A previously healthy 17-year-old male adolescent was admitted to the Pediatric Emergency Department due to a non-itchy progressive skin eruption with four days of evolution. He mentioned history of trauma on the elbows and right ankle one week earlier and reported odynophagia and low fever (axillary temperature of 37.6ºC) in the previous week, which solved with symptomatic treatment. Other symptoms or medications were denied. No family history of autoimmune diseases was reported.
On admission, crusty abrasion lesions were present on the patient’s elbows and right ankle. A well-defined erythematous plaque with adherent white scales was observed around skin lesions of the ankle (Figure 1). Several erythematous papular drop-like lesions, most of which with overlying scales, were observed on the trunk and limbs (Figures 2 and 3).
What is your diagnosis?

Figure 2 Erythematous papular drop-like lesions, most with overlying scales, on the trunk and lower limbs
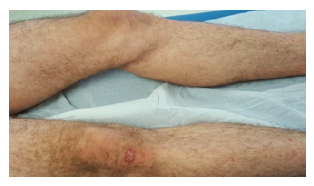
Figure 3 Erythematous papular drop-like lesions, most with overlying scales, on the trunk and lower limbs
Diagnosis
Guttate psoriasis secondary to trauma (Koebner phenomenon) and upper airway infection.
The adolescent was discharged with calcipotriol/betamethasone topic treatment once a day and a skin emollient and fully recovered within a few weeks. After one year of follow-up, he remains asymptomatic and without relapse.
Discussion
Guttate psoriasis is the second most common psoriasis variant in pediatric age, usually affecting patients older than five years.1-4 It typically presents with acute onset of numerous small, erythematous, scaly papules (“drop-like lesions”) and plaques with centripetal progression and symmetrical distribution. The trunk and proximal extremities are typically involved, although lesions may also occur in other locations, such as the scalp, hands, feet, and nails. The palms and soles are rarely affected.4 Pruritus may be present. Skin eruption may present as a new-onset disorder in patients with no previous history of psoriasis or as a new psoriasis presentation in patients with preexisting chronic plaque-type disease.5
The interplay between genetic and environmental factors seems to account for disease development. Positive family history may be present. Streptococcal upper airway infection is a major trigger of the condition, occurring in 56-85% of cases.4 Perianal streptococcal infection may also precede guttate psoriasis in children.6-7 The latency period between streptococcal infection and the appearance of skin lesions is typically two to three weeks. Multiple other infectious agents have been linked to guttate psoriasis, although less frequently than streptococcus. Drug therapy may sometimes precipitate a guttate-type flare. The most commonly implicated medications include lithium, beta-blockers, antimalarial drugs, nonsteroidal anti-inflammatory drugs, and biologic agents.4 Trauma is also an important trigger due to the Koebner phenomenon. In this entity, skin lesions appear at the injury site, with wound healing triggering hyperproliferative changes in the surrounding healthy skin that can lead to guttate psoriasis. Lesions usually appear 10-14 days after trauma. The Koebner phenomenon occurs in 50% of children with psoriasis.4,8
In the present case, both previous upper airway infection and trauma were present, which precluded the identification of the exact trigger and allowed to admit the existence of two environmental triggers.
In most cases, clinical history and physical examination are sufficient to diagnose the condition. Laboratory studies should only be required to rule out other diagnoses or identify the etiological agent. In challenging cases, a skin biopsy can be performed to support the diagnosis.
The differential diagnosis includes lichen planus, chronic lichenoides pityriasis, pityriasis rubra pilaris, pitiriasis rosea, and secondary syphilis.4
Guttate psoriasis may spontaneously remit, intermittently recur, or persist and progress to chronic plaque psoriasis.7,9-11 The course of the disease is unpredictable. Disease remission is the most common course in patients lacking a preceding history of psoriasis and typically occurs over the course of several weeks to a few months.1,7,9-11
First-line treatments include phototherapy and topical agents (corticosteroids and vitamin D analogs, such as calcipotriol, tacalcitol, or calcitriol).12,13 Topical agents may be used in monotherapy or combination and are usually able to control mild-to-moderate forms of the disease. Combined topical agents achieve more prolonged remission without rebound effect compared to corticosteroid monotherapy. Topical monotherapy or combined therapy should be used once to twice daily for around two weeks, although longer periods can be required. Low-potency corticosteroids are typically used on atrophy-prone sites, such as the face and intertriginous areas. Topical calcineurin inhibitors may alternatively be used in these thinner skin areas.14 Medium-to-high-potency corticosteroids are indicated for lesions on the trunk and extremities. Vitamin D analogs should be applied on the skin at night and cleared in the morning to avoid triggering sun hypersensitivity. Cutaneous irritation is the most common adverse effect of these agents, which should thus be avoided in the face and flexures.4 Phototherapy or even heliotherapy should be considered in cases of widespread lesions (when application of topical agents is unfeasible) or lesions refractory to topical therapy.4 Moderate-to-severe cases may require combining phototherapy and topical agents.4 Systemic immunomodulatory and immunosuppressive therapies used in chronic plaque psoriasis may also be attempted in patients with severe or persistent disease that fails to respond to first-line therapies.12,15 An emollient cream should always be used despite the selected therapy option.4 Patients with an active source of streptococcal infection should also be treated with antibiotic therapy.
This report highlights the importance of considering the clinical diagnosis of guttate psoriasis (a frequent psoriasis variant in pediatric ages) in cases of widespread skin eruption after trauma and/or infection, avoiding unnecessary exams.
















