Introduction
The past two years have witnessed the most serious pandemic of the modern world, coronavirus 19 infection (COVID-19). COVID-19 is caused by the acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a single-stranded positive-sense RNA virus belonging to the genus Betacoronavirus.1,9,11 The disease was first described in Wuhan, China, in December 2019, rapidly spread globally, and one year later, in March 2021, more than 114 million cases and nearly 3 million deaths had been reported.12) Despite these numbers, children and adolescents account for a relatively small proportion of COVID-19 cases.18) The pediatric population is also less likely to experience severe disease, and most patients do not require hospital admission.12
COVID-19 clinical manifestations have evolved over these two years. Although patients typically present with fever and respiratory symptoms ─ like cough, dyspnea, and fatigue ─ that may progress to severe respiratory failure, gastrointestinal (GI) symptoms, such as vomiting, diarrhea, and even abdominal pain, have been increasingly reported, mainly in pediatric patients.1,2,11,12,18
Several studies have identified SARS-CoV-2 ribonucleic acid (RNA) in anal/rectal and stool samples from patients with COVID-19 disease, even after virus clearance from the upper respiratory tract, suggesting fecal-oral transmission.3-6,12 Some mechanisms have been described to explain how SARS-CoV-2 can interact with and damage the GI system. SARS-CoV-2 interacts with the membrane receptor of host cells through the spike protein, which mediates fusion between the virus and the cell membrane.12 In addition, the viral receptor angiotensin-converting enzyme 2 (ACE2) and the transmembrane protease serine 2 (TMPRSS2), crucial for viral invasion, have been shown to be expressed in GI epithelial cells.7,8,10,12) They are co-expressed in glandular cells of the gastric, duodenal, and rectal epithelium and in the enterocytes of the ileum and colon.12,13 After viral cellular infection, new virions are synthesized in the cytoplasm of GI cells and released in the tract, causing direct disruption of enterocytes and viral shedding in stools.12,14,15) These findings suggest that SARS-CoV-2 may have the ability to infect and replicate in the GI tract, causing GI symptoms, which may have important implications for disease management and transmission and for infection control.1,9,10,12
The pediatric population has important clinical manifestations, ranging from asymptomatic to mild symptomatic and severe, and GI symptoms have become increasingly important in this age group.1,12 GI symptoms may be the only manifestation of the disease (~10% of cases) and may also precede or follow other systemic symptoms.1,10,11) These manifestations include diarrhea (2-50%), anorexia (40-50%), vomiting (4-67%), nausea (1-30%), abdominal pain (2-6%), and GI bleeding (4-14%). Diarrhea and vomiting are the most common GI symptoms, having been reported as first symptoms of the disease.12,13,16)
The aim of this study was to investigate and compare the clinical features of COVID-19 disease in pediatric patients with and without GI involvement, and to investigate the correlation with disease severity and presence of GI manifestations.
Material and methods
A retrospective cohort study was conducted at a tertiary pediatric center. Data were collected from the electronic clinical records of children and adolescents under 18 years old diagnosed with COVID-19 between March 1, 2020 and September 31, 2021. COVID -19 cases were established through a positive real-time polymerase chain reaction (RT PCR) test. Cases of children diagnosed with multisystemic inflammatory syndrome in children (MIS-C) were excluded.
All children and adolescents admitted to the Emergency Department (ED) with probable SARS-CoV-2 infection suggested by a clinical or epidemiological link were screened for SARS-CoV-2 virus through a nasopharyngeal swab followed by RT-PCR testing. Suspicious cases presented one or more of the following symptoms: fever, cough, or respiratory distress; or fever plus one of the following: nausea, vomiting, diarrhea, or abdominal pain. In addition, children who underwent nasopharyngeal PCR testing for SARS-CoV-2 during hospital admission for other medical reasons or who underwent elective surgery, and children with chronic conditions followed at our hospital who were referred by their attending physician and tested positive for SARS-CoV-2 elsewhere were also considered. All children and adolescents with positive SARS-CoV-2 testing were included in the Portuguese epidemiological surveillance platform SINAVE and in the surveillance platform of Centro Materno Infantil do Norte (CMIN) of Centro Hospitalar Universitário do Porto (CMIN-CHPorto) and underwent daily clinical and epidemiological surveillance by telephone. Those who remained asymptomatic or had mild symptoms had daily telephone follow-up, while those who raised concerns with symptom worsening during follow-up were referred to the ED. The clinical records of all patients were assessed for demographic, clinical, laboratory, and therapy data. Data regarding age, gender, body mass index (BMI), chronic conditions, symptoms, need for medication or hospitalization, and severity of disease were retrieved. According to the BMI value obtained, all children and adolescents were assigned to one of three groups, as per World Health Organization (WHO) definition: normal weight, overweight (BMI >25 Kg/m2), or obesity (BMI >30 Kg/m2) 17. Serum results retrieved from patients’ analytical study were assessed, considering leukocytosis when leukocytes were higher than the values considered normal for age and sex and using the same rational for the remaining analytical parameters assessed. Patients were further divided into two groups according to GI symptoms: patients with GI symptoms (Group 1) and patients without GI symptoms (Groups 2). GI involvement was defined as the presence of at least one of the following symptoms: diarrhea, nausea, vomiting, abdominal pain, or GI bleeding.
