Introduction
Feeding difficulties in early childhood are among the most common problems reported by parents.1) Up to 40% of typically developing children experience feeding difficulties, with the percentage rising to 80% in children with developmental delays.1),(2) These difficulties include refusal to eat, decreased appetite, food selectivity, difficulty self-regulating at mealtimes, fear of eating, and vomiting, among others.1)-(4) Feeding disorders are associated with problems later in life, such as behavioral disorders, cognitive deficits, and eating disorders.4
Identifying the etiology of the feeding problem can be challenging because it may reflect the child’s own characteristics and/or a dysfunctional dyadic or family relationship.5) The child may have difficulty self-regulating at mealtimes, difficulty with transitions and changes, sensory processing disorders, food refusal secondary to invasive medical procedures, or medical conditions that predispose to feeding problems.2,5) Because it involves an interaction between the caregiver and the child, feeding difficulties may also reflect a relational problem.5),(6 For young children, food goes beyond its nutritional value, as its quality affects the child’s sense of security, autonomy, and basic trust.5) Disturbed patterns of interaction between mother and child in cases of feeding and eating disorders were described as early as 1983 by Chatoor and colleagues.7) During mealtimes, there is an increasing conflict over autonomy and control between parent and child, exacerbated by the development of separation and individuation.8 In the case of feeding disorders, there are usually inconsistent and non-contingent responses from caregivers who fail to read the infant’s signals, leading to increased dyadic conflict and struggle for control.7),(8) There are also reports of disturbed triadic parent-child interactions in families of children with feeding disorders, with increased tension and negative affect, which impairs the children's self-regulatory abilities.9
Chatoor and colleagues proposed a diagnostic classification of feeding disorders divided into six categories: feeding disorder of state regulation, feeding disorder of reciprocity, infantile anorexia, sensory food aversion, feeding disorder associated with concurrent medical condition, and post-traumatic feeding disorder.4 Later, the authors described a classification of feeding difficulties using a systematic approach in which the child’s eating behavior is classified as restricted appetite, selective feeding, or fear of feeding, and the caregiver’s feeding style is classified as responsive, controlling, indulgent, or neglectful.3
In the Diagnostic and Statistical Manual of Mental Disorders, the various presentations of feeding disorders can be grouped into a single avoidant/restrictive feeding intake disorder.10 The Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0-5TM) defines three main diagnostic categories of eating disorders: overeating disorder, undereating disorder, and atypical eating disorder.1)
The aim of this study was to conduct a descriptive analysis of a sample of children under the age of six who were seen in a child psychiatry consultation for feeding and eating difficulties.
Methods
A retrospective descriptive analysis of sociodemographic and clinical data of children under six years of age with feeding or eating problems, evaluated at a first consultation in a child psychiatry unit of a tertiary hospital between January 2019 and May 2021, was performed. Children with previous child psychiatry follow-up and children with a diagnosis or suspected autism spectrum disorder were excluded from the study.
Patient data were retrieved from their medical records. Patient anonymity and confidentiality were maintained during data collection.
Sociodemographic data of the patients and their parents were collected and described. Several data on feeding patterns were assessed: child’s feeding behavior (food selectivity, difficulty with self-regulation at mealtimes, limited appetite, difficulty with transition to solid foods, vomiting or anticipatory gagging, fear of feeding, and chewing without swallowing), failure to thrive, prolonged mealtimes, disruptive and stressful mealtimes, nighttime feeding, breastfeeding, and duration of breastfeeding. Psychomotor development was also assessed using the Griffiths III Mental Development Scale.
Data on parental psychiatric history and parental history of food selectivity or eating disorders were also collected. The Graffar scale was used to stratify family social characteristics.
Attachment style was assessed using an adaptation (in three stages) of the Mary Ainsworth’s Strange Situation Procedure.11
The Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0-5™) was used to classify patients’ diagnosis.1 There are several diagnostic axes in this manual. Axis I refers to the clinical diagnosis, while Axis II is used to characterize the relational context. The latter has two parts: an assessment of the level of adaptation of the primary caregiving relationship(s) (Part A) and an assessment of the level of adaptation of the broader caregiving environment (Part B). The levels of adaptive functioning in Part A define ranges of relationship adaptation, and in Part B define ranges of qualities of the caregiving environment.1
Therapeutic interventions were examined and classified as mother-child psychotherapy, occupational therapy with sensory integration, speech therapy, day care, and parent counseling only. Follow-up status was described as improved, stabilized, or worsened.
