Introduction
The new coronavirus disease (COVID-19) is an infectious condition caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was considered an international public health emergency by the World Health Organization (WHO) and classified as a global pandemic on March 11, 2020, highlighting the enormity of the viral outbreak.1
Despite the significant increase in both the incidence and prevalence of the condition, little is known about COVID-19 in the perinatal period. Limited data indicate that pregnancy may not be a risk factor for severe disease, and studies suggest that vertical transmission of the virus and transmission through breast milk is unlikely.2-4
However, concerns about viral transmission from infected mothers to babies prompted the development of restrictive policies in various settings, which included the delivery of babies through cesarean section, the immediate separation of mothers and newborns after birth, and avoiding early breastfeeding. (5-7
With the epidemiological data of the pandemic rapidly evolving, neonatologists need to continuously update management strategies for neonates born to mothers with confirmed or suspected COVID-19.
Our institution is a level III Neonatology Unit included in the maternity hospital of reference for the care of pregnant women with COVID-19 and their newborns in the central region of Portugal during the pandemic. As a member of the Baby-Friendly Hospital Initiative launched by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), it is our permanent concern to protect and support breastfeeding, and efforts were made during the pandemic toward this goal.
The aim of this study was to investigate how the adjustment of clinical practices to continuously evolving guidance from national and international institutions during the pandemic influenced the general health of babies born to infected mothers, particularly regarding breastfeeding.
Material and methods
A longitudinal study was conducted based on the registry of cases of infants born to mothers with confirmed SARS-CoV-2 infection during seven months (April-October 2020). All women admitted to our maternity ward were tested for SARS-CoV-2. Data were retrieved from routine perinatal obstetric and newborn medical records. After hospital discharge, the follow-up of the mother and infant was carried out during the first month through a weekly teleconsultation. Questions were asked about the type of feeding implemented, feeding difficulties, weight surveillance and evolution, medical appointments attended or scheduled (by general practitioners at a primary care center or pediatricians), de novo symptoms affecting the mother and/or baby (respiratory symptoms, fever, vomiting), and other types of concerns or difficulties. Medical support and advice regarding all these issues were provided. Informed consent was obtained from study participants, and all patient data were anonymized.
Management of infected mothers and their newborns
During the study period, different approaches were undertaken to adjust the institution´s clinical practices to the rapidly evolving guidance from national and international entities. Simultaneously, professionals had to deal with constraints in facility infrastructures and limitations in logistics and human resources.
The management of infected mother-neonate dyads varied according to three institution’s management phases throughout the study period.
In the first phase (April 1-24, 2020), immediately after birth, mothers and newborns were separated and referred to different hospital units. Puerpera were admitted to negative-pressure rooms at the COVID Unit of the main hospital. During hospital stay, they received a daily visit from an obstetric team composed of a doctor and nurse. Newborns were transferred to negative-pressure rooms in the Intensive Care Unit (ICU) of the Pediatric Hospital, only being discharged or readmitted to the maternity ward after two negative SARS-CoV-2 reverse transcription polymerase chain reaction (RT-PCR) tests performed at 24 and 48 hours of life, respectively, and no signs of disease.
In the second phase (April 24-May 10, 2020), mothers were still transferred to the Infectious Disease Unit of the main hospital, but newborns remained isolated in a regular room in the COVID area of the Neonatology Unit under the care of a nurse. If the newborn tested positive, he/she was transferred to a negative-pressure room in the ICU of the Pediatric Hospital.
In the third phase (after May 10), the option of mother and newborn cohabitation in a specific COVID area of the maternity ward under strict protective measures in cases of asymptomatic or poorly symptomatic mothers was discussed prior to delivery. Updated information of the potential risks and benefits of that option was provided to the mother, and informed consent was obtained.
Type of newborn feeding
In phases 1 and 2, mothers were encouraged to pump breast milk and instructed on how to stimulate and maintain the production of breast milk during separation from the newborn. During the admission period, the newborn was fed with infant formula. After home discharge of both mother and newborn, breastfeeding was encouraged as soon as the mother tested negative.