The Statistical Package for the Social Science (SPSS), version 25 for MacOS was used for statistical analysis. Descriptive statistics was conducted for the global population and for Groups 1 and 2. Continuous data were presented as median and interquartile range (IQR), and categorical data as frequency and percentage. Regarding group comparisons, Student’s t-test was used for quantitative analysis and Chi-square test for qualitative analysis. P-values below 0.05 were considered statistically significant.
The study protocol was approved by the Ethics Committee of the study’s institution, and all data was kept blinded and confidential.
Results
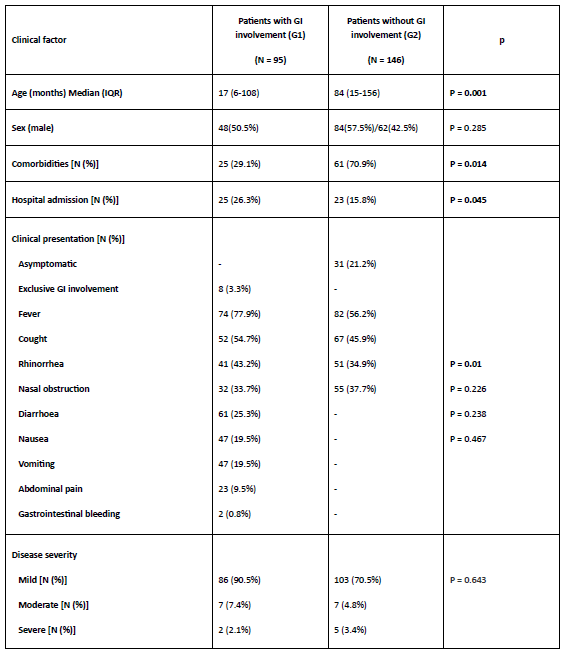
This study included 241 children with a median age of 48 months (IQR 10-144 months), 132 (54.7%) of whom boys and 109 (45.3%) girls. The baseline characteristics of the study cohort are shown in Table 1. Only 48 children (19.9%) were admitted to the hospital, with the remaining 193 being followed daily by telephone.
BMI estimate could not be done for 73 children. Among the remaining, 10 (6.0%) were overweight and 18 (7.4%) obese. Children with comorbidities accounted for 86 cases (35.7%), with comorbidities including lung disease (n=32, 13.2%), neurological disease (n=23, 9.5%), immune suppression (n=17, 7.0%), and gastrointestinal disease (n=8, 3.3%; Table 1).
Table 1 Baseline characteristics of the study population (n=241)
BMI, body mass index; IQR, interquartile range
Clinical assessment
At clinical presentation, 31 (12.8%) children were asymptomatic and 210 (87.2%) presented one or more symptoms. Table 2 summarizes the symptoms described by patients or caregivers at presentation in the global study sample.
Among symptomatic patients, 189 (78.4%) presented with mild disease, 14 (5.8%) with moderate disease, and 7 (2.9%) with severe disease.
The majority of symptomatic patients (n=146; 60.5%) presented no GI involvement, which was present in only 95 (39.4%) children and adolescents. Exclusive GI involvement was only reported in 8 (3.3%) patients.
The most frequent symptom in symptomatic patients was fever, present in 156 (64.7%) cases, followed by cough in 119 (49.4%) and rhinorrhea in 87 (36.1%) cases. In the group of patients with GI involvement, the most frequent symptom was diarrhea in 61 (25.3%) patients, followed by nausea and vomiting in 47 (19.5%) patients each.