Results
Of a total of 647 children assessed at a first visit to an early childhood psychiatry unit, 57 (8.81%) were classified as having feeding problems or difficulties, of whom 31 (54.4%) were male. The median age was 24.5 months. The age distribution is shown in Table 1. Children under 36 months were the most common group with feeding problems (80.6%), with the majority in the third year of life. A large percentage of children with feeding problems were under twelve months of age (n=14; 24.5%). In this age group, the most common feeding problems were difficulties with self-regulation at mealtimes (n=8), followed by parent-perceived decreased appetite (n=7), and vomiting or anticipatory gagging (n=6). Of the 14 children less than one year of age, 11 were singletons, eight were breastfed, and nine were fed at night. Five infants younger than 12 months had a diagnosis of gastroesophageal reflux disease. The most common diagnosis in this age group was undereating disorder (n=11). Regarding the relational context, nine children under one year of age had relationships with their primary caregiver that were considered strained to dysfunctional (Levels 2 and 3 on Axis II of the DC:0-5™). Child-parent psychotherapy was provided to nine children in this age group.
Regarding first consultations, 41 (71.9%) were from inpatient referrals, ten (17.5%) were from outpatient referrals, and only six (10.5%) were from primary care referrals.
The types of feeding problems identified in this cohort are described in Table 2. For 31 children (54.4%), parents reported more than one type of feeding problem. Eleven children (19.3%) were reported to have failure to thrive or weight loss. Twenty-five parents (43.9%) reported long mealtimes, and 31 (54.4%) found mealtimes to be disruptive or stressful. Nocturnal feeding was reported in 14 cases (24.6%).
Breastfeeding was reported in 47 cases (82.5%), with the majority of infants (56.5%) being breastfed until six months of age. Twenty-nine infants (50.9%) were cared for at home, 27 (47.4%) were in day care, nursery, or kindergarten, and one infant was institutionalized. Twenty-eight infants (49.1%) were singletons, 24 (42.1%) had one sibling, and five (8.8%) had two or more siblings.
Tables 3 and 4 show the main diagnoses registered in Axis I and II, respectively, based on DC:0-5TM. In Axis I, undereating disorders and sensory processing disorders were the two most prevalent diagnoses. Noteworthy, in Axis II, 49.1% of children exhibited patterns of interaction with the primary caregiver that were considered worrisome or disruptive (Level 2).
Regarding medical conditions, nine children (15.8%) had a diagnosis of gastroesophageal reflux disease, nine (15.8%) were born prematurely, two (3.5%) had a nasogastric tube for enteral nutrition, and five (8.8%) had a diagnosis of cow’s milk protein allergy. Of the total study population, 33 children were assessed using the Griffiths III Mental Development Scale. The results of this assessment is shown in Table 5.
