Introduction
Neonatal mastitis (NM) is an uncommon infection of the breast tissue in neonates. Although it is equally common in both sexes in the first two weeks of life, the incidence peaks at three weeks and is more often in females.1) The difference in gender distribution is thought to be related to the longer duration of physiologic breast hypertrophy in females.2 In the case of physiologic breast hypertrophy, usually bilateral and symmetrical, the nipple discharge is milky rather than purulent and is characterized by the absence of polymorphonuclear cells or bacteria.3) NM is also more common in term infants, as premature infants have underdeveloped mammary glands. The infection usually evolves from the skin through the nipple to the breast parenchyma and rarely results from hematogenous infection.3 Most cases present unilaterally and are characterized by erythema, tenderness, heat, hypersensitivity, and breast induration.4 Rarely, NM may be associated with bacteremia and severe systemic symptoms, including fever, vomiting, and irritability, but otherwise systemic infection is uncommon in healthy happearing neonates.5 Extensive cellulitis, necrotizing fasciitis, and osteomyelitis have rarely been reported.6 The most common pathogen is Staphylococcus aureus (SA), which accounts for 83-88% of cases, followed by Escherichia coli, anaerobes, and group B Streptococcus.7,8) There is little evidence regarding the management of NM.2 The present study reviews the cases of NM diagnosed and treated in a neonatal intermediate care unit.
Methods
This was a retrospective review of cases with a diagnosis of NM in a neonatal intermediate care from July 2000 to June 2020, based on inflammatory signs such as redness, swelling, heat and induration of breast tissue, and purulent discharge.4,8) Retrieved data included maternal characteristics, including pregnancy complications, and neonatal characteristics, sex, gestational age, birth weight, physical examination, age at diagnosis, analytical workup (blood count, blood culture, culture of breast discharge, breast ultrasound), treatment (antibiotics, duration, treatment response, need for surgery), complications, and sequelae.
Neonates with NM are routinely admitted to the neonatal unit. However, in the presence of mild inflammatory signs, they may be discharged and re-evaluated in the outpatient setting − these cases were not included in this study.
Results
From July 2000 to June 2020, a total of 29.797 births were reported in the considered neonatal unit, corresponding to an average of 1,490 births/year. The annual incidence of unit admissions was 0.15, accounting for 225 admissions/year. During this period, ten cases of inpatient treatment of NM were identified, all corresponding to female neonates. The neonatal characteristics, laboratory findings, and treatment of these patients are depicted in Table 1. The median gestational age was 39 weeks and the mean age at diagnosis was 22 days. The median duration of symptoms before presentation to the Emergency Department was 2.2 days (range 1-4 days). All cases corresponded to unilateral NM. No relevant pregnancy or neonatal complications (including maternal skin or soft tissue infections) or cases of neonatal sepsis were reported.
Table 1 Characteristics of the ten female neonates with NM included in the study
| Neonate | Neonatal pathology | Age (days) | Blood culture | Breast exudate microculture | Antibiotic therapy | Treatment regimen | Treatment duration (days) |
| 1 | - | 14 | Sterile | - | Flucloxacillin | IV ->Oral | 10 |
| 2 | Hydronephrosis | 25 | Sterile | MRSA Vancomycin S | Flucloxacillin ->Vancomycin | IV | 16 |
| 3 | Goldenhar syndrome | 23 | Not performed | SA | Flucloxacillin | IV ->Oral | 10 |
| 4 | Persistent oval foramen | 9 | Sterile | - | A+G | IV | 10 |
| 5 | - | 28 | Sterile | S. epidermidis | Flucloxacillin | IV ->Oral | 10 |
| 6 | - | 26 | Sterile | - | A+G -> Flucloxacillin | IV ->Oral | 10 |
| 7 | Hydronephrosis | 30 | Not performed | SA | Flucloxacillin | IV ->Oral | 14 |
| 8 | Bronchiolitis | 33 | Sterile | SA | Flucloxacillin | IV | 12 |
| 9 | - | 24 | Sterile | MRSA Gentamicin S | A+G ->Gentamicin | IV | 16 |
| 10 | - | 30 | Not performed | SA | Flucloxacillin | Oral | 10 |
A+G: ampicillin + gentamicin; IV: intravenous; MRSA: multi-resistant Staphylococcus aureus; S: sensitive; SA: Staphylococcus aureus
All cases showed common inflammatory signs, including redness, induration, and tenderness. In addition, seven neonates had purulent breast drainage. No systemic signs such as fever, vomiting, feeding refusal, irritability, or lethargy were identified.