The median duration of symptoms in the overall study population was 6 days (IQR 2-9 days).
Table 2 Clinical presentations of the study population
| Symptoms | Number [N (%)] |
| Fever | 156 (64.7%) |
| Cough | 119 (49.4%) |
| Rhinorrhea | 92 (38.2%) |
| Nasal Obstruction | 87 (36.1%) |
| Anorexia | 70 (29.0%) |
| Diarrhoea | 61 (25.3%) |
| Nausea | 47 (19.5%) |
| Vomiting | 47 (19.5%) |
| Abdominal pain | 23 (9.5%) |
| Gastrointestinal bleeding | 2 (0.8%) |
Analytical assessment
Table 3 depicts the analytical results of the study sample.
Blood count was only available for 51 (21.2%) patients, alanine transaminase (ALT), aspartate transaminase (AST), gamma glutamyl transferase (GGT), and alkaline phosphatase (AP) for 44 (18.3%) patients, and serum C-reactive protein (CRP) for 51 (21.2%) patients.
Leukocytosis was observed in 7 (2.9%) patients, with a median leukocyte count of 21580/l (IQR 19165-25625; minimum-maximum 15880-31140).
Regarding hepatic markers, the median AST value was 32.5 U/L (IQR 23.5-55.0; minimum- maximum 12.0-881.0) and the median ALT value was 19.5 U/L (IQR 13.0-36.0; minimum- maximum: 7.0-272.0). The median CRP was 6.2 mg/L (IQR 3.66-38.9; minimum-maximum 0.14- 331.0).
Table 3 Analytical assessment of the study population
| Laboratory testing | Median (IQR) |
| Leucocytes (n/µl) | 6990 (4990-13820) |
| Neutrophiles (n/µl) | 2660 (1409-5910) |
| Lymphocytes (n/µl) | 3190 (1780-4950) |
| ALT (U/L) | 32.5 (23.5-55.0) |
| AST (U/L) | 19.5 (13.0-36.0) |
| CRP (mg/L) | 6.2 (3.66-38.9) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; IQR, interquartile range
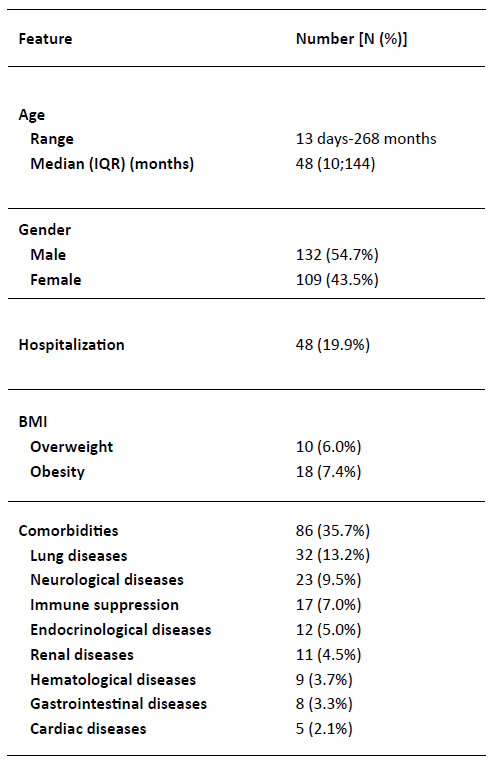
Comparison of patients with and without GI symptoms
Table 4 depicts the differences found between patients with (Group 1) and without (Group 2) GI symptoms at presentation, namely regarding hospital admission, clinical presentation, laboratory parameters, and disease severity. Patients with GI involvement at presentation were significantly younger than patients with no GI involvement (17 months vs. 84 months; p = 0.001). More children and adolescents with GI involvement at presentation required hospital admission compared to those without GI involvement (26.3% vs. 15.8%; p = 0.045). Clinically, the presence of fever was significantly associated with GI involvement at presentation, with more patients with this feature presenting with fever (77.9% vs. 56.2%; p=0.01). The remaining respiratory symptoms, including cough, rhinorrhea, and nasal obstruction, were not associated with GI involvement. Regarding analytical parameters, the presence of leukocytosis was exclusively observed in patients with GI involvement (Group 1). No significant association was found between analytical results or disease severity and presence of GI involvement at presentation.