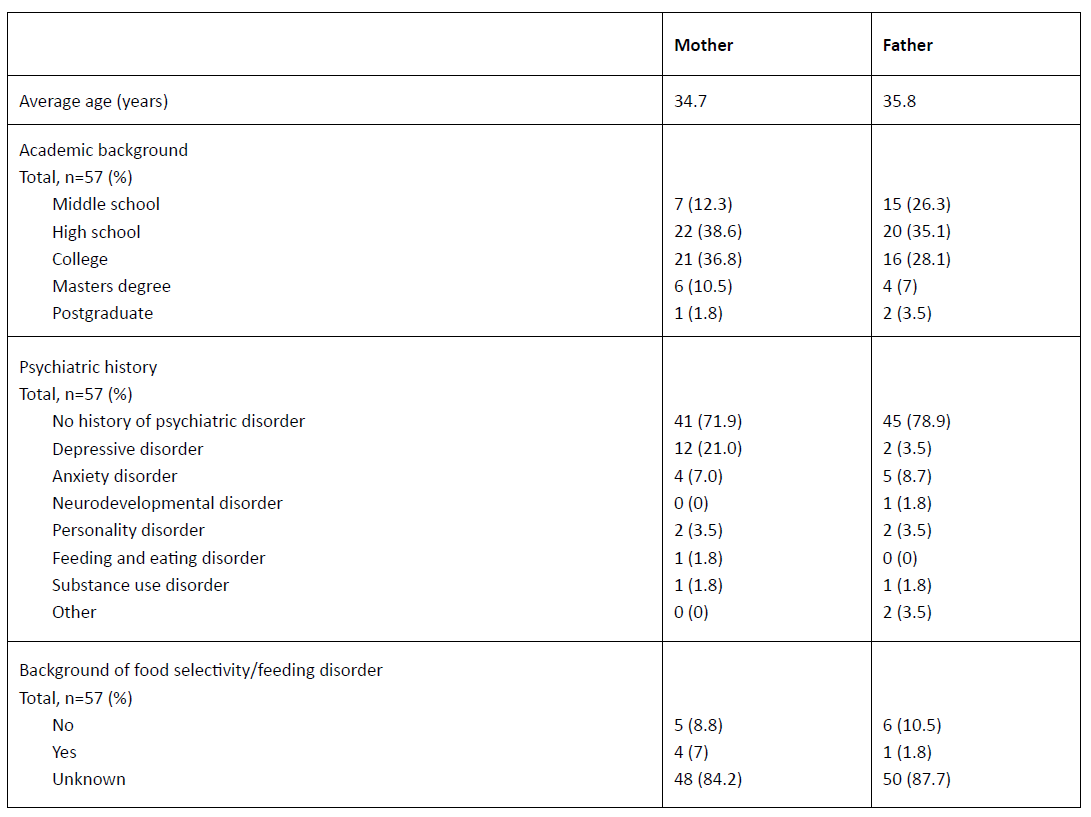
Table 6 depicts parental sociodemographic data, psychiatric history, and history of food selectivity or feeding disorders. The most common classification of family socioeconomic status was low/middle class (34.6%), followed by middle class (30.8%) according to the Graffar scale.
In 13 cases (22.8%) the attachment style was assessed using Mary Ainsworth’s Strange Situation Procedure. Five cases (38.5%) were classified as secure attachment and eight (61.5%) as insecure attachment. In the insecure attachment group, half of cases were classified as avoidant insecure attachment and the other half were classified as ambivalent/resistant insecure attachment.
The therapeutic interventions evaluated in this study were not mutually exclusive, as it was possible to use different interventions in the same case, depending on the symptomatology and relationship difficulties observed. Child-parent psychotherapy was the most common intervention, used in a total of 31 cases (54.4%). A total of 24 children (42.1%) were referred to occupational therapy, with sensory integration being the second most frequently recommended therapeutic intervention. Ten children (17.5%) were referred for speech therapy. Seven children (12.3%) were referred for nutritional pediatrics. Day hospital care was indicated in two cases (3.5%), and parent counseling and psychoeducation with no other intervention was provided in three cases (5.3%).
At follow-up, 38 children (67%) had a favorable outcome with the intervention provided, while 18 (31%) showed no change. Only one child (2%) had a worsened outcome.