From phase 3, direct breastfeeding was encouraged and supported, with the alternative of the baby being fed by a nurse through a bottle with freshly expressed breast milk. After being duly informed, the mother signed an informed consent form and could choose the preferred feeding type. If the mother chose to directly breastfeed, she should wear a surgical mask and perform hand and breast hygiene prior to feeding. After breastfeeding, both the mother and baby should remain at least two meters apart, and the baby should be under the care of a nurse wearing full personal protective equipment (PPE). At discharge, information about infection prevention measures during breastfeeding and home care of the newborn was provided verbally and through informative leaflets to the family.
Some practices remained unchanged over the seven-month study period. These included the mode of delivery based on progression of labor and routine obstetric indications; use of full PPE by providers and nurses, and use of surgical masks by mothers during the entire course of labor and delivery in cases of mothers with confirmed and suspected COVID-19 infection; and discharge of the newborn only after his/her well-being, parenting competences, and a healthy caregiver (with SARS-CoV-2 testing done and negative result whenever possible) were assured.
Results
During the seven-month study period, 1362 pregnant women were admitted to our Neonatology Unit and tested for COVID-19 infection. Of these, 14 had a positive test result. Table 1 depicts the clinical characteristics of these women. All pregnant women were asymptomatic at the time of hospital admission, except (Case 11), who presented with mild symptoms (cough). All cases but one (Case 4) were term births. All SARS-CoV-2 tests performed to newborns at 24 and 48 hours of life were negative, and no newborn had symptoms during hospital admission or follow-up.
At mother-newborn dyad discharge, half (50%; 7/14) of neonates were under exclusive direct breastfeeding, and the other half were under infant formula. During the institution’s management phases 1 and 2, when mothers and newborns were separated during hospital admission, all neonates (6/6) were under infant formula. During phase 3, rooming-in and direct exclusive breastfeeding took place according to the mother’s wish and institution’s guidance, being maintained until discharge in 88% of cases (7/8). The only exception was Case 8, in which the mother had to be transferred to the ICU after hemorrhagic shock due to uterine atony, with a consequent longer time to discharge.
At one-month follow-up, 71% (10/14) of infants were being breastfed, 57% (8/14) exclusively, and 14% (2/14) in combination with infant formula supplementation. Among cases included in phases 1 and 2, all infants were breastfed at one-month follow-up, 67% of whom exclusively. The four cases which were under exclusive infant formula feeding at one-month follow-up comprised Case 8, in which breastfeeding was not possible due to the mother’s staying at the ICU, and three cases of newborns who were under breastfeeding during hospital admission but initiated infant formula supplementation after discharge due to failure to thrive and probable maternal hypogalactia. At one-month follow-up, no infant experienced relevant symptoms. All were under proper surveillance by general practitioners and nurses at the primary care center or by pediatricians.
Table 1 Clinical characteristics of mother-newborn dyads included in the study
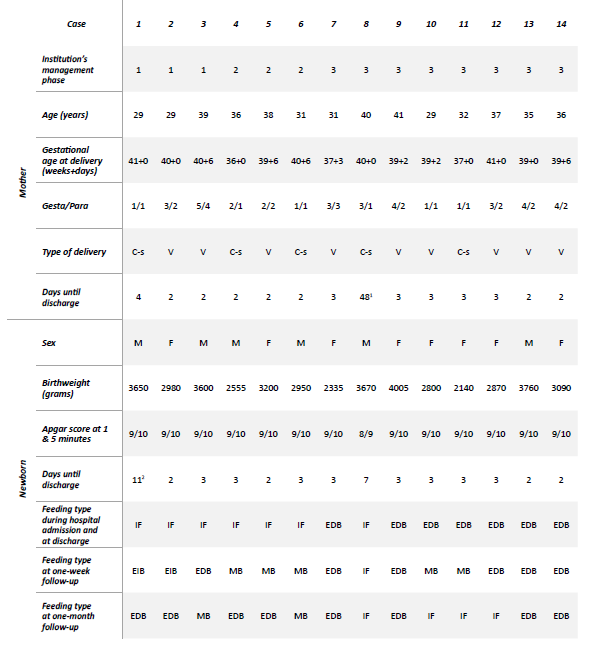
1Mother transferred to the Intensive Care Unit after hemorrhagic shock due to uterine atony; 2 Time taken to conclude SARS-CoV-2 testing of a large household (process carried out by the Public Health Department). Abbreviations: C-s, cesarean section; EDB, exclusive direct breastfeeding; EIB, exclusive indirect breastfeeding; F, female; IF, infant formula; M, male; MB, mixed breastfeeding (breastfeeding + infant formula); V, vaginal
Discussion
The COVID-19 pandemic has affected almost every aspect of life and posed challenges to the care of pregnant women and their infants. Long-supported and implemented perinatal practices acknowledged for their undisputed benefits (such as vaginal birth, rooming-in, and breastfeeding) were sometimes questioned and even threatened.