Complications and management
Most patients in this study (n=193; 80.1%) did not require hospital admission and were followed daily by telephone.
Overall, 12 (5.0%) patients in this cohort developed complications during follow-up. Of these, 9 (9.4%) were from Group 1 and 3 (2.1%) from Group 2 (p=0.010), suggesting an association between the presence of GI symptoms at presentation and the development of post-acute illness complications. Among these were three cases of MIS-C.
Concerning the therapeutic approach, 198 (82.1%) patients only required symptomatic and supportive treatment, including antipyretics, intravenous fluids, or antiemetics. Antibiotic treatment was necessary in 20 (8.3%) children due to suspected or confirmed concomitant bacterial infection. All (100%) children and adolescents in Group 1 (with GI involvement) received symptomatic treatment, 2 of whom (2.1%) received antibiotic treatment for suspected bacterial over-infection.
Discussion
Despite the plethora of studies published about COVID-19, the knowledge of pediatric COVID-19 and its clinical spectrum remains limited. As already documented in some epidemiological studies, COVID-19 mainly manifests as a mild disease in the pediatric age group.17-19) This was confirmed in the present study, with most children and adolescents presenting with mild or even asymptomatic disease (78.4% and 12.8%, respectively). This diagnosis was established in the context of screening due to previous contacts or pre-surgery/hospital admission. Due to the low severity of the disease, most of these patients (82.1%) recovered with symptomatic treatment only, with only a small percentage requiring hospital admission (19.9%). Nevertheless, GI manifestations were significantly associated with a higher rate of hospital admissions.
The present cohort had a slight male preponderance, with no significant gender differences between groups of GI involvement. The median age of the cohort was 48 months, with the group of patients with GI manifestations having a lower median age compared with patients with no GI manifestations (17 vs. 84 months). Eighteen children (7.4%) were obese and 10 (6.0%) were overweight, but no association was found between these features and GI involvement. However, the literature describes a higher risk of severe disease in overweight children and adolescents, stating that excessive weight is an important risk factor for COVID-19 infection.21 Regarding comorbidities, these were present in 35.7% of patients in this study sample, with a statistically significant association found between the presence of comorbidities and the presence of GI symptoms.
The clinical presentation of COVID-19 in this study sample was rather unspecific, with the most common manifestations being fever and cough, present in 64.7% and 49.4% of pediatric patients, respectively. Anorexia was also found in a considerable proportion of patients (29.0%). COVID-19 GI manifestations were found to be three times more frequent in the pediatric population compared to what is reported in the literature for the adult population (39.4% vs. 12%).11,12,18 Diarrhea (25.3%) was the most frequently described GI symptom in this cohort, contrarily to other studies that indicate vomiting as the most frequent GI manifestation in pediatric age.18,21 In addition, two children in this cohort presented with lower GI bleeding as a COVID-19 manifestation. This study also found a significant association between GI involvement due to COVID-19 and the presence of fever and associated anorexia.
Regarding serum parameters, analytical study was only performed for 20% of patients in this study, which limits the conclusions that can be drawn from the results obtained. Despite this caveat, the median leukocyte count was found to be slightly higher in the group with versus without GI manifestations, albeit with no statistical significance. Leukocytosis was only observed in the group of patients with GI involvement. Also, no significant differences were found between the groups with and without GI involvement regarding serum values of hepatic enzymes and CRP.
GI manifestations including diarrhea, vomiting, abdominal pain, and GI bleeding may be the only form of presentation of COVID-19 in young children, and the evidence retrieved in this study adds relevant data that can contribute to adjust screening and public health policies in pediatric SARS-CoV-2 infection.
This study has the main limitations of its retrospective nature and small sample size. Reporting bias is another limitation that should be acknowledged, as young children may have symptoms that are not detected or reported to their parents. Despite these limitations, the results obtained mostly agree with previous reports in the literature.
Conclusions
In conclusion, despite the report that fever and cough are the primary symptoms found in COVID-19 infection, GI involvement may its major or only form of presentation in young children. Given the wide variety of clinical symptoms, clinicians should maintain a high index of suspicion for the infection in young infants presenting with GI symptoms, even in absence of fever. These data is relevant and can be used as rational to adjust screening and public health programs in pediatric SARS-CoV-2 infection.