Table 1 Age distribution of the study population
| Age | n (%)* |
| < 12 months | 14 (24.5) |
| 12 - 24 months | 13 (22.8) |
| 25 - 36 months | 19 (33.3) |
| 37 - 48 months | 4 (0.7) |
| > 48 months | 8 (0.14) |
*N=57
Table 2 Types of feeding problems in the study population
| Feeding problem | n (%)* |
| Food selectivity | 26 (45.6) |
| Difficulty in self-regulation during mealtimes | 25 (43.9) |
| Limited appetite | 19 (33.3) |
| Difficulty transitioning to solid foods | 16 (28.1) |
| Vomiting or anticipatory gagging | 15 (26.3) |
| Fear of feeding | 3 (5.3) |
| Chewing without swallowing | 2 (3.5) |
*N=57
Table 3 Axis I diagnosis according to the DC:0-5™
| Axis I diagnosis | n (%)* |
| Undereating disorder | 25 (43.4) |
| Sensory processing disorder | 23 (40.4) |
| Relationship-specific disorder of infancy/early childhood | 5 (8.8) |
| Global developmental delay | 5 (8.8) |
| Night waking disorder | 3 (5.3) |
| Adjustment disorder | 2 (3.5) |
| Other anxiety disorder of infancy/early childhood | 1 (1.8) |
| Separation anxiety disorder | 1 (1.8) |
| Other mood disorder of early childhood | 1 (1.8) |
| Developmental language disorder | 1 (1.8) |
*N=57. DC:0-5™, Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood
| Axis II diagnosis | Level 1 n (%)* | Level 2 n (%)* | Level 3 n (%)* | Level 4 n (%)* | Unknown n (%)* |
| Part A | 21 (36.8) | 28 (49.1) | 6 (10.5) | 0 (0) | 2 (3.5) |
| Part B | 27 (47.4) | 25 (43.9) | 3 (5.3) | 0 (0) | 2 (3.5) |
*N=57. DC:0-5™, Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. Part A - Caregiver-infant/young child relationship adaptation. Part B - Caregiving environment and infant/young child adaptation. Level 1 - Well-Adapted to Good-Enough Relationships/Environments. Level 2 - Strained to Concerning Relationships/Caregiving Environments. Level 3 - Compromised to Disturbed Relationships/Caregiving Environments. Level 4 - Disordered to Dangerous Relationships/ Caregiving Environments
Table 5 Development assessment according to the Griffiths III Mental Development Scale
| Scale | Under average (<88 points) n (%) | Average or above average (>88 points) n (%) |
| Locomotor scale | 8 (24.2) | 25 (75.8) |
| Personal-social | 12 (36.4) | 21 (63.6) |
| Language | 9 (27.3) | 24 (72.7) |
| Eye and hand coordination | 15 (45.4) | 18 (54.6) |
| Performance | 14 (42.4) | 19 (57.6) |
| Global quotient | 15 (45.4) | 18 (54.6) |
*N=33
Discussion
This study sought to characterize a population of children with feeding difficulties evaluated in a child psychiatry unit.
Approximately 25% of children are identified by parents as having feeding difficulties, with only 1-5% meeting criteria for a feeding disorder.3) Benjasuwantep et al. studied 402 healthy children aged one to four years and found a prevalence of feeding problems of 26.9%.12) In a study designed to investigate the prevalence of feeding disorders in typically developing young children, the authors used a parental questionnaire with high reliability and validity in detecting feeding problems (Behavioral Pediatrics Feeding Assessment Scale) and found that 8.2% had an abnormal total frequency score and 26.6% had an abnormal total problem score.13 Wright et al. conducted a cross-sectional analysis of 455 children from a population-based cohort at 30 months and found feeding difficulties in 20% of parent reports.15) This study found a prevalence of feeding difficulties of 8.81%, which is significantly lower than the above studies. These differences may be explained by the different methodologies used, as most studies used a questionnaire-based approach with cross-sectional analysis, unlike the present study. In addition, the present study focused on a clinical population and, to the authors’ knowledge, similar studies in the literature have been conducted only in normal and typically developing children.12)-(15) Furthermore, the definition of feeding difficulties/problems is highly variable and non-specific across studies, and some studies assess a population of children older than the one included in this study. This makes it difficult to compare results.
The results of this study reflect a low number of referrals of children with feeding difficulties to child psychiatry consultation. A high prevalence of children with feeding difficulties would be expected because these difficulties are among the most common referrals of infants and toddlers to child psychiatry units.5 The low number observed in this study may be explained by a lack of awareness among general practitioners and pediatricians that child psychiatry can provide effective assessment and intervention for childhood feeding and eating problems. Another explanation is that parents may tolerate certain disruptive eating behaviors in children without recognizing that they may constitute a disorder and therefore do not seek medical care. Mental health stigma regarding children and infants may be another reason for low referral of children with feeding problems for medical follow-up.
