edges (Figure 1). Cardiac evaluation was normal, showing no arrhythmias in the electrocardiogram, left ventricle overload pattern or ST-T changes, and four balanced-size chambers, normal left systo-diastolic ventricular function, normal left atrial filling pressure, normal aortic flow, and no pulmonary hypertension in transthoracic echocardiography.
Forty milligrams of intravenous furosemide were administered with the previously described oxygen supplementation, with quick clinical recovery and improvement in gasometric parameters and chest radiograph findings (Figure 2).
Treatment with intravenous furosemide in decreasing dosages and oxygen supplementation in decreasing flow rates were maintained for approximately 50 hours. Due to favorable evolution, the patient was discharged four days after surgery, asymptomatic and with normal chest radiography results.
What is your diagnosis?
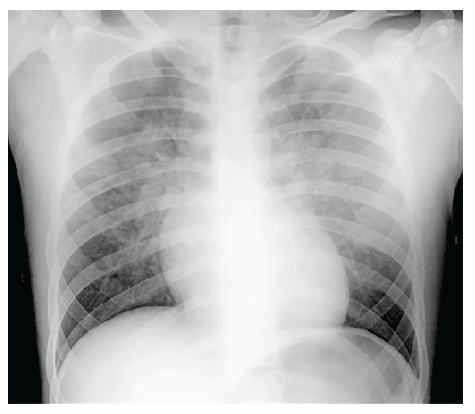
Figure 1 Antero-posterior chest radiograph few minutes after the onset of respiratory distress, showing bilateral diffuse opacities with ill-defined edges
Discussion
Post-extubation acute pulmonary edema (PEAPE) is an uncommon complication of tracheal extubation, occurring in 0.1% of patients undergoing general anesthesia.1-4 It has rarely been reported in pediatric age, but the actual global incidence is thought to be underestimated, as many cases of postoperative respiratory distress may be misdiagnosed or unrecognized.1,2
PEAPE has a multifactorial etiology. The main triggering factor is secondary to upper airway obstruction caused by laryngospasm resulting from an exaggerated and prolonged laryngeal closure reflex, triggered by the mechanical stimuli of pharynx or larynx manipulation (like in the extubation procedure).1,3-5-8,9 The deep inspiratory effort against a closed glottis generates high negative intra-thoracic pressure transmitted to the lungs, leading to fluid transudation from pulmonary vessels to the interstitium and alveoli.1,3-5-8 At the same time, afterload and preload of the left ventricle increase worsening fluid transudation, finally resulting in the typical signs and symptoms of acute pulmonary edema.1,3,4,6 Moreover, pulmonary vasoconstriction caused by hypoxia and marked release of catecholamines associated with hypoxemia and hypercapnia (caused by upper airway obstruction) also contribute to this type of acute pulmonary edema.1,8
Well-developed thoracic and abdominal muscles are mentioned as risk factors for this complication, explaining its higher incidence in healthy young individuals, capable of generating very high intrathoracic pressure.1-3,5,6 Other factors may also contribute, including obesity, short neck, sleep apnea, nasopharyngeal pathology, and smoke, neither observed in the present case.1,3,5,6
In agreement with the present case, PEAPE mostly occurs immediately after tracheal extubation, with immediate onset of respiratory distress.1-3,6 However, delayed presentation (up to 24 hours post airway obstruction relief) has also been reported.1,2,4,6,7,10 The presence of tachypnea, tachycardia, dyspnea, intense cough, sometimes pink frothy bronchial secretions, progressive oxygen desaturation, and basal/widespread rales or fine crackles and ronchi on chest auscultation suggests PEAPE diagnosis in the appropriate setting, as in this case.2,4,5,7
This diagnosis requires a high index of suspicion, as the presentation mimics aspiration pneumonia, pulmonary thromboembolism, anaphylaxis, myocardial dysfunction, and other causes of pulmonary edema, including cardiogenic, opioid-induced, neurogenic, and iatrogenic fluid overload.1-5,7,10
As observed in this case, chest radiograph shows rapid bilateral changes compatible with pulmonary edema, including diffuse interstitial and alveolar infiltrates and should be performed to confirm the diagnosis and exclude other causes of postoperative acute respiratory distress, particularly aspiration pneumonia.1,2,4,5,7
In the present case, the patient’s past medical history, course in the operating room, with low fluid infusion volume, and clinical and radiological findings, together with cardiac assessment excluding cardiogenic etiology, were consistent with post-extubation acute pulmonary edema.
If promptly diagnosed and managed, most PEAPE cases resolve within 3-48 hours, as observed in this case.2,3,4,8,10 Treatment includes maintaining the airway and providing supplemental oxygen, with the addition of positive end-expiratory pressure or continuous positive airway pressure (guided by physical examination, pulse oximetry, and arterial blood gas determination), which significantly reduces increased breathing work and ventricular afterload and helps in alveoli recruitment 1-4 8,10 In severe cases, invasive mechanical ventilation may be necessary.2-4 Although diuretics are often used, their role in PEAPE treatment is unclear, and their use is thus controversial.4,7,10 Despite that, the present patient was successfully treated with furosemide, like in other similar previous reports, probably due to “direct” vascular effects occurring apart from its primary diuretic action, contributing to pulmonary edema resolution regardless of fluid balance.2,4,7,11 Elevated catecholamine levels are thought to accelerate the rate of alveolar fluid clearance in PEAPE.8 However, since vascular pressure may be high, diuresis is unlikely to be harmful (provided that vascular status and renal function are normal), and enhances pulmonary edema resolution, as in this case.8
PEAPE is an uncommon but relevant anesthesia-related emergency, which may worsen the prognosis of low-risk surgical procedures.3 This case highlights the importance of keeping a high degree of suspicion in children and adolescents presenting with signs of respiratory distress and hypoxia after general anesthesia, as prompt diagnosis and treatment are crucial for a favorable outcome.