Lack of consistent data on the effects of COVID-19 on pregnancy and newborn health, as well as initially conflicting positions and disparities in recommendations from international experts and entities, led institutions ─ including our maternity hospital ─ to adopt different management practices within a short period of time.4-14 Furthermore, constraints in facility infrastructures and logistics and in human resources were relevant obstacles for some maternity hospitals.
At the beginning of the pandemic, with little yet known about the effects of COVID-19 in the perinatal period, some experts advocated the initial separation and isolation of the mother and child in different rooms after birth and recommended against breastfeeding as precautionary measures to minimize the risk of vertical transmission.5)-7) The Centres for Disease Control and Prevention (CDC) also recommended the separation of mothers and neonates as the first option to reduce the risk of vertical transmission of the virus.8 This position was also assumed by our institution during phases 1 and 2.
As evidence built, the continuous publication of studies suggested that the benefits of breastfeeding outweighed the risks of transmission of the infection from mothers to infants, leading several international entities to support breastfeeding and the non-separation of SARS-CoV-2-positive mothers and healthy babies.9-11 The World Health Organization (WHO), the United Nations Children’s Fund (UNICEF), and national guidelines recommended exclusive breastfeeding and excluded the option of separating mothers and neonates, with the concurrent adoption of infection prevention measures.12-14 Direct breastfeeding was the recommended first option for neonate feeding, followed by a second safe alternative of freshly expressed breast milk.4,9-11,14 This position was also adopted by our institution and has been in place since phase 3.
As a member of the Baby-Friendly Hospital Initiative launched by WHO and UNICEF, our Neonatology Unit sought to continue promoting and supporting breastfeeding throughout the pandemic, even during the period of mother-neonate separation. The rate of breastfeeding at discharge reported in this study (50%) can be explained by the separation of mothers and newborns during phases 1 and 2. In phase 3, exclusive breastfeeding at the time of discharge was reported in 88% of cases, which is in agreement with the most recent (unpublished) data of our institution from the first months of 2020, reporting exclusive breastfeeding in 82% of neonates born at the institution. At one-month follow-up, rates of breastfeeding (71%) and exclusive breastfeeding (57%) were below the 88% and 68% rates reported for infants from five to six weeks of age on a national report on breastfeeding, respectively.15 This fact possibly reflects the difficulties in assuring optimal breastfeeding support during the pandemic. However, the continuous support and information provided to mothers during hospital admission and regular teleconsultations after discharge might have had an important positive impact on the final outcome, particularly regarding the 100% rate of breastfeeding (although not exclusive) seen at one-month follow-up in cases of initial mother-neonate separation. Telephone follow-up consultations during the first month after discharge were also recommended by other authors.9,16
Conclusions
The COVID-19 pandemic had an impact on long-supported and implemented perinatal practices recognized for their outstanding benefits, including breastfeeding. Institutions had to continuously update management strategies for neonates born to mothers with confirmed or suspected COVID-19 infection according to national and international recommendations while dealing with logistic and infrastructure constraints. The authors believe that early and constant support and promotion of breastfeeding during hospital admission and after discharge are crucial to the success of this practice and stress the importance of supporting breastfeeding even during challenging times due to its unquestionable long-term benefits for the health of the mother and child.