Children under 36 months were found to be the main group with feeding problems, with most occurring in the third year of life. During this period, the child’s increasing sense of autonomy and individuation often presents a challenge and a period of conflict for caregivers during mealtimes. In a study of 108 children by Benjasuwantep et al., feeding problems were most common in the second year of life.12) These discrepancies may be explained by differences in methodology and inclusion criteria between among studies, as children in the latter study were between one and four years of age.
A large percentage of children with feeding problems in this study (24.5%) were under twelve months of age. Feeding problems have been reported in 1-2% of infants under one year of age, which is a significantly lower percentage than that found in this study.4 These results may be explained by the fact that a significant proportion of cases included in the study were assessed in an Early Childhood Mental Health Unit consultation, a specialized outpatient tertiary referral service for infants under three years old. In addition, the first year of life is marked by a profound change in feeding patterns, with complementary foods introduced at around six months. This leads to changes in feeding routines and increased infant autonomy, which can be challenging for some parents to adjust to. If this process is not well coordinated between infant and caregiver, a feeding disorder may emerge.
More than half of children in this study had more than one feeding problem reported by their parents, making it difficult to differentiate which types of feeding problems may have the greatest impact. The most common type of feeding problem was food selectivity, identified in 45.6% of children, a percentage significantly higher than that reported in the literature.12),(14 This may be explained by the fact that this study was based on a clinical population with challenging feeding and behavioral problems. In a study of 959 healthy children aged 1.5 to 6 years, 25.1% were classified as picky eaters.14 However, this study excluded children with psychiatric or psychological disorders. In another study, highly selective feeding was the most common type of feeding problem, similar to the present study, found in 15.4% of children with feeding problems.12 Carruth et al. conducted a cross-sectional study of 3022 children without psychiatric or developmental problems and found that the percentage of children identified as picky eaters increased from 19% to 50% from four to 24 months.16) Physicians must acknowledge that food selectivity (or picky eating) is a very common and normal part of child development, but in some severe cases it can be an important cause of feeding difficulties and possible failure to meet adequate nutritional or energy needs.17 Benjasuwantep and colleagues described that energetic children with little interest in eating and limited appetite represented the second and third most common types of feeding problems, respectively, which is consistent with the present study’s findings.12 After food selectivity, difficulties in self-regulation at mealtimes and reduced appetite were the most common types of feeding problems. Overall, 33.3% of parents reported reduced appetite in their children, which is a significantly higher percentage than that found by Wright and colleagues in a healthy population (10.9%).15
Only 10% of cases were referred from primary care, highlighting the need for increased awareness of feeding difficulties in early childhood among primary care providers, which can be achieved through psychoeducational approaches among these professionals.
Almost 20% of the children assessed for feeding and eating difficulties had poor weight growth, highlighting the need for these cases to be assessed in a collaborative and multidisciplinary approach between child psychiatry and pediatrics.
One quarter of the children studied were fed at night. A higher prevalence of night feeding (79.6%) was found in a study of children with feeding problems.12) This feeding practice is very common among caregivers who are concerned that their child is not getting enough nutritional intake during the day. However, it has several consequences, such as the risk of early childhood obesity and decreased nighttime sleep duration.18),(19
Half of the population in this study did not attend day care or kindergarten. Since many feeding difficulties are related to disrupted parent-child dynamics, it is not surprising that 50% of children spent the entire day in the care of their parents.7)-(9
Prolonged mealtimes are common among children with feeding problems, as documented in the present and previous studies.12),(15 In this study, 43.9% of parents reported prolonged mealtimes, which is significantly higher than the 10.9% found by Wright and colleagues.15 However, that study was conducted with typically developing children and not in a clinical population such as the present one. Furthermore, in a study of children aged one to four years, those with feeding problems had mealtimes longer than 30 minutes compared to typically developing children, which is consistent with the findings of this study.12
Mealtimes are often perceived as stressful by parents, as shown in this study, where more than half of parents (54.4%) perceived mealtimes as disruptive. This is significantly higher than the 6.5% reported by Wright et al.,15 which again may be explained by differences in the study populations (clinical vs. non-clinical). Toddlers with feeding difficulties are perceived by caregivers as having more difficult temperamental characteristics, requiring more attention, and being more prone to negative affect.20 Differences in perceptions between mothers and fathers were not explored in the present study.