Complete blood count was obtained in all cases. Elevated white blood cell count (>15,000 cells/mm3) and positive C-reactive protein (>1.0 mg/dL) were observed in individual cases. Blood cultures performed in seven cases were negative.
Six cases of SA were isolated from chest discharge cultures, two of which were methicillin-resistant (MRSA). Staphylococcus epidermidis was isolated in one case. Urinalysis and lumbar puncture were not performed. Breast abscesses were found by ultrasound in four neonates: one drained spontaneously and the other three were surgically drained.
All cases were treated with antibiotics. Seven (70%) were initially treated with flucloxacillin and three (30%) with combined ampicillin and gentamicin. Intravenous treatment was started in nine cases (90%) and was switched to oral flucloxacillin after 2-10 days of clinical improvement and antibiogram results. Intravenous vancomycin and gentamicin were each used for 16 days in MRSA cases according to the antibiogram results. Overall, the median duration of treatment was 10 days (range 10-16 days). No local or systemic complications were observed.
Discussion
This study reviewed the cases of NM diagnosed in a neonatal unit over a period of 20 years. NM had an incidence of 0.002 in neonatal unit admissions and 0.0003 in hospital births, confirming a low incidence during the neonatal period. All NM cases occurred in female term neonates and were more common in the first three weeks of life, in line with previous observations.9) Neonatal pathology was not associated with the development of NM.10
The diagnosis of NM relies on careful clinical assessment, and systemic signs, although rare, should not be overlooked. There is little evidence to support a complete analytical evaluation in neonates presenting with only local signs. However, a complete blood count, blood culture, gram stain, and culture of purulent discharge may be helpful in determining the need for additional workup (i.e., lumbar puncture) and treatment (broad-spectrum antibiotics), especially if systemic manifestations are present.8) More than 50% of NM cases develop abscesses, which were observed in four cases (40%) in this study, and breast ultrasound may be helpful to confirm breast abscesses.5 Blood cultures were not performed in cases with subtle inflammatory signs.
There is currently no standard treatment for NM. Empirical treatment includes anti-staphylococcal antibiotics and antibiotics with gram-negative coverage, such as aminoglycosides or third-generation cephalosporins and vancomycin, and should take into account resistance profiles. In the present series, 90% of cases were initially treated with intravenous antibiotics after recommendation of empirical parenteral treatment pending results of specimen cultures.9) The recommended average treatment duration is 7-14 days and should be based on clinical response.3 In uncomplicated mastitis, transition to oral treatment can be made based on good clinical response, antibiotic susceptibility results, and continued monitoring. As observed in one neonate, primary oral treatment for ten days may also be safe and effective in cases with good oral compliance and in absence of systemic complications. However, intravenous treatment should be prioritized in cases of suspected MRSA infection or breast abscess.
Notably, SA was the most common pathogen found (60%) and flucloxacillin was the main treatment selected. All neonates had a favorable outcome regardless of the anti-staphylococcal antibiotic used. However, Gram stain and culture are useful to identify MRSA and guide further antibiotic adjustment.