As expected, the two most common diagnoses in this study were undereating disorders (43.4%) and sensory processing disorders (40.4%). Up to 40% of caregivers report that their children have feeding problems, namely lack of interest or refusal to eat, food selectivity, slow feeding, and difficulty regulating their state during feeding.1),(2 These complaints are part of the criteria for undereating disorders.1 Sensory processing disorders are diagnosed when the infant or toddler exhibits behaviors that reflect alterations in sensory input regulation and interfere with daily functioning, such as at mealtimes.1) It has been described that children with sensory processing disorders, such as sensory over-responsivity disorder, may manifest severe feeding problems.1) Also, sensory processing difficulties are more commonly observed in young children with feeding problems, and there is an association between increased sensory sensitivity and food selectivity.20-25) Therefore, a high number of children with sensory processing disorders would be expected in this study.
The most common type of intervention was child-parent psychotherapy. Almost half of the children included in this study had patterns of interaction with their primary caregiver that were considered worrisome or disruptive, and in these cases, child-parent psychotherapy was a valuable intervention. This type of intervention is also used when there is no clear indication of a disturbed relationship, but there is evidence of worrisome aspects of the dyadic interaction that may lead to a troubled child-caregiver relationship. Feeding difficulties tend to reflect a problematic dyadic relationship, and therefore a relational approach needs to be incorporated into the management of feeding and eating disorders in early childhood.3
Children with apparent sensory processing difficulties were referred for assessment (and further intervention) by sensory integration occupational therapy. Of the population studied, 24 children (42.1%) were referred for this intervention, making it the second most common recommended therapeutic intervention. Many children with feeding difficulties have sensory processing problems that affect the child’s ability to process multiple sensory stimuli from food.21),(22) Indeed, there is a need for a multidisciplinary approach that includes sensory assessment of infants and toddlers with feeding difficulties.
One of this study’s main findings was that 21% of the mothers had a history of depressive disorder and 7% had a history of anxiety disorder. An association between maternal depression and anxiety and infant feeding difficulties has been described.5),(26 Chatoor et al. also pointed out that mothers who are depressed or anxious have more difficulty managing their child’s feeding difficulties at mealtimes.4
Assessment of attachment patterns was only performed in 13 cases in this study, with 61.5% classified as having insecure attachment. In previous studies by Chatoor and colleagues, infants with infantile anorexia had higher rates of insecure attachment, which may exacerbate feeding problems. However, feeding difficulties can also occur within securely attached child-parent dyads.6),(20 The literature also describes an association between insecure attachment and the development of eating disorders later in life.27-29
This study has several limitations. Being a retrospective and descriptive study based on clinical reports, it was not possible for the authors to perform a complete and individualized assessment of the cases included. The use of validated questionnaires would be helpful to provide more measurable and comparable data.13) It was also difficult to make valid comparisons between study results and those found in the literature because of the large variance in definitions used to characterize feeding difficulties, discrepancies in study methodologies and outcome measures, and different age ranges of participants in different studies. Therefore, conclusions regarding the prevalence of feeding difficulties should be drawn with caution.
A strength of the study is that it was based on a clinical population and, to the authors’ knowledge, is one of the few studies conducted in a clinical setting. Most studies on the prevalence of feeding problems in infants and toddlers are based on healthy and typically developing children.12)-(14
Conclusion
Although the estimated prevalence of children with feeding problems in this study was lower than that reported in the literature, it still represents a significant proportion of the cases referred to the child psychiatry unit in question. A multidisciplinary approach must always be considered, as feeding problems may have a relational, organic, or sensory processing etiology and may affect multiple domains of the child’s health and development. This work highlights the importance of early identification and intervention for children with feeding difficulties.
Authorship
Pedro Carvalho e Marques - Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing - original draft
Maria do Rosário Monteiro - Data curation; Formal analysis; Investigation
Márcia Rodrigues - Data curation; Formal analysis; Investigation
Graça Fernandes - Writing - review & editing
Vânia Martins - Writing - review & editing