Breast abscess is a possible complication of NM, and needle aspiration or surgical drainage may be required in the absence of spontaneous drainage.3 A report suggest that MRSA abscesses respond to isolated drainage.11 In this study, surgical drainage was used on admission in one case for an exuberant abscess and in two other cases as second-line treatment for a persistent abscess after 48 hours of antibiotic treatment. In all cases, the full course of antibiotics was completed and no recurrence was observed. In addition, no breast sequalae were observed after review of pediatric outpatient follow-up visits, although impaired breast development may occur in rare cases and should not be overlooked.9)
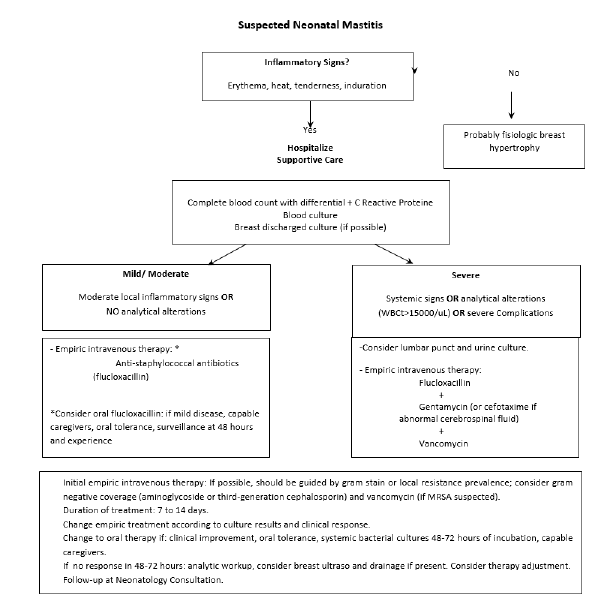
Based on the authors’ experience and literature review, a diagnostic and treatment algorithm for NM is proposed in Figure 1. Given the low incidence of NM, it is important to differentiate inflammatory signs from developmental breast hypertrophy, a physiologic condition with spontaneous resolution. Second, it is important to assess the severity and presence of systemic signs and symptoms. If only mild/moderate local inflammatory signs are observed, hospitalization is recommended. Treatment of NM should be based on supportive care (warm compresses), antimicrobial therapy, and abscess drainage (if possible). Analytical blood workup, blood cultures, and breast discharge culture should be obtained. Additional breast ultrasound may be helpful if the diagnosis is uncertain. Empirical therapy should include anti-staphylococcal coverage (penicillinase-resistant penicillin, as flucloxacillin) and consider Gram-negative coverage (aminoglycosides or third-generation cephalosporins) and vancomycin if MRSA colonization is suspected. Oral flucloxacillin may be considered. Although hospitalization is recommended, discharge may be considered in cases of competent caregivers, mild inflammatory signs, and if reassessment is possible within 48 hours. A change in empiric therapy may be considered at 48-72 hours only if cultures are sterile and significant clinical improvement is observed.
In neonates with severe systemic signs or symptoms, blood workup alterations (e.g., leukocytosis >15,000/uL), or severe complications (extensive cellulitis, necrotizing fasciitis, osteomyelitis, and shock), additional urine culture and lumbar puncture should be considered, as well as management of complications with empiric intravenous therapy starting with flucloxacillin, gentamicin, or cefotaxime (if abnormal cerebrospinal fluid) and vancomycin. Empiric therapy should be adjusted according to culture results and clinical response. In the absence of clinical improvement, breast ultrasound and surgical drainage (if possible) should be considered, as well as repetition of analytical study and therapy adjustment. The recommended treatment duration is seven to 14 days. Follow-up visit is recommended for all neonates to evaluate any breast sequelae.
Conclusion
This case series confirms that NM is a rare neonatal pathology that is more common in females, unilaterally, and in association with SA infection. All infants responded successfully to antibiotic treatment, even in the presence of complications such as abscesses. Prompt diagnosis and treatment are essential to ensure a favorable outcome, minimizing the risk of sepsis and breast complications.